Abstract
Background
Meeting energy requirements of children with chronic kidney disease (CKD) is paramount to optimising growth and clinical outcome, but little information on this subject has been published. In this study, we examined basal metabolic rate (BMR; a component of energy expenditure) with the aim to determine whether it is related to kidney function independently of weight, height and lean body mass (LBM).
Methods
Twenty children with CKD and 20 healthy age- and gender-matched control children were studied on one occasion. BMR was measured by indirect open circuit calorimetry and predicted by the Schofield equation. Estimated glomerular filtration rate (eGFR) was related to BMR and adjusted for weight, height, age and LBM measured by skinfold thickness.
Results
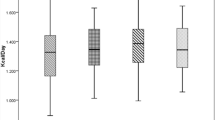
The adjusted BMR of children with CKD did not differ significantly from that of healthy subjects (1296 ± 318 vs.1325 ± 178 kcal/day; p = 0.720). Percentage of predicted BMR also did not differ between the two groups (102 ± 12 % vs. 99 ± 14 %; p = 0.570). Within the CKD group, eGFR (mean 33.7 ± 20.5 mL/min/m2) was significantly related to BMR (β 0.3, r = 0.517, p = 0.019) independently of nutritional status and LBM.
Conclusions
It seems reasonable to use estimated average requirement as the basis of energy prescriptions for children with CKD (mean CKD stage 3 disease). However, those who were sicker had significantly lower metabolic rates.

Similar content being viewed by others
References
Scientific Advisory Committee on Nutrition (2011) Dietary reference values for energy. TSO, London. Available at: http://www.SACN.gov.uk
Department of Health (1991) Dietary reference values for food energy and nutrients for the United Kingdom. No.41. HMSO, London
Shaw V, Lawson M (2007) Clinical paediatric dietetics. Nutritional assessment. John Wiley & Sons, Chichester
KDOQI Work Group (2009) KDOQI clinical practice guideline for nutrition in children with CKD: 2008 update. Executive summary. Am J Kidney Dis 53[3 Suppl 2]:S11-104
Food and Agriculture Organization (2004) Human energy requirements. Report of a joint FAO/WHO/UNU Expert consultation no.1. FAO, Rome. Available at: http://www.fao.org
Avesani CM, Draibe SA, Kamimura MA, Colugnati FA, Cuppari L (2004) Resting energy expenditure of chronic kidney disease patients: influence of renal function and subclinical inflammation. Am J Kidney Dis 44:1008–1016
Utaka S, Avesani CM, Draibe SA, Kamimura MA, Andreoni S, Cuppari L (2005) Inflammation is associated with increased energy expenditure in patients with chronic kidney disease. Am J Clin Nutr 82:801–805
Kamimura MA, Draibe SA, Avesani CM, Canziani ME, Colugnati FA, Cuppari L (2007) Resting energy expenditure and its determinants in hemodialysis patients. Eur J Clin Nutr 61:362–367
Wang AY, Sea MM, Tang N, Lam CW, Chan IH, Lui SF, Sanderson JE, Woo J (2009) Energy intake and expenditure profile in chronic peritoneal dialysis patients complicated with circulatory congestion. Am J Clin Nutr 90:1179–1184
Mafra D, Deleaval P, Teta D, Cleaud C, Arkouche W, Jolivot A, Fouque D (2011) Influence of inflammation on total energy expenditure in hemodialysis patients. J Ren Nutr 21:387–393
Schneeweiss B, Graninger W, Stockenhuber F, Druml W, Ferenci P, Eichinger S, Grimm G, Laggner AN, Lenz K (1990) Energy metabolism in acute and chronic renal failure. Am J Clin Nutr 52:596–601
Cuppari L, de Carvalho AB, Avesani CM, Kamimura MA, Dos Santos Lobao RR, Draibe SA (2004) Increased resting energy expenditure in hemodialysis patients with severe hyperparathyroidism. J Am Soc Nephrol 15:2933–2939
Marques de Aquino T, Avesani CM, Brasileiro RS, de Abreu Carvalhaes JT (2008) Resting energy expenditure of children and adolescents undergoing hemodialysis. J Ren Nutr 18:312–319
Tounian P, Salaun JF, Bensman A, Melchior JC, Veinberg F, Morgant G, Fontaine JL, Girardet JP (1995) Energy-balance in children and young-adults receiving hemodialysis for chronic renal failure. Clin Nutr 14:341–347
