Abstract
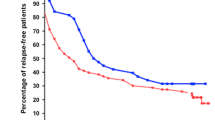
The aim of our study was to determine the clinical course of children with idiopathic childhood nephrotic syndrome (ICNS) who received intravenous methylprednisolone (ivMP) following failure to achieve remission with standard oral prednisolone therapy. This study was designed as a retrospective case record review from 1993 to 2007. Sixteen children received ivMP over the 15-year study period, of whom ten responded, achieving clinical remission. The remaining six children with steroid resistant nephrotic syndrome (SRNS) underwent biopsy [four focal segmental glomerulosclerosis (FSGS), two minimal change disease (MCD)]. Three responders developed late secondary steroid resistance (two FSGS, one MCD). At the latest follow-up (mean 6.7 years), three of the ten ivMP responders and none (0/6) of the children with SRNS had heavy proteinuria and chronic kidney disease (CKD) stage 3-5. The remaining 13 children demonstrated significant steroid dependency but had achieved stable remission following cyclophosphamide and/or ciclosporin therapy. The majority of children with ICNS who do not respond to 4 weeks of daily prednisolone therapy will enter remission following three to five doses of ivMP, thus avoiding a renal biopsy at initial presentation. These children are likely to develop steroid dependency, and the majority will require treatment with alkylating agents and/or ciclosporin to maintain remission. The requirement for ivMP in this setting appears to be associated with a risk of developing CKD in the longer term.

Similar content being viewed by others
References
Webb NJA, Lewis MA, Iqbal J, Smart PJ, Lendon M, Postlethwaite RJ (1996) Childhood steroid sensitive nephrotic syndrome: dose the histology matter? Am J Kidney Dis 27(4):484–488
ISKDC (1981) The primary nephrotic syndrome in children. Clinical significances of histopathologic variants of minimal change. Kidney Int 20(6):765–771
Brodehl J, Krohn HP, Ehrich JH (1982) The treatment of minimal change nephrotic syndrome (lipoid nephrosis): Cooperative studies of the Arbeitsgemeinschaft für Pädiatrische Nephrologie (APN). Klin Padiatr 194(3):162–165
Murnaghan K, Vasmant D, Bensman A (1984) Pulse methylprednisolone therapy in severe idiopathic childhood nephrotic syndrome. Acta Pediatr Scand 73(6):733–739
Letavernier B, Letavernier E, Leroy S, Baudet-Bonneville V, Bensman A, Ulinski T (2008) Prediction of high-degree steroid dependency in pediatric idiopathic nephrotic syndrome. Pediatr Nephrol 23(12):2221–2226
Tune BM, Mendoza SA (1997) Treatment of idiopathic nephrotic syndrome: regimens and outcomes in children and adults. J Am Soc Nephrol 8(5):824–832
Kim JS, Bellew CA, Silverstein DM, Aviles DH, Boineau FG, Vehaskari VM (2005) High incidence of initial and late steroid resistance in childhood nephrotic syndrome. Kidney Int 68(3):1275–1281
International Study of Kidney Disease in Children (1981) The primary nephrotic syndrome in children: Identification of patients with minimal change nephrotic syndrome from initial response to prednisolone. J Pediatr 98(4):561–564
Tarshish P, Tobin JN, Bernstein J, Edelmann CM (1997) Prognostic significance of early course of minimal change nephrotic syndrome: Report of the International Study of Kidney Disease in Children. J Am Soc Nephrol 8(5):769–776
Ehrich JH, Brodehl J (1993) Long versus standard prednisolone therapy for initial treatment of idiopathic nephrotic syndrome. Eur J Pediatr 152(4):357–361
Gambertoglio JG, Frey FJ, Holdford NHG, Birnbaum JL, Lizak PS, Vincenti F, Feduska NJ, Salvatierra O, Amend WJC (1982) Prednisone and prednisolone bioavailability in renal transplant patients. Kidney Int 21(4):621–626
Nammalvar BR, Vijayakumar M, Prahlad N (2006) Experience of renal biopsy in children with nephrotic syndrome. Pediatr Nephrol 21(2):286–288
Klein-Gitelman MS, Pachman LM (1988) Intravenous corticosteroids: adverse events are more variable than expected in children. J Rheumatol 25(10):1995–2002
Akikusa JD, Feldman BM, Gross GJ, Silverman ED, Schneider R (2007) Sinus bradycardia after intravenous pulse methylprednisolone. Pediatrics 119(3):e778–e782
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shenoy, M., Plant, N.D., Lewis, M.A. et al. Intravenous methylprednisolone in idiopathic childhood nephrotic syndrome. Pediatr Nephrol 25, 899–903 (2010). https://doi.org/10.1007/s00467-009-1417-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-009-1417-1