Abstract
Background
Shiga-toxin-producing Escherichia coli (STEC)-associated hemolytic-uremic syndrome (HUS) is a major cause of acute kidney injury (AKI), especially in children. Its long-term outcome with respect to endothelial damage remains largely elusive.
Methods
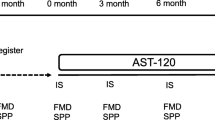
This was a cross-sectional study in 26 children who had suffered from STEC-HUS in the past and achieved a complete recovery of renal function (eGFR >90 ml/min/1.73 m2). Skin microcirculation after local heating was assessed by laser Doppler fluximetry, carotid-femoral pulse wave velocity (PWV), carotid intima media thickness (cIMT), 24-h ambulatory blood pressure, and angiopoietin (Ang) 1 and 2 serum levels after a median follow-up period of 6.1 years. The results were compared to those of healthy controls.
Results
All patients were normotensive, mean eGFR was 102 (range 91–154) ml/min/1.73 m2, and 13 of the 26 patients showed albuminuria. Endothelial dysfunction was present in 13 patients, and the mean serum Ang2/Ang1 ratio was increased compared to healthy children (each p < 0.05). In contrast, mean values for PWV and cIMT in the patients did not differ from those of the controls. Endothelial dysfunction was significantly associated with younger age at STEC-HUS manifestation, time after HUS, and presence of albuminuria.
Conclusion
The results of this study highlight the need for long-term follow-up of STEC-HUS patients even after complete recovery of eGFR and lack of hypertension with respect to microvascular damage.




Similar content being viewed by others
References
Mele C, Remuzzi G, Noris M (2014) Hemolytic uremic syndrome. Semin Immunopathol 36:399–420
Page A, Tarr P, Watkins S, Rajwans N, Petruzziello Pellegrini T, Marsden P, Kain K, Liles WC (2013) Dysregulation of angiopoietin 1 and 2 in escherichia coli O157:H7 infection and the hemolytic-uremic syndrome. J Infect Dis 208:929–933
Gagnadoux MF, Habib R, Gubler MC, Bacri JL, Broyer M (1996) Long-term (15–25 years) outcome of childhood hemolytic-uremic syndrome. Clin Nephrol 46:39–41
Garg AX, Suri RS, Barrowman N, Rehman F, Matsell D, Rosas-Arellano MP, Salvadori M, Haynes RB, Clark WF (2003) Long-term renal prognosis of diarrhea-associated hemolytic uremic syndrome: a systematic review, meta-analysis, and meta-regression. JAMA 290:1360–1370
Martín Navarro J, Petkov Stoyanov V, Gutiérrez Sánchez MJ, Justo Ávila P, Díaz Díaz D (2013) Long-term renal prognosis of typical haemolytic-uraemic syndrome suffered in infancy. Nefrologia 33:433–435
Spinale J, Ruebner R, Copelovitch L, Kaplan B (2013) Long-term outcomes of Shiga toxin hemolytic uremic syndrome. Pediatr Nephrol 28:2097–2105
Vikse BE, Irgens LM, Leivestad T, Skjaerven R, Iversen BM (2008) Preeclampsia and the risk of end-stage renal disease. N Engl J Med 359:800–809
Orabona R, Sciatti E, Vizzardi E, Bonadei I, Valcamonico A, Metra M, Frusca T (2017) Endothelial dysfunction and vascular stiffness in women with a previous pregnancy complicated by early or late pre-eclampsia. Ultrasound Obstet Gynecol. doi:10.1002/uog.15893
Heimhalt-El Hamriti M, Schreiver C, Noerenberg A, Scheffler J, Jacoby U, Haffner D, Fischer D (2013) Impaired skin microcirculation in paediatric patients with type 1 diabetes mellitus. Cardiovasc Diabetol 12:115
Fischer D, Schreiver C, Heimhalt M, Noerenberg A, Haffner D (2012) Pediatric reference values of carotid-femoral pulse wave velocity determined with an oscillometric device. J Hypertens 30:2159–2167
Doyon A, Kracht D, Bayazit AK, Deveci M, Duzova A, Krmar RT, Litwin M, Niemirska A, Oguz B, Schmidt BM, Sozeri B, Querfeld U, Melk A, Schaefer F, Wuhl E, 4C Study Consortium (2013) Carotid artery intima-media thickness and distensibility in children and adolescents: Reference values and role of body dimensions. Hypertension 62:550–556
Shroff RC, Price KL, Kolatsi-Joannou M, Todd AF, Wells D, Deanfield J, Johnson RJ, Rees L, Woolf AS, Long DA (2013) Circulating angiopoietin-2 is a marker for early cardiovascular disease in children on chronic dialysis. PLoS One 8:e56273
Neuhauser HK, Thamm M, Ellert U, Hense HW, Rosario AS (2011) Blood pressure percentiles by age and height from nonoverweight children and adolescents in Germany. Pediatrics 127:e978–e988
