Abstract
Renal replacement therapy (RRT) is the most important supportive measure used in the management of acute kidney injury (AKI). Peritoneal dialysis (PD) is a safe, simple and inexpensive procedure and has been used in pediatric AKI patients, ranging from neonates to adolescents. It is the modality of choice for RRT in developing countries with cost constraints and limited resources. However, its use has declined with the availability of newer types of extracorporeal modalities for RRT in the developed world. Much controversy exists regarding the dosing and adequacy of PD in the management of AKI. Data in infants and children have shown that PD can provide adequate clearance, ultrafiltration and correction of metabolic abnormalities even in those who are critically ill. Although there are no prospective studies in children, data from retrospective studies reveal no differences in mortality rates between different modalities of RRT. In this review, we discuss the advantages and limitations of PD, indications for acute PD, strategies to improve the efficiency of acute PD and outcomes of PD in children with AKI.
Similar content being viewed by others
Introduction
Renal replacement therapy (RRT) is often required in the management of children with acute kidney injury (AKI), especially in critically ill children [1–3]. The different options for RRT have expanded from peritoneal dialysis (PD) and intermittent hemodialysis (HD) to continuous RRT (CRRT; continuous venovenous hemodialysis/hemofiltration/hemodiafiltration), slow low-efficiency dialysis and slow continuous ultrafiltration. PD has been successfully used to treat AKI across all age groups, including neonates following open heart surgery for congenital heart disease, in critically ill children with multi-organ failure and shock, infection and sepsis and following natural disasters, particularly in regions that are remote and have poor infrastructure [4–8]. It remains one of the most common RRT modalities in AKI in developing countries [9–11]. However, despite PD being a common RRT modality in the management of children with AKI, the choices of catheters, treatment regimens and dosing are not standardized due to limited evidence. Recently, the International Society of Peritoneal Dialysis has published guidelines to help standardize clinical practice [12]. In this review we discuss the advantages and limitations of PD, indications for acute PD, strategies to improve the efficiency of acute PD and outcomes of PD in children with AKI.
Advantages of acute PD
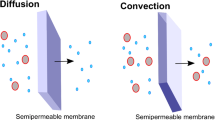
Peritoneal dialysis offers several advantages over other forms of RRT in children. First, this RRT modality is particularly suitable for children as the peritoneal surface area of pediatric patients is greater than that of adults (per unit weight), leading to more efficient solute clearance as compared to PD in adults [13]. Second, PD is a dynamic dialysis process which is more physiological and less pro-inflammatory than HD because the natural biocompatible peritoneal membrane is used as the dialyzer [14]. Third, cardiovascular tolerance is excellent as the gradual and continuous nature of solute and fluid removal during PD permits large volumes of ultrafiltration without causing hemodynamic instability [15, 16]. Finally, the peritoneal membrane has large pores which allow clearance of higher molecular weight substances as compared to HD; this may provide a potential advantage over conventional HD and filtration in patients with sepsis as it allows removal of toxic cytokines [17].
PD is technically simple and can therefore be performed with minimal infrastructural support and without an “intensive care unit (ICU) environment.” This attribute not only makes PD a lifesaving procedure in regions with poor infrastructure and lack of trained staff, but also in places affected by calamities where HD cannot be used due to the destruction of infrastructure, disruption of power and limited accessibility to clean water [18, 19]. The financial cost of providing PD may be as much as three- to fivefold less than that of providing HD or CRRT, making the former a more viable RRT modality in developing countries [20, 21]. PD can be a good choice in critically ill children with shock, multi-organ failure and coagulopathy. It is also a useful modality in newborns, including babies weighing <1000 g and infants in whom obtaining a vascular access for extracorporeal therapy can be very challenging [22, 23]. The dialysate which contains dextrose can also act as a source of supplemental calories for the patient undergoing PD, especially infants for whom hypoglycemia with fluid restriction may be a problem [24]. The continuous ultrafiltration by PD also allows for adequate nutrition by creating more space for fluid administration.
Limitations associated with acute PD
There are several limitations associated with acute PD. PD requires an intact peritoneal cavity and hence is relatively contraindicated in children with recent abdominal surgeries, abdominal cellulites, inguinal hernia, diaphragmatic hernia, paralytic ileus and peritonitis [25]. The ultrafiltration and solute removal is unpredictable, hence controlled ultrafiltration and precise fluid balance cannot be obtained with PD. Consequently, PD is not an ideal choice in critically ill children with multi-organ dysfunction who require meticulous management of volume status in addition to the removal of uremic toxins in order to maintain hemodynamic stability.
Poor ultrafiltration is another concern, especially in newborns and critically ill infants on high ventilator settings due to inability to increase the dwell to the desired volume, as this will increase intra-abdominal pressure and interfere with respiratory mechanics, with worsening of symptoms [26, 27]. In addition, many of these critically ill children are in severe shock and may have decreased splanchnic perfusion due to vasoconstriction of the mesenteric vessels, which also contributes to the poor ultrafiltration. Although peritoneal access can be obtained at the bedside percutaneously, allowing rapid initiation of therapy, the slow and gradual nature of PD with unpredictable ultrafiltration may result in a slower correction of life-threatening hyperkalemia or severe acute pulmonary edema. The clearance of small solutes is slower with acute PD as compared with a 4-h hemodialysis session or CRRT [28, 29], with the potential to result in inadequate clearances in hypercatabolic patients. Slow clearance of small solutes also makes PD less effective than HD or CRRT in children with inborn errors of metabolism (IEM), such as hyperammonemia where the neurological outcome is correlated with the rapidity of normalization of urea [30, 31]. In these patients, CRRT or HD, both of which permit more efficient ammonium removal, are recommended as the modality of choice during the acute phase [32, 33]. The use of PD may be a reasonable option until extracorporeal therapy can be commenced or when other forms of RRT are not available [34]. In their analysis of 45 neonates who underwent extracorporeal dialysis (ECD) or PD for hyperammonemia secondary to IEM, Picca et al. observed that the initiation of PD at an average of 10 h after IEM diagnosis versus initiation of ECD 20 h after the onset of hyperammonemia resulted in no difference in the short-term outcome of these patients [35]. In certain clinical situations, such as rapidly progressive glomerulonephritis and acute liver failure, where dialysis is often combined with plasma exchange (PE) or immunoadsorption, HD is preferred over PD. Over and above from the convenience of using the same access, the combined procedure of HD and PE in tandem or sequentially allows for a more efficient treatment [36, 37].
