Abstract
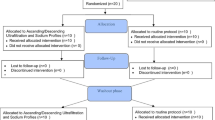
The aim of this study was to adjust dry weight by short-term blood volume monitoring (BVM)-guided ultrafiltration and evaluate the effects of optimizing dry weight on blood pressure (BP) control and intradialytic symptoms (IDS) in a group of hypertensive hemodialysis (HD) patients. The study was performed in four sequential phases, each of which lasted for 1 week, on nine hypertensive HD patients (six girls, age 16.9 ± 3.1 years). In phase I, patients were observed by BVM. In phase II, BVM was used to guide ultrafiltration to adjust dry weight. Antihypertensive drugs were gradually tapered or withheld in phase III, when the patients were hypotensive and/or their IDS increased. In phase IV, this particular weight was maintained without any intervention. Pre- and post-HD body weight, pre-HD, post-HD, 30 min after HD casual BP values, and IDS in each HD session were recorded. The BP was also assessed by 44-h ambulatory BP monitoring (ABPM), which is an ideal method to determine BP changes throughout the interdialytic period at the beginning of phase I and at the end of phase IV. There was a decrease in mean dry weight, all casual systolic BPs, and systolic/diastolic ABPM at the end of the study (all p ≤ 0.05). Antihypertensive drugs were stopped in five patients and reduced in two during phase III of the study. The IDS was more frequent (36%) in phase IV than in phase I (16%); however, this increase did not reach statistical significance. The results of this study suggest that short-term BVM guided-ultrafiltration may be a useful tool to diagnose volume overload and to adjust dry weight and, consequently, to achieve a better control of BP in pediatric HD patients.
Similar content being viewed by others
References
Mitsnefes M, Stablein D (2005) Hypertension in pediatric patients on long-term dialysis: a report of the North American Pediatric Renal Transplant Cooperative Study (NAPRTCS). Am J Kidney Dis 45:309–315
Parekh RS, Carroll CE, Wolfe RA, Port FK (2002) Cardiovascular mortality in children and young adults with end-stage kidney disease. J Pediatr 141:191–197
Van De Voorde RG, Barletta GM, Chand DH, Dresner IG, Lane J, Leiser J, Lin JJ, Pan CG, Patel H, Valentini RP, Mitsnefes MM (2007) Blood pressure control in pediatric hemodialysis: the Midwest Pediatric Nephrology Consortium Study. Pediatr Nephrol 22:547–553
Hörl MP, Hörl WH (2002) Hemodialysis-associated hypertension: pathophysiology and therapy. Am J Kidney Dis 39:227–244
Jaeger JQ, Mehta RL (1999) Assessment of dry weight in hemodialysis: an overview. J Am Soc Nephrol 10:392–403
Ishibe S, Peixoto AJ (2004) Methods of assesment of volume status and intercompartmental fluid shifts in hemodialysis patients: implications in clinical practice. Semin Dial 17:37–43
Leypoldt JK, Cheung AK (1998) Evaluating volume status in hemodialysis patients. Adv Ren Replace Ther 5:64–74
Leypoldt JK, Lindsay RM (1999) Hemodynamic monitoring during hemodialysis. Adv Ren Replace Ther 6:233–242
De Vries JP, Kouw PM, Nardo JM, Van der Meer NJ, Olthof CG, Oe LP, Donker AJ, De Vries PM (1993) Non-invasive monitoring of blood volume during hemodialysis: its relation with post-dialytic dry weight. Kidney Int 44:851–854
Steuer RR, Leypoldt JK, Cheung AK, Senekjian HO, Conis JM (1996) Reducing symptoms during hemodialysis by continuously monitoring the hematocrit. Am J Kidney Dis 27:525–532
Steuer RR, Conis JM (1996) The incidence of hypovolemic morbidity in hemodialysis. Dial Transplant 25:272–274
Wilkie ME, Lindley EJ, Edwards L, Roebuck AF, Warwick G, Brown CB (1996) Improved ultrafiltration control using an on-line blood volume monitor (BVM). Nephrol Dial Transplant 11:A202
Steuer RR, Germain MJ, Leypoldt JK, Cheung AK (1998) Enhanced fluid removal guided by blood volume monitoring during hemodialysis. Artif Organs 22:627–632
Rodriguez HJ, Domenici R, Diroll A, Goykhman I (2005) Assessment of dry weight by monitoring changes in blood volume during hemodialysis using Crit-Line. Kidney Int 68:854–861
Jain SR, Smith L, Brewer ED, Goldstein SL (2001) Non-invasive intravascular monitoring in the pediatric hemodialysis population. Pediatr Nephrol 16:15–18
