Abstract
Background
Drainage fluid amylase (DFA) is useful for predicting clinically relevant postoperative pancreatic fistula (CR-POPF) after distal pancreatectomy (DP). However, difference in optimal cutoff value of DFA for predicting CR-POPF between open DP (ODP) and laparoscopic DP (LDP) has not been investigated. This study aimed to identify the optimal cutoff values of DFA for predicting CR-POPF after ODP and LDP.
Methods
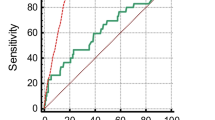
Data for 294 patients (ODP, n = 127; LDP, n = 167) undergoing DP at Kobe University Hospital between 2010 and 2021 were reviewed. Propensity score matching was performed to minimize treatment selection bias. Receiver operating characteristic (ROC) analysis was performed to determine the optimal cutoff values of DFA for predicting CR-POPF for ODP and LDP. Logistic regression analysis for CR-POPF was performed to investigate the diagnostic value of DFA on postoperative day (POD) three with identified cutoff value.
Results
In the matched cohort, CR-POPF rates were 24.7% and 7.9% after ODP and LDP, respectively. DFA on POD one was significantly lower after ODP than after LDP (2263 U/L vs 4243 U/L, p < 0.001), while the difference was not significant on POD three (543 U/L vs 1221 U/L, p = 0.171). ROC analysis revealed that the optimal cutoff value of DFA on POD one and three for predicting CR-POPF were different between ODP and LDP (ODP, 3697 U/L on POD one, 1114 U/L on POD three; LDP, 10564 U/L on POD one, 6020 U/L on POD three). Multivariate analysis showed that DFA on POD three with identified cutoff value was the independent predictor for CR-POPF both for ODP and LDP.
Conclusions
DFA on POD three is an independent predictor for CR-POPF after both ODP and LDP. However, the optimal cutoff value for it is significantly higher after LDP than after ODP. Optimal threshold of DFA for drain removal may be different between ODP and LDP.
Graphical abstract



Similar content being viewed by others
References
Van Buren G, Bloomston M, Schmidt CR, Behrman SW, Zyromski NJ, Ball CG, Morgan KA, Hughes SJ, Karanicolas PJ, Allendorf JD, Vollmer CM Jr, Ly Q, Brown KM, Velanovich V, Winter JM, McElhany AL, Muscarella P 2nd, Schmidt CM, House MG, Dixon E, Dillhoff ME, Trevino JG, Hallet J, Coburn NSG, Nakeeb A, Behrns KE, Sasson AR, Ceppa EP, Abdel-Misih SRZ, Riall TS, Silberfein EJ, Ellison EC, Adams DB, Hsu C, Tran Cao HS, Mohammed S, Villafañe-Ferriol N, Barakat O, Massarweh NN, Chai C, Mendez-Reyes JE, Fang A, Jo E, Mo Q, Fisher WE (2017) A prospective randomized multicenter trial of distal pancreatectomy with and without routine intraperitoneal drainage. Ann Surg 266:421–431
Yamada S, Fujii T, Sonohara F, Kawai M, Shibuya K, Matsumoto I, Fukuzawa K, Baba H, Aoki T, Unno M, Satoi S, Kishi Y, Hatano E, Uemura K, Horiguchi A, Sho M, Takeda Y, Shimokawa T, Kodera Y, Yamaue H (2021) Safety of combined division vs separate division of the splenic vein in patients undergoing distal pancreatectomy: a noninferiority randomized clinical trial. JAMA Surg 156:418–428
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, Allen P, Andersson R, Asbun HJ, Besselink MG, Conlon K, Del Chiaro M, Falconi M, Fernandez-Cruz L, Fernandez-Del Castillo C, Fingerhut A, Friess H, Gouma DJ, Hackert T, Izbicki J, Lillemoe KD, Neoptolemos JP, Olah A, Schulick R, Shrikhande SV, Takada T, Takaori K, Traverso W, Vollmer CR, Wolfgang CL, Yeo CJ, Salvia R, Buchler M (2017) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery 161:584–591