Mechanical complications associated with PD include leaks, catheter displacement, catheter obstruction and hernias. These complications lead to poor drainage of the dialysis fluid which in turn impacts the overall efficiency of dialysis. Dialysate leakage may occur around the catheter, especially when large fill volumes are used. Peri-catheter leakage can be prevented by using a lower dwell volume and tightly secured purse string sutures at the site of entrance of the catheter into the peritoneal cavity (for rigid catheters) and by precisely placing the catheter cuffs. Fibrin glue has been successfully used for the treatment of peritoneal dialysate leakage in infants and small children on PD [38]. Dialysate may also leak into the pleural space, through the pleuro-peritoneal channels, resulting in hydrothorax. Severe cases may require cessation of PD and surgical closure of the communication or pleurodesis. Catheter obstruction is usually due to kinking, omental wrapping or displacement of the catheter or to the formation of fibrin clot. The risks of catheter displacement/malposition, peri-catheter leakage and catheter obstruction are much lower with the use of Tenckhoff catheters as compared to rigid stylet catheters [39–41].
Serious complications, such as bladder or bowel perforation, are rare and mostly seen with the use of a rigid catheter. Hence it is important to ensure that the bladder is completely drained prior to the procedure and that a good fluid reservoir is achieved prior to insertion of the catheter. Bowel perforation is manifested by severe abdominal pain and leak of intestinal contents and may require surgical repair in some cases [4].
Other potential problems specific to PD include the risk of hyperglycemia from glucose-containing dialysate and worsening of nutritional status due to excessive protein loss through the peritoneal route [42]. Hypothermia, especially in malnourished children and small infants, may occur if pre-warmed PD fluid is not used.
Indications for acute PD in children
In recent years, the indications for acute PD in critically ill patients have been somewhat limited, mainly because of the advent of newer HD techniques and the development of CRRT. The extracorporeal modalities now incorporate several technological advances that have successfully competed with the traditional advantages of PD, such as the use of local anticoagulation which minimizes bleeding risk and tighter ultrafiltration control with precise volumetric systems resulting in better cardiovascular stability.
Acute PD remains the modality of choice in newborns and infants who develop AKI following surgery for congenital heart disease or from sepsis. Acute PD is currently the best modality for managing “uncomplicated” or primary renal disease causing AKI, such as glomerular diseases, acute tubular necrosis due to ischemia and/or drugs and hemolytic-uremic syndrome. This modality has been found to be useful in children with AKI secondary to snake bites and infections such as leptospirosis and malaria [43, 44]. Acute PD is also a useful modality in critically ill children with severe hypotension who are unable to tolerate more intensive extracorporeal therapy. PD is the modality of choice in children with difficult vascular access or with severe bleeding diathesis which makes vascular access and extracorporeal therapy unsafe. The ability of PD to achieve continuous gentle ultrafiltration with minimal impact on hemodynamic status makes it pathophysiologically an attractive therapy in patients with diuretic-resistant congestive heart failure. Ultrafiltration using PD has shown promise in the treatment of adult patients with decompensated or refractory congestive heart failure [45, 46]. Although controlled trials are lacking, children with acute decompensated heart failure constitute another patient group for whom PD for ultrafiltration may be preferred.
However, there is a wide variation between different countries in the choice of acute PD as the primary modality for providing RRT in AKI [47, 48]. The use of PD in the management of AKI has declined steadily in developed regions of the world since the 1990s, while it continues to be the modality of choice in developing countries [49, 50]. Many factors are responsible for the dissimilar pattern in the choice of modality between countries. As mentioned earlier, with the advent of these extracorporeal dialytic therapies with better techniques, improved patient safety profile and improved strategies for vascular access, it is now possible to dialyze critically ill children with unstable hemodynamic status and even newborns and infants with modalities other than PD [51, 52]. The declining use of acute PD in developed regions is also due to the notion that PD is not as efficacious as HD in AKI [53]. Growing loss of physician familiarity with PD coupled with reduced training opportunities in PD that affect competency and increased physician “comfort” with HD and CRRT have also contributed to the decline [54]. PD is the modality of choice in many developing countries, especially in the management of children, because it is cheap and requires minimal resources [55, 56]. Taking into account the importance of PD as a lifesaving therapy for the management of AKI in these minimally resourced countries, the International Society of Nephrology-Global Outreach (ISN-GO), International Society for Peritoneal Dialysis (ISPD) and International Pediatric Nephrology Association (IPNA) in collaboration with other organizations have developed educational programs for acute PD, as part of the global outreach and capacity-building initiatives [57, 58].
Efficiency of acute PD
The most appropriate dose for PD in the management of patients with AKI is poorly defined. In addition to solute clearance, factors such as fluid balance, acid–base and electrolyte disturbances and nutritional factors also have to be considered while dialyzing a child with AKI. A recent guideline recommends that a targeted dose of a weekly Kt/V urea of 2.1 with PD may represent a reasonable goal [12]. There is limited data to determine the minimum PD dose in AKI in children and adults. In a prospective study involving five patients aged 6–839 days who underwent cardiopulmonary by-pass and developed AKI requiring PD, a Kt/V of >2.1 (median 4.84, range 2.12–5.59) was achieved in all patients [59]. In another study involving 20 neonates requiring postoperative PD following cardiopulmonary bypass, the PD creatinine clearance and ultrafiltration rate was 3.4 ml/min/1.73 m2 and 9.75 ml/h, respectively, independent of hemodynamic status or vasopressor support [60]. Similarly, in a study that used dialysate volumes of <20 ml/kg in 12 critically ill infants and children with hypervolemia, the average ultrafiltration obtained was 3.0 ± 0.3 ml/kg/h [61]. Fleming et al. compared PD and CRRT in a small cohort of children (n = 42) who underwent RRT after repair of congenital heart disease [62]. These authors observed that ultrafiltration rate and solute clearance as measured by percentage reduction in urea and creatinine was higher with CRRT than with PD. Controversy exists regarding the efficacy of PD in critically ill patients with AKI, who are often severely hypercatabolic [63].
Strategies to improve dialysis efficiency in acute PD
The efficiency of PD is influenced by choice of peritoneal catheters, method of fluid delivery, the choice of regimen and prescription of PD. Figure 1 describes the setting-up of acute PD and the practical aspects of prescribing, delivering and monitoring PD in patients with AKI.
