Abstract
Background
Steroid-sparing drugs, such as cyclosporine, are recommended as treatment for children with frequently relapsing nephrotic syndrome (FRNS) and steroid-related toxicities. We recently reported a high rate of relapsing nephrotic syndrome 2 years after discontinuation of cyclosporine treatment, suggesting that long-term treatment is necessary. Cyclosporine-associated nephrotoxicity (CAN) is a potential side effect of long-term cyclosporine treatment.
Methods
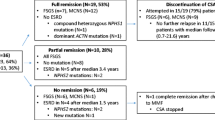
We retrospectively reviewed pediatric patients with FRNS treated with cyclosporine for ≥3 years at a single center between 1999 and 2012. The cyclosporine dose was adjusted to maintain the whole-blood cyclosporine trough level at 80–100 ng/ml for 6 months, at 60–80 ng/ml for 18 months, and then at around 50–60 ng/ml thereafter. Maintenance dose of prednisolone was not prescribed. CAN was graded in terms of arteriolar hyalinosis and the degree of interstitial fibrosis.
Results
Thirty-six children (28 males) were enrolled in the study. The median age at the start of long-term cyclosporine treatment was 9.4 years. The median duration of the longest period of cyclosporine treatment was 4.5 years. Most CAN cases were characterized by arteriolar hyalinosis. The frequency of CAN was positively correlated with the duration of cyclosporine treatment, with an odds ratio (95% confidence interval) for CAN of 3.84 (0.79–18.74) after 2–5 years and 6.60 (1.18–36.94) after >5 years of cyclosporine treatment (vs. 0–2 years).
Conclusions
Although the frequency of CAN was correlated with the duration of cyclosporine treatment in our pediatric patient population, most cases of CAN involved arteriolar hyalinosis. We conclude that long-term cyclosporine treatment is useful for treating FRNS in children, providing its dose is controlled and kidney biopsies are regularly performed.


Similar content being viewed by others
References
Fujinaga S, Ohtomo Y, Someya T, Shimizu T, Yamashiro Y, Kaneko K (2008) Is single-daily low- dose cyclosporine therapy really effective in children with idiopathic frequent-relapsing nephrotic syndrome? Clin Nephrol 69:84–89
Ishikura K, Ikeda M, Hattori S, Yoshikawa N, Sasaki S, Iijima K, Nakanishi K, Yata N, Honda M (2008) Effective and safe treatment with cyclosporine in nephrotic children: a prospective, randomized multicenter trial. Kidney Int 73:1167–1173
Ishikura K, Yoshikawa N, Hattori S, Sasaki S, Iijima K, Nakanishi K, Matsuyama T, Yata N, Ando T, Honda M ; for Japanese Study Group of Renal Disease in Children (2010) Treatment with microemulsified cyclosporine in children with frequently relapsing nephrotic syndrome. Nephrol Dial Transplant 25:3956–3962
Seikaly MG, Prashner H, Nolde-Hurlbert B, Browne R (2000) Long-term clinical and pathological effects of cyclosporin in children with nephrosis. Pediatr Nephrol 14:214–217
Tanaka H, Nakahata T, Ito E (2004) Single-dose daily administration of cyclosporin a for relapsing nephrotic syndrome. Pediatr Nephrol 19:1055–1058
Kano K, Nishikura K, Hoshi M, Yamada Y, Arisaka O (2001) Effectiveness of a second course of cyclophosphamide therapy in children with frequently relapsing nephrotic syndrome after cyclosporin a therapy. Clin Nephrol 55:424–425
Kyrieleis HA, Levtchenko EN, Wetzels JF (2007) Long-term outcome after cyclophosphamide treatment in children with steroid-dependent and frequently relapsing minimal change nephrotic syndrome. Am J Kidney Dis 49:592–597
Barletta GM, Smoyer WE, Bunchman TE, Flynn JT, Kershaw DB (2003) Use of mycophenolate mofetil in steroid-dependent and -resistant nephrotic syndrome. Pediatr Nephrol 18:833–837
Dorresteijn EM, Kist-van Holthe JE, Levtchenko EN, Nauta J, Hop WC, van der Heijden AJ (2008) Mycophenolate mofetil versus cyclosporine for remission maintenance in nephrotic syndrome. Pediatr Nephrol 2523:2013–2020