de Rooij T, van Hilst J, van Santvoort H, Boerma D, van den Boezem P, Daams F, van Dam R, Dejong C, van Duyn E, Dijkgraaf M, van Eijck C, Festen S, Gerhards M, Groot Koerkamp B, de Hingh I, Kazemier G, Klaase J, de Kleine R, van Laarhoven C, Luyer M, Patijn G, Steenvoorde P, Suker M, Abu Hilal M, Busch O, Besselink M (2019) Minimally invasive versus open distal pancreatectomy (LEOPARD): a multicenter patient-blinded randomized controlled trial. Ann Surg 269:2–9
Ecker BL, McMillan MT, Allegrini V, Bassi C, Beane JD, Beckman RM, Behrman SW, Dickson EJ, Callery MP, Christein JD, Drebin JA, Hollis RH, House MG, Jamieson NB, Javed AA, Kent TS, Kluger MD, Kowalsky SJ, Maggino L, Malleo G, Valero V 3rd, Velu LKP, Watkins AA, Wolfgang CL, Zureikat AH, Vollmer CM Jr (2019) Risk factors and mitigation strategies for pancreatic fistula after distal pancreatectomy: analysis of 2026 resections from the International, Multi-institutional Distal Pancreatectomy Study Group. Ann Surg 269:143–149
Vass DG, Hodson J, Isaac J, Marudanayagam R, Mirza DF, Muiesan P, Roberts K, Sutcliffe RP (2018) Utility of drain fluid amylase measurement on the first postoperative day after distal pancreatectomy. HPB 20:803–808
Daniel F, Tamim H, Hosni M, Ibrahim F, Mailhac A, Jamali F (2019) Validation of day 1 drain fluid amylase level for prediction of clinically relevant fistula after distal pancreatectomy using the NSQIP database. Surgery 165:315–322
Maggino L, Malleo G, Bassi C, Allegrini V, Beane JD, Beckman RM, Chen B, Dickson EJ, Drebin JA, Ecker BL, Fraker DL, House MG, Jamieson NB, Javed AA, Kowalsky SJ, Lee MK, McMillan MT, Roses RE, Salvia R, Valero V 3rd, Velu LKP, Wolfgang CL, Zureikat AH, Vollmer CM Jr (2019) Identification of an optimal cut-off for drain fluid amylase on postoperative day 1 for predicting clinically relevant fistula after distal pancreatectomy: a multi-institutional analysis and external validation. Ann Surg 269:337–343
Villafane-Ferriol N, Van Buren G, Mendez-Reyes JE, McElhany AL, Massarweh NN, Silberfein EJ, Hsu C, Tran Cao HS, Schmidt C, Zyromski NJ, Dillhoff ME, Roch A, Oliva E, Smith AC, Zhang Q, Fisher WE (2018) Sequential drain amylase to guide drain removal following pancreatectomy. HPB 20:514–520
Nassour I, AlMasri S, Hodges JC, Hughes SJ, Zureikat A, Paniccia A (2022) Novel calculator to estimate the risk of clinically relevant postoperative pancreatic fistula following distal pancreatectomy. J Gastrointest Surg 26:1436–1444
Kosaka H, Satoi S, Yamamoto T, Hirooka S, Yamaki S, Kotsuka M, Sakaguchi T, Inoue K, Matsui Y, Sekimoto M (2019) Clinical impact of the sequentially-checked drain removal criteria on postoperative outcomes after pancreatectomy: a retrospective study. J Hepatobiliary Pancreat Sci 26:426–434
Kawai M, Tani M, Terasawa H, Ina S, Hirono S, Nishioka R, Miyazawa M, Uchiyama K, Yamaue H (2006) Early removal of prophylactic drains reduces the risk of intra-abdominal infections in patients with pancreatic head resection: prospective study for 104 consecutive patients. Ann Surg 244:1–7
Linnemann RJA, Patijn GA, van Rijssen LB, Besselink MG, Mungroop TH, de Hingh IH, Kazemier G, Festen S, de Jong KP, van Eijck CHJ, Scheepers JJG, van der Kolk M, Dulk MD, Bosscha K, Busch OR, Boerma D, van der Harst E, Nieuwenhuijs VB (2019) The role of abdominal drainage in pancreatic resection—a multicenter validation study for early drain removal. Pancreatology 19:888–896