Flow diagram of the acute peritoneal dialysis (PD) set-up and the associated practical aspects of prescribing, delivering and monitoring PD in patients with acute kidney injury (AKI). Asterisk Catheter change every 3–5 days, @@Delivered Kt/V (the dose target for PD in AKI has not been well studied) \( =\frac{\mathrm{Mean}\;\mathrm{dialysate}\;\mathrm{urea}\;\mathrm{nitrogen}\left(\mathrm{mg}/\mathrm{dl}\right)}{\mathrm{mean}\;\mathrm{serum}\;\mathrm{urea}\;\mathrm{nitrogen}\left(\mathrm{mg}/\mathrm{dl}\right)\mathrm{before}\;\mathrm{and}\;\mathrm{after}\;\mathrm{dialysis}}\times \frac{\mathrm{drained}\;24-\mathrm{hour}\;\mathrm{volume}\left(\mathrm{ml}\right)}{\mathrm{patient}\;\mathrm{urea}\;\mathrm{distribution}\;\mathrm{volume}\left(\mathrm{ml}\right)} \) RRT Renal replacement therapy, CPD continuous peritoneal dialysis, HD hemodialysis, CRRT, continuous renal replacement therapy, ABG arterial blood gas, BUN blood urea nitrogen
Choice of catheter for peritoneal access, PD fluid and method of fluid delivery
Safe and efficient access to the peritoneal cavity is a key factor for PD success. In order to ensure an effective dialysis, it is important to insert a catheter that provides a good dialysate flow with minimal mechanical problems. The common types of catheters used in acute PD are the rigid stylet catheter, Tenckhoff catheter and Cook (Cook Medical Inc., Bloomington, IN) Teflon rigid catheter [64–66]. The flexible Cook Mac-Loc Multipurpose Drainage catheter (Cook Medical Inc.) is an alternative to the Tenckhoff and Cook catheters [67]. The type of catheter used varies widely between countries as it depends on the availability of catheters, cost and expertise for insertion. A percutaneous or surgically placed Tenckhoff catheter is the catheter of choice for acute PD in children as continuous PD can be performed for a long period of time. A Tenckhoff catheter provides higher dialysate flow rates, and the risks of catheter displacement, peri-catheter leakage, organ injury and mechanical complications are much lower than with other catheter types [64, 66]. Rigid catheters should only be used if Tenckhoff or Cook catheters are not available or if the expertise and/or requisite infrastructure to place the Tenckhoff catheter is not available. Recent guidelines from the ISPD suggest that if Tenchkoff catheters are unavailable, catheters using the Seldinger technique for insertion, such as the Cook catheters, are preferred to rigid catheters [12]. However, the reality in many emerging economies is that the rigid catheters are the only available catheters for acute PD [9, 48, 68].
Although the natural biocompatible peritoneal membrane is used as the dialyzer, the conventional dextrose-containing PD fluids may alter the functional and anatomical integrity of the peritoneal membrane over time due to presence of glucose degradation products (GDPs), high lactate and low pH levels. In children on long-term dialysis, the use of pH-neutral solutions with a low concentration of GDPs and bicarbonate or a bicarbonate/lactate mixture as buffer has been associated with better membrane preservation, less pain at peritoneal filling and a smaller increase in intraperitoneal pressure (IPP) for the same amount of fill volume [69, 70]. Several new PD solutions with low GDPs have been introduced, but these are more expensive than the conventional dextrose/lactate-containing solutions. Little information exists on the impact of the use of these more physiological PD fluids in AKI. The decision to use biocompatible PD solutions needs to be individualized in AKI as there are clinically relevant benefits without added risks of harm, as well as potential limitations. Commercial or pharmacy-prepared bicarbonate-based solutions may be used in critically ill children with shock, liver dysfunction and metabolic disorders who have impaired conversion of lactate to bicarbonate [71, 72]. Amino acid-based PD solutions contain very low amounts of GDPs [70]. In a retrospective study in children with AKI, Vande Walle et al. observed lower glucose reabsorption and protein loss but no significant difference in plasma albumin levels with use of PD solutions containing amino acids as compared to only glucose-based solutions [73]. Icodextrin is a less toxic osmotic agent than glucose. However, the slow ultrafiltration process with icodextrin-containing solutions limits its use in those who require rapid fluid or solute removal [72]. Unfortunately, these newer biocompatible fluids are not available in many countries.
A manual, gravity-based closed system or automated system using a cycler may be used for delivering and draining dialysis fluid from the abdominal cavity. In neonates and smaller children, buretrols, which permit the precise measurement of in- and outflow is recommended for optimal dialysis and fluid removal. Automated PD reduces the nursing burden but adds to the cost; in addition, a trained nurse is required for the smooth operation of the cycler which is not easily available in resource-poor settings.
Regimen of PD
Peritoneal dialysis can be performed intermittently or continuously with either manual or automated exchanges using a cycler. The various regimens that have been described are acute intermittent PD, continuous PD (CPD), tidal PD (TPD), high-volume PD (HVPD) and continuous flow PD (CFPD) (Fig. 2). These regimens have been adapted from chronic PD to achieve adequate solute clearances. Data comparing different regimens of acute PD in children are not yet available. Acute intermittent PD with a stiff catheter is used in children in countries with limited resources and cost constraints [9, 48]. The catheter needs to be removed after 3–5 days due to increased risk of peritonitis and the mechanical complications associated with stiff catheters [74]. Hence, the small solute clearance may not be sustained as it is an intermittent process. CPD is similar to continuous ambulatory peritoneal dialysis (CAPD) wherein PD is continued until indicated. CPD may control azotemia and provide good ultrafiltration but being a continuous system with a low dialysate flow rate, it may provide inadequate nitrogen balance in severe hypercatabolic patients [75]; however, the middle molecular weight solute clearance may be higher as the dwell time is longer [76]. TPD is a modality wherein only a portion of dialysate (25–50 % of dwell volume) is drained, giving a tidal volume of 50–75 % [77]. TPD always requires a cycler. The clearance of small and middle molecules is better in TPD than in CPD, possibly because of a high dialysate flow rate and shortened inflow and outflow times which increase dialysate contact time [77, 78]. The disadvantage of TPD is that the protein loss may be higher than with CPD. Chitalia et al. performed a randomized crossover trial in adults and obtained a weekly Kt/V of 2.43 and 1.80 for TPD and CPD, respectively, leading them to conclude that both TPD and CPD are reasonable options for the management of mild-to-moderate hypercatabolic AKI [77]. HVPD is another continuous modality in which each session lasts 24 h and is repeated daily, with a dwell time of 30–50 min, dwell volume of 1200 ml/m2 and 18–22 exchanges/24 h [79]. The use of a high volume has not been shown to interfere with oxygenation in ventilated adult patients [80]. In single-center studies comparing CPD or HVPD with HD in adults, although daily solute clearances achieved with PD were lower than those achieved with daily intermittent or extended HD, PD provided adequate ultrafiltration rates and control of biochemical derangements in most patients [79–81]. CFPD uses a fixed intraperitoneal volume and fast, continuous movement of dialysate into and out of the peritoneal cavity at a high flow rate using two peritoneal catheters (Cook or Tenckhoff dialysis catheters) or one double lumen catheter [82]. In this modality, there is continuous flow of the PD solution, unlike in CPD where the peritoneal fluid is allowed to remain in the peritoneal cavity for 1–4 h. CFPD provides higher solute clearance and ultrafiltration rates than the regimens due to maintenance of the highest possible plasma to dialysate concentration and minimal exchanges during the procedure, both of which maximize the dialysis time. In the first reported study on the use of CFPD in children with AKI admitted to the ICU, CFPD was shown to be ninefold more effective than conventional PD for ultrafiltration and at least three- to fivefold more effective for urea and creatinine clearance [83]. CFPD is technically complex and more costly than the other modalities of PD which may preclude its routine use in AKI, particularly at centers with limited resources.