Michael M, Brewer ED, Goldstein SL (2004) Blood volume monitoring to achieve target weight in pediatric hemodialysis patients. Pediatr Nephrol 19:432–437
Goldstein SL, Smith JM, Currier H (2003) Noninvasive interventions to decrease hospitalization and associated costs for pediatric patients receiving hemodialysis. J Am Soc Nephrol 14:2127–2131
Patel HP, Goldstein SL, Mahan JD, Smith B, Fried CB, Currier H, Flynn JT (2007) A standard, noninvasive monitoring of hematocrit algorithm improves blood pressure control in pediatric hemodialysis patients. Clin J Am Soc Nephrol 2:252–257
Leypoldt JK, Cheung AK, Steuer RR, Harris DH, Conis JM (1995) Determination of circulating blood volume by continuously monitoring hematocrit during hemodialysis. J Am Soc Nephrol 6:214–219
National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents (2004) The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114:555–576
Soergel M, Kirschstein M, Busch C, Danne T, Gellermann J, Holl R, Krull F, Reichert H, Reusz GS, Rascher W (1997) Oscillometric twenty-four-hour ambulatory blood pressure values in healthy children and adolescents: a multicenter trial including 1141 subjects. J Pediatr 130:178–184
Fischbach M, Edefonti A, Schröder C, Watson A (2005) Hemodialysis in children: general practical guidelines. Pediatr Nephrol 20:1054–1066
Cohen EP (2000) Hypertension in chronic hemodialysis: viewing a paradox, and some notes on therapy. Dial Transplant 29:535–539
Sankaranarayanan N, Sergio Santos FF, Peixoto AJ (2004) Blood pressure measurement in dialysis patients. Adv Chronic Kidney Dis 11:134–142
Mitra S, Chandna SM, Farrington K (1999) What is hypertension in chronic hemodialysis? The role of interdialytic blood pressure monitoring. Nephrol Dial Transplant 14:2915–2921
Mitsnefes MM, Kimball TR, Daniels SR (2003) Office and ambulatory blood pressure elevation in children with chronic renal failure. Pediatr Nephrol 18:145–149
Mailloux LU, Haley WE (1998) Hypertension in ESRD patient: pathophysiology, therapy, outcomes, and future directions. Am J Kidney Dis 32:705–719
Sorof JM, Brewer ED, Portman RJ (1999) Ambulatory blood pressure monitoring and interdialytic weight gain in children receiving chronic hemodialysis. Am J Kidney Dis 33:667–674
Özkahya M, Töz H, Ünsal A, Özerkan F, Asçı G, Gürgün C, Akçiçek F, Dorhout Mees EJ (1999) Treatment of hypertension in dialysis patients by ultrafiltration: role of cardiac dilatation and time factor. Am J Kidney Dis 34:218–221
Movilli E, Gaggia P, Zubani R, Camerini C, Vizzardi V, Parrinello G, Savoldi S, Fischer MS, Londrino F, Cancarini G (2007) Association between high ultrafiltration rates and mortality in uraemic patients on regular haemodialysis. A 5-year prospective observational multicentre study. Nephrol Dial Transplant 22:3547–3552
Hothi DK, Harvey E, Goia CM, Geary D (2008) Blood-volume monitoring in paediatric haemodialysis. Pediatr Nephrol 23:813–820
Fiscbach M, Terzic J, Laugel V, Dheu C, Menouer S, Helms P, Livolsi A (2004) Daily on-line hemodiafiltration: a pilot trial in children. Nephrol Dial Transplant 19:2360–2367
Charra B, Bergström J, Scribner BJ (1998) Blood pressure control in dialysis patients: importance of the lag phenomenon. Am J Kidney Dis 32:720–724
Acknowledgements
This work was supported by the Turkish Foundation of Pediatrics, and Turkish Society of Nephrology Istanbul Branch. It was partly presented at the 39th Annual Meeting of the European Society for Pediatric Nephrology, September 10–13, 2005, Istanbul, Turkey, and has been published in abstract form (abstract; Candan C et al, Pediatr Nephrol 20: C56, 2005). The authors thank the nurses of the Children’s Hospital Hemodialysis Unit of Cerrahpasa Medical Faculty, especially Gulseren Pehlivan and Refiye Basegmez for their assistance in performing this study. The authors thank to Mehmet Sukru Sever M.D. for his criticism and advice.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Candan, C., Sever, L., Civilibal, M. et al. Blood volume monitoring to adjust dry weight in hypertensive pediatric hemodialysis patients. Pediatr Nephrol 24, 581–587 (2009). https://doi.org/10.1007/s00467-008-0985-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00467-008-0985-9