Shapiro AC, Bandini LG, Kurtin PS (1992) Estimating energy-requirements for children with renal-disease—a comparison of methods. J Am Diet Assoc 92:571–573
IBM (2012) SPSS SamplePower. Available at: http://www.ibm.com/software/products/us/en/spss-samplepower
SECA GmbH & Co. KG (2012). Available at: http://www.seca.com/english/uk/home/. Accessed 23 Sept 2013
Child Growth Foundation (1994) LMS growth programme. Harlow Healthcare, South Shields. Available at: http://www.childgrowthfoundation.org. Accessed Jan 2007
Delderfield M (2005) SDS individual calculator for British 1990 Growth Reference Data. Public Health Informatics, University of Manchester, Manchester. Available at: http://www.phsim.man.ac.uk/SDScalculator. Accessed Dec 2014
Baty International. Available at: http://www.baty.co.uk/products/categories/170. Accessed Jan 2007
Lohman TG, Slaughter MH, Boileau RA, Bunt J, Lussier L (1984) Bone mineral measurements and their relation to body density in children, youth and adults. Hum Biol 56:667–679
GE Healthcare. Deltatrac 11. GH Healthcare UK, Little Chalfont. Available at: http://www.gehealthcare.com/usen/oximetry/docs/881439.pdf. Accessed 23 Sept 2013
Garrow JS, James WPT, Ralph A (2000) Human nutrition and dietetics, 10th edn. Churchill Livingston, Edinburgh
Medical Research Council. Physical activity assessment—indirect calorimetry. Available at http://dapa-toolkit.mrc.ac.uk/physical-activity-assessment/methods/indirect-calorimetry/index.html. Accessed 31 March 2011
University Hospital Southampton Southampton University Hospital NHS Foundation Trust UHS SUHNFT (2006/2007) Standard operating procedure: measuring resting energy expenditure using indirect calorimetry: GEM standard operating procedure: measuring resting energy expenditure using indirect calorimetry: GEM). Standard operating procedure. WTCRF, Southampton University Hospital NHS Foundation Trust, Southampton
UHS SUHNFT (2006/2007) Standard operating procedure: measuring resting energy expenditure using indirect calorimetry: Delta-trac II standard operating procedure: measuring resting energy expenditure using indirect calorimetry: Delta-trac II). Standard operating procedure. WTCRF, Southampton University Hospital NHS Foundation Trust, Southampton
Elia M, Livesey G (1992) Energy expenditure and fuel selection in biological systems: the theory and practice of calculations based on indirect calorimetry and tracer methods. World Rev Nutr Diet 70:68–131
Schofield WN (1985) Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr 39[Suppl 1]:5–41
Schwartz GJ, Haycock GB, Edelmann CM Jr, Spitzer A (1976) A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 58:259–263
IBM SPSS (2012) Available at: http://public.dhe.ibm.com/common/ssi/ecm/en/yts03009usen/YTS03009USEN.PDF. Accessed 23 Sept 2013
Kuhlmann U, Schwickardi M, Trebst R, Lange H (2001) Resting metabolic rate in chronic renal failure. J Ren Nutr 11:202–206
Panesar A, Agarwal R (2003) Resting energy expenditure in chronic kidney disease: relationship with glomerular filtration rate. Clin Nephrol 59:360–366
Elia M (1992) Energy expenditure in the whole body. Energy metabolism. Tissue determinants and cellular corollaries. Raven Press, New York
Wang AY-M, Sea MM-M, Tang N, Lam CW-K, Chan IH-S, Lui S-F, Sanderson JE, Woo J (2009) Energy intake and expenditure profile in chronic peritoneal dialysis patients complicated with circulatory congestion. Am J Clin Nutr 90:1179–1184
Acknowledgments
Research funding was awarded by the Health Foundation, through the ‘Leadership through clinical practice award’ (2005), for clinical research and leadership training. This study was also supported by the NIHR Southampton Clinical Research Facility.
This report is independent research by the National Institute for Health Research Biomedical Research Unit Funding Scheme. The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Anderson, C.E., Gilbert, R.D. & Elia, M. Basal metabolic rate in children with chronic kidney disease and healthy control children. Pediatr Nephrol 30, 1995–2001 (2015). https://doi.org/10.1007/s00467-015-3095-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-015-3095-5