Diagrammatic representation of PD regimens with respect to urea clearance. Adapted from: Ansari N [97] (open access)
Prescription of PD
There are no standardized prescription of dose, volume and duration of PD. The PD prescription needs to be individualized according to patient size, clinical condition and volume status with a goal to achieve adequate ultrafiltration and biochemical control (Table 1). The choice of dextrose concentration is based on volume status of the child. It is recommended that dialysis fill volumes of 10–20 ml/kg (300 to 600 ml/m2) be used initially, especially in younger children who are at greater risk of leaks, with increasing dwell times and cycle fill volume (if no leakage problems or respiratory compromise) until the desired fill volume of 30 ml/kg (800 ml/m2), as tolerated by the child, is achieved. Larger volumes of 40–50 ml/kg (1100–1400 ml/m2) may be achievable in children with Tenckhoff catheters without the risk of leakage. The recommendation for children under 2 years old is not to exceed fill volumes of >800 ml/m2 due to problems related to increased interperitoneal pressure (IPP) [84]. Whenever possible, the fill volume—especially in infants and smaller children—may be scaled to body surface area (in m2) rather that body weight (per kg) in order to ensure an adequate fill volume. This step will prevent the development of functional hyperpermeability, a major risk factor for ultrafiltration failure [85].
An optimal dwell volume that is well tolerated by the child is an important factor that enhances the adequacy of PD. Bedside measurement of IPP in children on chronic dialysis has been shown to be helpful in scaling the dwell volume to prevent poor clearance secondary to inappropriately low fill volume and at the same time avoid complications associated with large fill volumes, such as poor ultrafiltration due to increased lymphatic absorption and risks related to high IPP (leaks, hernia, pain and pleural effusion) [86]. The upper level “of tolerable” IPP is 8–10 cm H2O (800 ml/m2) and 13–14 cm H2O (1400 ml/m2) in children aged <2 years and >2 years, respectively [59]. Since intra-abdominal hypertension due to increased intra-abdominal pressure is an adverse complication seen in a number of critically ill children, further studies are required to assess the appropriate upper level “of tolerable” IPP in children with AKI receiving PD [87].
The initial exchange time (combined time for inflow, dwell and drain) suggested is 60–90 min, with a dwell time of 30–40 min [12]. Current practice in many parts of the world suggests that 1-h dwells may also be used initially, especially in CPD, which can be gradually increased to ensure adequate dialysis [9, 12, 72]. Shorter dwells can be considered initially in the presence of life-threatening hyperkalemia, hypercatabolic states or fluid overload, especially in neonates and infants, as reducing the dwell time increases the dialysate flow rate resulting in more efficient dialysis. In CPD, the dwell time can be gradually prolonged after 24 h to that used for chronic dialysis based on patient tolerance, adequacy of fluid removal and normalization of metabolic parameters. The duration of PD depends on the dose of PD that needs to be delivered. Fluid balance, metabolic control and renal recovery are factors which determine the length of a dialysis session.
Timing of initiation of PD
One of the important questions to address in the management of children with AKI is when to initiate RRT in patients with AKI. The optimal timing for RRT initiation is not determined. Most of the studies on the timing of RRT in AKI in children involve children receiving CRRT. Analysis of 116 pediatric patients with multiple organ dysfunction syndrome (MODS) and AKI who received CRRT showed that children with patient fluid overload of >20 % at the time of CRRT initiation had decreased survival compared to those with fluid overload of <20 % [88]. In another retrospective cohort study of critically ill children who received CRRT for management of AKI and/or fluid overload (n = 190; 380 treatments), timing of initiation was identified as an independent predictor of mortality with modest effect (adjusted odds ratio 1.05; 95 % confidence interval 1.01–1.11) [89]. Similarly, results from a meta-analysis based on heterogeneous studies of variable quality suggest that outcomes of RRT in critically ill patients with AKI are superior with early institution of RRT, but no clear definition of “early” was provided [90]. In the only study which has examined the timing of PD in AKI, Bojan et al. observed that in their retrospective cohort of 146 neonates and infants who received PD for the treatment of AKI following cardiac surgery, initiation of PD on the first day following surgery was associated with a significant decrease in mortality compared with delayed dialysis [91].