Gellermann J, Weber L, Pape L, Tönshoff B, Hoyer P, Querfeld U, Gesellschaft für Pädiatrische Nephrologie (GPN) (2013) Mycophenolate mofetil versus cyclosporin a in children with frequently relapsing nephrotic syndrome. J Am Soc Nephrol 24:1689–1697
Moudgil A, Bagga A, Jordan SC (2005) Mycophenolate mofetil therapy in frequently relapsing steroid-dependent and steroid-resistant nephrotic syndrome of childhood: current status and future directions. Pediatr Nephrol 20:1376–1381
Fujieda M, Ishihara M, Morita T, Hayashi A, Okada S, Ohta T, Sakano T, Wakiguchi H (2012) Effect of single-dose oral mizoribine pulse therapy twice per week for frequently relapsing steroid-dependent nephrotic syndrome. Clin Nephrol 78:40–46
Kawasaki Y, Hosoya M, Kobayashi S, Ohara S, Onishi N, Takahashi A, Isome M, Suzuki H (2005) Oral mizoribine pulse therapy for patients with steroid-resistant and frequently relapsing steroid-dependent nephrotic syndrome. Nephrol Dial Transplant 20:2243–2247
Fujinaga S, Sakuraya K, Yamada A, Urushihara Y, Ohtomo Y, Shimizu T (2015) Positive role of rituximab in switching from cyclosporine to mycophenolate mofetil for children with high-dose steroid- dependent nephrotic syndrome. Pediatr Nephrol 30:687–691
Iijima K, Sako M, Nozu K, Mori R, Tuchida N, Kamei K, Miura K, Aya K, Nakanishi K, Ohtomo Y, Takahashi S, Tanaka R, Kaito H, Nakamura H, Ishikura K, Ito S, Ohashi Y; Rituximab for Childhood-onset Refractory Nephrotic Syndrome (RCRNS) Study Group (2014) Rituximab for childhood-onset, complicated, frequently relapsing nephrotic syndrome or steroid-dependent nephrotic syndrome: a multicentre, double-blind, randomised, placebo-controlled trial. Lancet 384:1273–1281
Kronbichler A, Kerschbaum J, Fernandez-Fresnedo G, Hoxha E, Kurschat CE, Busch M, Bruchfeld A, Mayer G, Rudnicki M (2014) Rituximab treatment for relapsing minimal change disease and focal segmental glomerulosclerosis: a systematic review. Am J Nephrol 39:322–330
Hodson EM, Willis NS, Craig JC (2008) Non-corticosteroid treatment for nephrotic syndrome in children. Cochrane Database Syst Rev 2008(1):CD002290
Ishikura K, Matsumoto S, Sako M, Tsuruga K, Nakanishi K, Kamei K, Saito H, Fujinaga S, Hamasaki Y, Chikamoto H, Ohtsuka Y, Komatsu Y, Ohta T, Nagai T, Kaito H, Kondo S, Ikezumi Y, Tanaka S, Kaku Y, Iijima K; Japanese Society for Pediatric Nephrology (2015) Clinical practice guideline for pediatric idiopathic nephrotic syndrome 2013: medical therapy. Clin Exp Nephrol 19:6–33
Iijima K, Sako M, Oba MS, Ito S, Hataya H, Tanaka R, Ohwada Y, Kamei K, Ishikura K, Yata N, Nozu K, Honda M, Nakamura H, Nagata M, Ohashi Y, Nakanishi K, Yoshikawa N; Japanese Study Group of Kidney Disease in Children (2014) Cyclosporine C2 monitoring for the treatment of frequently relapsing nephrotic syndrome in children: a multicenter randomized phase II trial. Clin J Am Soc Nephrol 9:271–278
Ishikura K, Yoshikawa N, Nakazato H, Sasaki S, Iijima K, Nakanishi K, Matsuyama T, Ito S, Yata N, Ando T, Honda M; Japanese Study Group of Renal Disease in Children (2012) Two-year follow-up of a prospective clinical trial of cyclosporine for frequently relapsing nephrotic syndrome in children. Clin J Am Soc Nephrol 7:1576–1583
Moustafa BH, Tolba OA (2016) Immunosuppressive therapy in children with steroid-resistant, frequently-relapsing, and steroid-dependent idiopathic nephrotic syndrome: a single center experience. Elem Phys 8:2039–2047
Inoue Y, Iijima K, Nakamura H, Yoshikawa N (1999) Two-year cyclosporin treatment in children with steroid-dependent nephrotic syndrome. Pediatr Nephrol 13:33–38
El-Husseini A, El-Basuony F, Mahmoud I, Sheashaa H, Sabry A, Hassan R, Taha N, Hassan N, Sayed-Ahmad N, Sobh M (2005) Long-term effects of cyclosporine in children with idiopathic nephrotic syndrome: a single-centre experience. Nephrol Dial Transplant 20:2433–2438
Iijima K, Hamahira K, Tanaka R, Kobayashi A, Nozu K, Nakamura H, Yoshikawa N (2002) Risk factors for cyclosporine-induced tubulointerstitial lesions in children with minimal change nephrotic syndrome. Kidney Int 61:1801–1805