Seykora TF, Liu JB, Maggino L, Pitt HA, Vollmer CM Jr (2020) Drain management following distal pancreatectomy: characterization of contemporary practice and impact of early removal. Ann Surg 272:1110–1117
van Hilst J, de Rooij T, Abu Hilal M, Asbun HJ, Barkun J, Boggi U, Busch OR, Conlon KC, Dijkgraaf MG, Han HS, Hansen PD, Kendrick ML, Montagnini AL, Palanivelu C, Røsok BI, Shrikhande SV, Wakabayashi G, Zeh HJ, Vollmer CM, Kooby DA, Besselink MG (2017) Worldwide survey on opinions and use of minimally invasive pancreatic resection. HPB 19:190–204
Nakamura M, Wakabayashi G, Miyasaka Y, Tanaka M, Morikawa T, Unno M, Tajima H, Kumamoto Y, Satoi S, Kwon M, Toyama H, Ku Y, Yoshitomi H, Nara S, Shimada K, Yokoyama T, Miyagawa S, Toyama Y, Yanaga K, Fujii T, Kodera Y, Tomiyama Y, Miyata H, Takahara T, Beppu T, Yamaue H, Miyazaki M, Takada T (2015) Multicenter comparative study of laparoscopic and open distal pancreatectomy using propensity score-matching. J Hepatobiliary Pancreat Sci 22:731–736
Kishi D, Nezu R, Ito T, Taniguchi E, Momiyama T, Obunai S, Ohashi S, Matsuda H (2000) Laparoscopic-assisted surgery for Crohn’s disease: reduced surgical stress following ileocolectomy. Surg Today 30:219–222
Tsujimoto H, Ono S, Sugasawa H, Ichikura T, Yamamoto J, Hase K (2010) Gastric tube reconstruction by laparoscopy-assisted surgery attenuates postoperative systemic inflammatory response after esophagectomy for esophageal cancer. World J Surg 34:2830–2836
American Diabetes Association Professional Practice Committee (2022) 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2022. Diabetes Care 45:S17–S38
Yang F, Jin C, Hao S, Fu D (2019) Drain contamination after distal pancreatectomy: incidence, risk factors, and association with postoperative pancreatic fistula. J Gastrointest Surg 23:2449–2458
Hiki N, Shimizu N, Yamaguchi H, Imamura K, Kami K, Kubota K, Kaminishi M (2006) Manipulation of the small intestine as a cause of the increased inflammatory response after open compared with laparoscopic surgery. Br J Surg 93:195–204
Xourafas D, Ashley SW, Clancy TE (2017) Comparison of perioperative outcomes between open, laparoscopic, and robotic distal pancreatectomy: an analysis of 1815 patients from the ACS-NSQIP Procedure-Targeted Pancreatectomy Database. J Gastrointest Surg 21:1442–1452
Schouten TJ, Henry AC, Smits FJ, Besselink MG, Bonsing BA, Bosscha K, Busch OR, van Dam RM, van Eijck CH, Festen S, Groot Koerkamp B, van der Harst E, de Hingh IHJT, Kazemier G, Liem MSL, de Meijer VE, Patijn GA, Roos D, Schreinemakers JMJ, Stommel MWJ, Wit F, Daamen LA, Molenaar IQ, van Santvoort HC, Dutch Pancreatic Cancer Group (2023) Risk models for developing pancreatic fistula after pancreatoduodenectomy: validation in a nationwide prospective cohort. Ann Surg 278:1001–1008
Funding
The authors declare no sources of funding for this research and publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Jun Ishida, Hirochika Toyama, Sadaki Asari, Tadahiro Goto, Yoshihide Nanno, Toshihiko Yoshida, Shinichi So, Takeshi Urade, Kenji Fukushima, Hidetoshi Gon, Daisuke Tsugawa, Shohei Komatsu, Hiroaki Yanagimoto, Masahiro Kido, and Takumi Fukumoto have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ishida, J., Toyama, H., Asari, S. et al. Optimal cutoff values of drain amylase for predicting pancreatic fistula are different between open and laparoscopic distal pancreatectomy. Surg Endosc 38, 2699–2708 (2024). https://doi.org/10.1007/s00464-024-10781-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-024-10781-3