Impact of PD on outcomes in children with AKI
No prospective studies in children have evaluated the effect of dialysis modality on the outcome of children with AKI. The outcomes by various modalities of RRT for AKI are summarized in Table 2; all these studies are retrospective in nature and have patient selection bias. A retrospective analysis of 118 infants and children treated either with PD (n = 82) or CRRT (n = 36) demonstrated that there was no difference in mortality rates between modalities, although CRRT provided better fluid control [92]. Fleming et al. reported similar findings in their retrospective study comparing PD (n = 21) and CRRT (n = 21) in 42 children with AKI who underwent surgery for repair of congenital heart disease [62]. Although a higher proportion of children in the CRRT group obtained negative fluid balance and better solute clearance as compared to the PD group, the mortality rates were similar in the two groups. In a large retrospective analysis of 226 children comparing CRRT (n = 106), HD (n = 61) or PD (n = 59), survival rates between PD and CRRT were similar, but higher survival rates were seen with intermittent HD than with PD or CRRT (89.9 % vs. 49 % and 40 %, respectively) [93]. In another retrospective study of 115 children with AKI requiring RRT, a similar trend of favorable outcome with HD as compared to PD or hemodiafiltration was observed [94]. The better survival rate seen with HD in both of these studies is due to fewer sick children and older children being preferentially dialyzed using HD. A systematic review of 11 studies in adults (7 cohort studies, 4 randomized trials) looking at outcomes in patients with AKI treated with PD found no significant differences in mortality between PD and extracorporeal therapies [95]. However, a significant heterogeneity (I 2 = 73 %, p = 0.03) between studies was noted. Two studies in adults from the same center that compared HVPD with HD or extended HD noted shorter time to renal recovery with PD, possibly due to the absence of extracorporeal circulation resulting in a reduced risk for worsening of renal ischemia [81, 96].
Conclusion
Peritoneal dialysis is a simple, safe and inexpensive procedure and is an option for the supportive management of AKI. In the absence of evidence-based guidelines for the selection of modality of RRT for AKI, the choice of PD is based on local expertise, available resources and the patient’s clinical status. PD performed with a flexible catheter ensuring efficient dialysis is a viable alternative to HD and CRRT in AKI, particularly in children with hemodynamic instability, severe coagulopathy and mild-to-moderate catabolic conditions. It is the modality of choice in settings that do not have access to extracorporeal therapies or if there are cost constraints. The minimum dose of PD in AKI has not been well studied. Various techniques of PD are available to achieve a high small solute clearance. To date, data do not suggest any inferiority of PD over other modalities. Multicentric, randomized studies in children are required to compare adequacy between different RRT modalities and to evaluate the impact of modality on outcomes.
Key summary points
-
1.
PD is a technically simple and inexpensive form of modality used as RRT in children with AKI although its use has declined considerably in developed countries.
-
2.
Using the appropriate catheter and technique, adequate solute clearances, ultrafiltration and metabolic control can be achieved even in critically ill infants and children, although fluid removal may be unpredictable.
-
3.
Currently there is no evidence to suggest significant differences in mortality between PD and extracorporeal dialytic modalities in AKI.
Key research points
-
1.
There is a need for multicentric randomized controlled trials to evaluate the impact of modality of RRT in the outcome of children with AKI and also to identify the group of children who would benefit the most from PD.
-
2.
Evaluation of the delivery of doses and clearance using novel regimens of PD (continuous flow PD, tidal PD, high-volume PD) in various settings of AKI in infants and children is needed.
-
3.
Studies assessing the transport characteristics in acute PD are needed in order to determine the most appropriate PD regimen in children.
Questions (answers are provided following the reference list)
-
1.
Which of the following statement is true:
-
a)
Peritoneal surface area in infants is lower than that in adults (per unit weight)
-
b)
To perform PD, an “ICU environment” is not always necessary
-
c)
PD is not safe in patients with bleeding diathesis
-
d)
Controlled and precise fluid balance can be obtained with acute intermittent PD
-
a)
-
2.
The maximum dwell volume in PD is:
-
a)
800 ml/m2
-
b)
1000 ml/m2
-
c)
1200 ml/m2
-
d)
1400 ml/m2
-
a)
-
3.
All of the following are true with reference to composition of standard 1.7 % peritoneal dialysis fluid with the exception of:
-
a)
Osmolarity of 355 mOsm/l
-
b)
Sodium of 130 mmol/l
-
c)
Potassium of 2 mmol/l
-
d)
Dextrose of 1.7 g/dl
-
a)
-
4.
Which of the following regimens of PD has highest small solute clearance as compared to standard PD:
-
a)
Tidal PD
-
b)
Continuous flow PD
-
c)
High-volume PD
-
d)
All have similar solute clearances
-
a)
References
Hui-Stickle S, Brewer ED, Goldstein SL (2005) Pediatric ARF epidemiology at a tertiary care center from 1999 to 2001. Am J Kidney Dis 45:96–101
Kendirli T, Ekim M, Ozçakar ZB, Yüksel S, Acar B, Oztürk-Hiişmi B, Derelli E, Kavaz A, Yalaki Z, Yalçinkaya F (2007) Renal replacement therapies in pediatric intensive care patients: experiences of one center in Turkey. Pediatr Int 49:345–348
Mehta P, Sinha A, Sami A, Hari P, Kalaivani M, Gulati A, Kabra M, Kabra SK, Lodha R, Bagga A (2012) Incidence of acute kidney injury in hospitalized children. Indian Pediatr 49:537–542