Wuhl E, Witte K, Soergel M, Mehls O, Schaefer F, German Working Group on Pediatric Hypertension (2002) Distribution of 24-h ambulatory blood pressure in children: normalized reference values and role of body dimensions. J Hypertens 20:1995–2007
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL (2009) New equations to estimate GFR in children with CKD. J Am Soc Nephrol 20:629–637
Pollack MM, Ruttimann UE, Getson PR (1988) Pediatric risk of mortality (PRISM) score. Crit Care Med 16:1110–1116
Scheiring J, Rosales A, Zimmerhackl L (2010) Clinical practice. today’s understanding of the haemolytic uraemic syndrome. Eur J Pediatr 169:7–13
Nester C (2013) Multifaceted hemolytic uremic syndrome in pediatrics. Blood Purif 35:86–92
Rosales A, Hofer J, Zimmerhackl LB, Jungraithmayr TC, Riedl M, Giner T, Strasak A, Orth-Holler D, Wurzner R, Karch H, German–Austrian HUS Study Group (2012) Need for long-term follow-up in enterohemorrhagic Escherichia coli-associated hemolytic uremic syndrome due to late-emerging sequelae. Clin Infect Dis 54:1413–1421
Tonshoff B, Sammet A, Sanden I, Mehls O, Waldherr R, Scharer K (1994) Outcome and prognostic determinants in the hemolytic uremic syndrome of children. Nephron 68:63–70
Roustit M, Cracowski JL (2012) Non-invasive assessment of skin microvascular function in humans: an insight into methods. Microcirculation 19:47–64
Khan F, Elhadd TA, Greene SA, Belch JJ (2000) Impaired skin microvascular function in children, adolescents, and young adults with type 1 diabetes. Diabetes Care 23:215–220
Cracowski JL, Minson CT, Salvat-Melis M, Halliwill JR (2006) Methodological issues in the assessment of skin microvascular endothelial function in humans. Trends Pharmacol Sci 27:503–508
Cracowski JL, Roustit M (2015) Current methods to assess human cutaneous blood flow. an updated focus on laser based-techniques. Microcirculation 23:337–344
Roustit M, Cracowski JL (2013) Assessment of endothelial and neurovascular function in human skin microcirculation. Trends Pharmacol Sci 34:373–384
Minson CT (2010) Thermal provocation to evaluate microvascular reactivity in human skin. J Appl Physiol (1985) 109:1239–1246
Bartz SK, Caldas MC, Tomsa A, Krishnamurthy R, Bacha F (2015) Urine albumin-to-creatinine ratio: a marker of early endothelial dysfunction in youth. J Clin Endocrinol Metab 100:3393–3399
Lin CY, Huang SM (2016) Childhood albuminuria and chronic kidney disease is associated with mortality and end-stage renal disease. Pediatr Neonatol 57:280–287
Garg AX, Salvadori M, Okell JM, Thiessen-Philbrook HR, Suri RS, Filler G, Moist L, Matsell D, Clark WF (2008) Albuminuria and estimated GFR 5 years after Escherichia coli O157 hemolytic uremic syndrome: an update. Am J Kidney Dis 51:435–444
Fitzpatrick MM, Shah V, Trompeter RS, Dillon MJ, Barratt TM (1991) Long term renal outcome of childhood haemolytic uraemic syndrome. BMJ 303:489–492
Bar J, Kaplan B, Wittenberg C, Erman A, Boner G, Ben-Rafael Z, Hod M (1999) Microalbuminuria after pregnancy complicated by pre-eclampsia. Nephrol Dial Transplant 14:1129–1132
Shahbazian N, Shahbazian H, Ehsanpour A, Aref A, Gharibzadeh S (2011) Hypertension and microalbuminuria 5 years after pregnancies complicated by pre-eclampsia. Iran J Kidney Dis 5:324–327
Kim KT, Choi HH, Steinmetz MO, Maco B, Kammerer RA, Ahn SY, Kim HZ, Lee GM, Koh GY (2005) Oligomerization and multimerization are critical for angiopoietin-1 to bind and phosphorylate Tie2. J Biol Chem 280:20126–20131
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the local ethics committee and conducted in accordance with the Helsinki Declaration. Patients and/or their parents gave written and informed consent for participating in the study.
Conflict of interest
The authors declare no conflict of interest.
Funding
This study was supported by the Jackstädt-Foundation, Wuppertal, Germany.
Additional information
Martin Kreuzer and Laura Sollmann contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Table S1
(DOCX 12 kb)
Rights and permissions
About this article
Cite this article
Kreuzer, M., Sollmann, L., Ruben, S. et al. Endothelial dysfunction during long-term follow-up in children with STEC hemolytic-uremic syndrome. Pediatr Nephrol 32, 1005–1011 (2017). https://doi.org/10.1007/s00467-016-3574-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-016-3574-3