Fujinaga S, Kaneko K, Muto T, Ohtomo Y, Murakami H, Yamashiro Y (2006) Independent risk factors for chronic cyclosporine induced nephropathy in children with nephrotic syndrome. Arch Dis Child 91:666–670
Kengne-Wafo S, Massella L, Diomedi-Camassei F, Gianviti A, Vivarelli M, Greco M, Stringini GR, Emma F (2009) Risk factors for cyclosporin a nephrotoxicity in children with steroid-dependant nephrotic syndrome. Clin J Am Soc Nephrol 4:1409–1416
Fujinaga S, Endo A, Ohtomo Y, Ohtsuka Y, Shimizu T (2013) Uncertainty in management of childhood-onset idiopathic nephrotic syndrome: is the long-term prognosis really favorable? Pediatr Nephrol 28:2235–2238
International Study of Kidney Disease in Children (1982) Early identification of frequent relapsers among children with minimal change nephrotic syndrome a report of the international study of kidney disease in children. J Pediatr 101:514–518
Uemura O, Nagai T, Ishikura K, Ito S, Hataya H, Gotoh Y, Fujita N, Akioka Y, Kaneko T, Honda M (2014) Creatinine-based equation to estimate the glomerular filtration rate in Japanese children and adolescents with chronic kidney disease. Clin Exp Nephrol 18:626–633
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A, Collaborators developing the Japanese equation for estimated GFR (2009) Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 53:982–992
Solez K, Colvin RB, Racusen LC, Haas M, Sis B, Mengel M, Halloran PF, Baldwin W, Banfi G, Collins AB, Cosio F, David DS, Drachenberg C, Einecke G, Fogo AB, Gibson IW, Glotz D, Iskandar SS, Kraus E, Lerut E, Mannon RB, Mihatsch M, Nankivell BJ, Nickeleit V, Papadimitriou JC, Randhawa P, Regele H, Renaudin K, Roberts I, Seron D, Smith RN, Valente M (2008) Banff 07 classification of renal allograft pathology: updates and future directions. Am J Transplant 8:753–760
Hamahira K, Iijima K, Tanaka R, Nakamura H, Yoshikawa N (2001) Recovery from cyclosporine- associated arteriolopathy in childhood nephrotic syndrome. Pediatr Nephrol 16:723–727
Cattran DC, Alexopoulos E, Heering P, Hoyer PF, Johnston A, Meyrier A, Ponticelli C, Saito T, Choukroun G, Nachman P, Praga M, Yoshikawa N (2007) Cyclosporin in idiopathic glomerular disease associated with the nephrotic syndrome: workshop recommendations. Kidney Int 72:1429–1447
Acknowledgments
The authors wish to thank Nicholas Smith, PhD, of Edanz Group Japan K.K., for providing editorial support in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All clinical data and follow-up information were retrospectively obtained from the medical records. The design and execution of this study were in accordance with the ethical standards of the Declaration of Helsinki. The ethics committee at Tokyo Metropolitan Children’s Medical Center approved this study (approval number: 24–28).
Funding
Yuko Hamasaki has received a research grant from Novartis Pharma and a CPCF Research Grant, 2013.
Conflict of interest
Yuko Hamasaki has received research grant from Novartis Pharma, and lecture fees from Novartis Pharma and Astellas Pharma. Kenji Ishikura has received lecture fees from Novartis Pharma, Asahi Kasei Pharma, Chugai pharmaceutical Co. Ltd. and Zenyaku Kogyo. Kenji Ishikura has also received a consultant fee from Ono pharmaceutical. Masataka Honda has received lecture fees from Novartis Pharma, Takeda Pharmaceutical Co. Ltd., Chugai Pharmaceutical Co. Ltd., Zenyaku Kogyo, Pfizer Japan and Asahi Kasei Pharma. Riku Hamada has received lecture fees from Chugai Pharmaceutical Co. Ltd. Takashi Ando has received consultancy fees for statistical analyses from Asahi Kasei Pharma. The other authors have no potential conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Hamasaki, Y., Komaki, F., Ishikura, K. et al. Nephrotoxicity in children with frequently relapsing nephrotic syndrome receiving long-term cyclosporine treatment. Pediatr Nephrol 32, 1383–1390 (2017). https://doi.org/10.1007/s00467-017-3641-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-017-3641-4