Matthews DE, West KW, Rescorla FJ, Vane DW, Grosfeld JL, Wappner RS, Bergstein J, Andreoli S (1990) Peritoneal dialysis in the first 60 days of life. J Pediatr Surg 25:110–116
Pedersen KR, Hjortdal VE, Christensen S, Pedersen J, Hjortholm K, Larsen SH, Povlsen JV (2008) Clinical outcome in children with acute renal failure treated with peritoneal dialysis after surgery for congenital heart disease. Kidney Int Suppl 108:S81–S86
Morelli S, Ricci Z, Di Chiara L, Stazi GV, Polito A, Vitale V, Giorni C, Iacoella C, Picardo S (2007) Renal replacement therapy in neonates with congenital heart disease. Contrib Nephrol 156:428–433
Kumar V, Ramachandran R, Rathi M, Kohli HS, Sakhuja V, Jha V (2013) Peritoneal dialysis: the great savior during disasters. Perit Dial Int 33:327–329
Anochie IC, Eke FU (2005) Acute renal failure in Nigerian children: Port Harcourt experience. Pediatr Nephrol 20:1610–1614
Mishra OP, Gupta AK, Pooniya V, Prasad R, Tiwary NK, Schaefer F (2012) Peritoneal dialysis in children with acute kidney injury: a developing country experience. Perit Dial Int 32:431–436
Diarrassouba G, Adonis-Koffy L, Niamien E, Yaokreh JB, Coulibaly PA (2015) Acute peritoneal dialysis in African pediatric area experience of pediatric nephrology unit of Yopougon University Hospital (Abidjan, Côte d’Ivoire). Blood Purif 39:141–144
Aloni MN, Nsibu CN, Meeko-Mimaniye M, Ekulu PM, Bodi JM (2012) Acute renal failure in Congolese children: a tertiary institution experience. Acta Paediatr 101:e514–e518
Cullis B, Abdelraheem M, Abrahams G, Balbi A, Cruz DN, Frishberg Y, Koch V, McCulloch M, Numanoglu A, Nourse P, Pecoits-Filho R, Ponce D, Warady B, Yeates K, Finkelstein FO (2014) Peritoneal dialysis for acute kidney injury. Perit Dial Int 34:494–517
Esperanca MJ, Collins D (1966) Peritoneal dialysis efficiency in relation to body weight. J Pediatr Surg 1:162–169
Haubitz M, Brunkhorst R, Wrenger E, Froese P, Schulze M, Koch KM (1996) Chronic induction of C reactive protein by hemodialysis, but not by peritoneal dialysis therapy. Perit Dial Int 16:158–162
Golej J, Kitzmueller E, Hermon M, Boigner H, Burda G, Trittenwein G (2002) Low-volume peritoneal dialysis in 116 neonatal and paediatric critical care patients. Eur J Pediatr 161:385–389
Nolph KD (1988) Continuous versus intermittent therapy for acute renal failure. Peritoneal dialysis for acute renal failure. ASAIO Trans 34:54–55
Zemel D, Imholz AL, de Waart DR, Dinkla C, Struijk DG, Krediet RT (1994) Appearance of tumor necrosis factor-alpha and soluble TNF-receptors I and II in peritoneal effluent of CAPD. Kidney Int 46:1422–1430
Sever MS, Vanholder R, Lameire N (2006) Management of crush-related injuries after disasters. N Engl J Med 354:1052–1063
Portilla D, Shaffer RN, Okusa MD, Mehrotra R, Molitoris BA, Bunchman TE, Ibrahim T (2010) Lessons from Haiti on disaster relief. Clin J Am Soc Nephrol 5:2122–2129
Reznik VM, Randolph G, Collins CM, Peterson BM, Lemire JM, Mendoza SA (1993) Cost analysis of dialysis modalities for pediatric acute renal failure. Perit Dial Int 13:311–313
Flynn JT (2002) Choice of dialysis modality for management of pediatric acute renal failure. Pediatr Nephrol 17:61–69
Genc G, Bicakci U, Gunaydin M, Tander B, Aygun C, Ozkaya O, Rizalar R, Ariturk E, Kucukoduk S, Bernay F (2012) Temporary peritoneal dialysis in newborns and children: a single-center experience over five years. Ren Fail 34:1058–1061
Sizun J, Giroux JD, Rubio S, Guillois B, Alix D, De Parscau L (1993) Peritoneal dialysis in the very low-birth-weight neonate (less than 1000 g). Acta Paediatr 82:488–489
Podel J, Hodelin-Wetzel R, Saha DC, Burns G (2000) Glucose absorption in acute peritoneal dialysis. J Ren Nutr 10:93–97
Basu RK, Wheeler DS, Goldstein S, Doughty L (2011) Acute renal replacement therapy in pediatrics. Int J Nephrol 2011:785392
Mahale AS, Katyal A, Khanna R (2003) Complications of peritoneal dialysis related to increased intra-abdominal pressure. Adv Perit Dial 19:130–135
Bunchman TE, Meldrum MK, Meliones JE, Sedman AB, Walters MB, Kershaw DB (1992) Pulmonary function variation in ventilator dependent critically ill infants on peritoneal dialysis. Adv Perit Dial 8:75–78
Brown ST, Ahearn DJ, Nolph KD (1973) Potassium removal with peritoneal dialysis. Kidney Int 4:67–69
Gabriel DP, Fernandez-Cean J, Balbi AL (2007) Utilization of peritoneal dialysis in the acute setting. Perit Dial Int 27:328–331
Schaefer F, Straube E, Oh J, Mehls O, Mayatepek E (1999) Dialysis in neonates with inborn errors of metabolism. Nephrol Dial Transplant 14:910–918
Uchino T, Endo F, Matsuda I (1998) Neurodevelopmental outcome of long-term therapy of urea cycle disorders in Japan. J Inherit Metab Dis 21:151–159
McBryde DK, Kershaw DB, Bunchman TE, Maxvold NJ, Mottes TA, Kudelka TL, Brophy PD (2006) Renal replacement therapy in the treatment of confirmed or suspected inborn errors of metabolism. J Pediatr 148:770–778
Wiegand C, Thompson T, Bock GH, Mathis RK, Kjellstrand CM, Mauer SM (1980) The management of life-threatening hyperammonemia: a comparison of several therapeutic modalities. J Pediatr 96:142–144
Gortner L, Leupold D, Pohlandt F, Bartmann P (1989) Peritoneal dialysis in the treatment of metabolic crises caused by inherited disorders of organic and amino acid metabolism. Acta Paediatr Scand 78:706–711
Picca S, Dionisi-Vici C, Bartuli A, De Palo T, Papadia F, Montini G, Materassi M, Donati MA, Verrina E, Schiaffino MC, Pecoraro C, Iaccarino E, Vidal E, Burlina A, Emma F (2015) Short-term survival of hyperammonemic neonates treated with dialysis. Pediatr Nephrol 30:839–847
Schaefer B, Ujszaszi A, Schaefer S, Heckert KH, Schaefer F, Schmitt CP (2014) Safety and efficacy of tandem hemodialysis and plasma exchange in children. Clin J Am Soc Nephrol 9:1563–1570
Ponikvar R, Buturović J, Cizman M, Mekjavić I, Kandus A, Premru V, Urbancic A, Zakotnik B, Bren A, Ivanovich P (1998) Hyperbaric oxygenation, plasma exchange, and hemodialysis for treatment of acute liver failure in a 3-year-old child. Artif Organs 22:952–957
Rusthoven E, van de Kar NA, Monnens LA, Schröder CH (2004) Fibrin glue used successfully in peritoneal dialysis catheter leakage in children. Perit Dial Int 24:287–289
Reznik VM, Griswold WR, Peterson BM, Rodarte A, Ferris ME, Mendoza SA (1991) Peritoneal dialysis for acute renal failure in children. Pediatr Nephrol 5:715–717
Kohli HS, Arora P, Kher V, Gupta A, Sharma RK, Bhaumik SK (1995) Daily peritoneal dialysis using a surgically placed Tenckhoff catheter for acute renal failure in children. Ren Fail 17:51–56
Kohli HS, Barkataky A, Kumar RS, Sud K, Jha V, Gupta KL, Sakhuja V (1997) Peritoneal dialysis for acute renal failure in infants: a comparison of three types of peritoneal access. Ren Fail 19:165–170
Day RE, White RH (1977) Peritoneal dialysis in children. Review of 8 years’ experience. Arch Dis Child 52:56–61
Anacleto FE Jr, Collado AB, Wyson AM (2014) Profile of acute kidney injury in pediatric leptospirosis. Ren Fail 36:1090–1094
Bodi JM, Nsibu CN, Aloni MN, Lukute GN, Kunuanuna TS, Tshibassu PM, Pakasa N (2014) Black water fever associated with acute renal failure among Congolese children in Kinshasa. Saudi J Kidney Dis Transpl 25:1352–1358
Kazory A (2015) Peritoneal dialysis for chronic cardiorenal syndrome: lessons learned from ultrafiltration trials. World J Cardiol 7:392–396
Querido S, Branco P, Sousa H, Adragão T, Aguiar C, Pereira S, Costa E, Gaspar A, Barata JD (2016) Peritoneal dialysis as a successful treatment in patients with refractory congestive heart failure: a one-center experience. Clin Nephrol 85:260–265
Warady BA, Bunchman T (2000) Dialysis therapy for children with acute renal failure: Survey results. Pediatr Nephrol 15:11–13
Vasudevan A, Iyengar A, Phadke KD (2012) Modality of choice for renal replacement therapy for children with acute kidney injury. Indian J Nephrol 22:121–124
Williams DM, Sreedhar SS, Mickell JJ, Chan JC (2002) Acute kidney failure: a pediatric experience over 20 years. Arch Pediatr Adolesc Med 156:893–900
Gong WK, Tan TH, Foong PP, Murugasu B, Yap HK (2001) Eighteen years’ experience in pediatric acute dialysis: analysis of predictors of outcome. Pediatr Nephrol 16:212–215
Askenazi DJ, Goldstein SL, Koralkar R, Fortenberry J, Baum M, Hackbarth R, Blowey D, Bunchman TE, Brophy PD, Symons J, Chua A, Flores F, Somers MJ (2013) Continuous renal replacement therapy for children ≤10 kg: a report from the prospective pediatric continuous renal replacement therapy registry. J Pediatr 162:587–592
Bunchman TE, Maxvold NJ, Kershaw DB, Sedman AB, Custer JR (1995) Continuous venovenous hemodiafiltration in infants and children. Am J Kidney Dis 25:17–21
Mehta RL, Letteri JM (1999) Current status of renal replacement therapy for acute renal failure. Am J Nephrol 19:377–382
Berns JS (2010) A survey-based evaluation of self-perceived competency after nephrology fellowship training. Clin J Am Soc Nephrol 5:490–496
Abu-Aisha H, Elamin S (2010) Peritoneal dialysis in Africa. Perit Dial Int 30:23–28
Phadke KD, Dinakar C (2001) The challenges of treating children with renal failure in a developing country. Perit Dial Int 21:S326–S329
Finkelstein FO, Smoyer WE, Carter M, Brusselmans A, Feehally J (2014) Peritoneal dialysis, acute kidney injury, and the Saving Young Lives program. Perit Dial Int 34:478–480
Esezobor C, Ladago T, Lesi F (2014) Peritoneal dialysis for children with acute kidney injury in Lagos, Nigeria: experience with adaptations. Perit Dial Int 34:534–538
Fischbach M, Terzic J, Menouer S, Haraldsson B (2001) Optimal volume prescription for children on peritoneal dialysis. Perit Dial Int 20:603–606
Ricci Z, Morelli S, Ronco C, Polito A, Stazi GV, Giorni C, Di Chiara L, Picardo S (2008) Inotropic support and peritoneal dialysis adequacy in neonates after cardiac surgery. Interact Cardiovasc Thorac Surg 7:116–120
Wood EG, Lynch RE, Fleming SS, Bunchman TE (1991) Ultrafiltration using low volume peritoneal dialysis in critically ill infants and children. Adv Perit Dial 7:266–268
Fleming F, Bohn D, Edwards H, Cox P, Geary D, McCrindle BW, Williams WG (1995) Renal replacement therapy after repair of congenital heart disease in children. A comparison of hemofiltration and peritoneal dialysis. J Thorac Cardiovasc Surg 109:322–331
Yeates K, Cruz DN, Finkelstein FO (2012) Re-examination of the role of peritoneal dialysis to treat patients with acute kidney injury. Perit Dial Int 32:238–241
Wong SN, Geary DF (1988) Comparison of temporary and permanent catheters for acute peritoneal dialysis. Arch Dis Child 63:827–831
Asku N, Yavascan O, Anil M, Kara OD, Erdogan H, Bal A (2007) A ten-year experience in children on chronic peritoneal dialysis—significance of percutaneous placement of peritoneal dialysis catheters. Nephrol Dial Transplant 22:2045–2051
Chadha V, Warady BA, Blowey DL, Simckes AM, Alon US (2000) Tenckhoff catheters prove superior to cook catheters in pediatric acute peritoneal dialysis. Am J Kidney Dis 35:1111–1116
Auron A, Warady BA, Simon S, Blowey DL, Srivastava T, Musharaf G, Alon US (2007) Use of multipurpose drainage catheter for the provision of acute peritoneal dialysis in infants and children. Am J Kidney Dis 49:650–655
Abdelraheem M, Ali E-T, Osman R, Ellidir R, Bushara A, Hussein R, Elgailany S, Bakhit Y, Karrar M, Watson A, Abu-Aisha H (2014) Outcome of acute kidney injury in Sudanese children—an experience from a sub-Saharan African unit. Perit Dial Int 34:526–533
Fischbach M, Warady BA (2009) Peritoneal dialysis prescription in children: bedside principles for optimal practice. Pediatr Nephrol 24:1633–1642
Schmitt CP, Bakkaloglu SA, Klaus G, Schröder C, Fischbach M, European Pediatric Dialysis Working Group (2011) Solutions for peritoneal dialysis in children: recommendations by the European Pediatric Dialysis Working Group. Pediatr Nephrol 26:1137–1147
Vande Walle J, Raes A, Castillo D, Lutz-Dettinger N, Dejaegher A (1997) Advantages of HCO3 solution with low sodium concentration over standard lactate solutions for acute peritoneal dialysis. Adv Perit Dial 1:179–182
Strazdins V, Watson AR, Harvey B, European Pediatric Peritoneal Dialysis Working Group (2004) Renal replacement therapy for acute renal failure in children: European guidelines. Pediatr Nephrol 19:199–207
Vande Walle J, Raes A, Dehoorne J, Mauel R, Dejaeghere A, Matthys D (2004) Combined amino-acid and glucose peritoneal dialysis solution for children with acute renal failure. Adv Perit Dial 20:226–230
Ponce D, Balbi AL, Finkelstein FO (2007) Peritoneal dialysis for the treatment of acute kidney injury. In: Daugirdas JT, Blake PG, Ing TS (eds) Handbook of dialysis, 5th edn. Boston, Little, Brown and Company, p 453
Steiner RW (1989) Continuous equilibration peritoneal dialysis in acute renal failure. Perit Dial Int 9:5–7
Chionh CY, Soni S, Cruz DN, Ronco C (2009) Peritoneal dialysis for acute kidney injury: techniques and dose. Contrib Nephrol 163:278–284
Chitalia VC, Almeida AF, Rai H, Bapat M, Chitalia KV, Acharya VN, Khanna RI (2002) Is peritoneal dialysis adequate for hypercatabolic acute renal failure in developing countries? Kidney Int 61:747–757
Agrawal A, Nolph KD (2000) Advantages of tidal peritoneal dialysis. Perit Dial Int 20:S98–S100
Gabriel DP, Nascimento GV, Caramori JT, Martim LC, Barretti P, Balbi AL (2007) High volume peritoneal dialysis for acute renal failure. Perit Dial Int 27:277–282
Ponce D, Berbel MN, Regina de Goes C, Almeida CT, Balbi AL (2012) High-volume peritoneal dialysis in acute kidney injury: indications and limitations. Clin J Am Soc Nephrol 7:887–894
Gabriel DP, Caramori JT, Martim LC, Barretti P, Balbi AL (2008) High volume peritoneal dialysis vs daily hemodialysis: a randomized, controlled trial in patients with acute kidney injury. Kidney Int 108:S87–S93
Diaz-Buxo J (2001) Evolution of continuous flow peritoneal dialysis and the current state of the art. Semin Dial 14:373–377
Raaijmakers R, Schröder CH, Gajjar P, Argent A, Nourse P (2011) Continuous flow peritoneal dialysis: first experience in children with acute renal failure. Clin J Am Soc Nephrol 6:311–318
Fischbach M, Stefanidis CJ, Watson AR, European Paediatric Peritoneal Dialysis Working Group (2002) Guidelines by an ad hoc European committee on adequacy of the paediatric peritoneal dialysis prescription. Nephrol Dial Transplant 17:380–385
Fischbach M, Dheu C, Seugé-Dargnies L, Delobbe JF (2007) Adequacy of peritoneal dialysis in children: consider the membrane for optimal prescription. Perit Dial Int 27:S167–S170
Fischbach M, Terzic J, Laugel V, Escande B, Dangelser C, Helmstetter A (2003) Measurement of hydrostatic intraperitoneal pressure: a useful tool for the improvement of dialysis dose prescription. Pediatr Nephrol 18:976–980
Thabet FC, Bougmiza IM, Chehab MS, Bafaqih HA, AlMohaimeed SA, Malbrain ML (2015) Incidence, risk factors, and prognosis of intra-abdominal hypertension in critically Ill children: a prospective epidemiological study. J Intensive Care Med 31:403–408
Goldstein SL, Somers MJ, Baum MA, Symons JM, Brophy PD, Blowey D, Bunchman TE, Baker C, Mottes T, McAfee N, Barnett J, Morrison G, Rogers K, Fortenberry JD (2005) Pediatric patients with multi-organ dysfunction syndrome receiving continuous renal replacement therapy. Kidney Int 67:653–658
Modem V, Thompson M, Gollhofer D, Dhar AV, Quigley R (2014) Timing of continuous renal replacement therapy and mortality in critically ill children. Crit Care Med 42:943–953
Karvellas CJ, Farhat MR, Sajjad I, Mogensen SS, Leung AA, Wald R, Bagshaw SM (2011) A comparison of early versus late initiation of renal replacement therapy in critically ill patients with acute kidney injury: a systematic review and meta-analysis. Crit Care 15:R72
Bojan M, Gioanni S, Vouhé PR, Journois D, Pouard P (2012) Early initiation of peritoneal dialysis in neonates and infants with acute kidney injury following cardiac surgery is associated with a significant decrease in mortality. Kidney Int 82:474–481
Bandeira HF, Gama A, Zagury A, Matulevic LC, Mariz LA, Almeida M (2005) Renal replacement therapy (RRT) in acute renal failure in critically ill children under 10 kg. In: Abstracts of the 25th Annual Conference on Peritoneal Dialysis, 16th Annual Symposium on Pediatric Dialysis. Tampa, Florida, USA, 2005. Perit Dial Int 25:S3–S51
Bunchman TE, McBryde KD, Mottes TE, Gardner JJ, Maxvold NJ, Brophy PD (2001) Pediatric acute renal failure: outcome by modality and disease. Pediatr Nephrol 16:1067–1071
Krause I, Herman N, Cleper R, Fraser A, Davidovits M (2011) Impact of dialysis type on outcome of acute renal failure in children: a single-center experience. Isr Med Assoc J 13:153–156
Chionh CY, Soni SS, Finkelstein FO, Ronco C, Cruz D (2013) Use of peritoneal dialysis in AKI: a systematic review. Clin J Am Soc Nephrol 8:1649–1660
Gabriel DP, Caramori JT, Martin LC, Barretti P, Balbi AL (2009) Continuous peritoneal dialysis compared with daily hemodialysis in patients with acute kidney injury. Perit Dial Int 29:S62–S71
Ansari N (2011) Peritoneal dialysis in renal replacement therapy for patients with acute kidney injury. Int J Nephrol 739794. doi: 10.4061/2011/739794
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Key:
1: (b)
2: (d)
3: (c)
4: (b)
Rights and permissions
About this article
Cite this article
Vasudevan, A., Phadke, K. & Yap, HK. Peritoneal dialysis for the management of pediatric patients with acute kidney injury. Pediatr Nephrol 32, 1145–1156 (2017). https://doi.org/10.1007/s00467-016-3482-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-016-3482-6