Abstract
Background
3D computed tomography (CT) has been seldom used for the evaluation of hiatal hernias (HH) in surgical patients. This study aims to describe the 3D CT findings in candidates for laparoscopic or robotic antireflux surgery or HH repair and compare them with other tests.
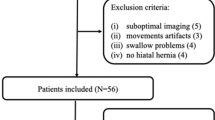
Methods
Thirty patients with HH and/or gastroesophageal reflux disease (GERD) who were candidates for surgical treatment and underwent high-resolution CT were recruited. The variables studied were distance from the esophagogastric junction (EGJ) to the hiatus; total gastric volume and herniated gastric volume, percentage of herniated volume in relation to the total gastric volume; diameters and area of the esophageal hiatus.
Results
HH was diagnosed with CT in 21 (70%) patients. There was no correlation between the distance EGJ-hiatus and the herniated gastric volume. There was a statistically significant correlation between the distance from the EGJ to the hiatus and the area of the esophageal hiatus of the diaphragm. There was correlation between tomographic and endoscopic findings for the presence and size of HH. HH was diagnosed with manometry in 9 (50%) patients. There was no correlation between tomographic and manometric findings for the diagnosis of HH and between hiatal area and lower esophageal sphincter basal pressure. There was no correlation between any parameter and DeMeester score.
Conclusions
The anatomy of HH and the hiatus can be well defined by 3D CT. The EGJ-hiatus distance may be equally measured by 3D CT or upper digestive endoscopy. DeMeester score did not correlate with any anatomical parameter.




Similar content being viewed by others
References
Jobe BA, Richter JE, Hoppo T, Peters JH, Bell R, Dengler WC, DeVault K, Fass R, Gyawali CP, Kahrilas PJ, Lacy BE, Pandolfino JE, Patti MG, Swanstrom LL, Kurian AA, Vela MF, Vaezi M, DeMeester TR (2013) Preoperative diagnostic workup before antireflux surgery: an evidence and experience-based consensus of the Esophageal Diagnostic Advisory Panel. J Am Coll Surg 217(4):586–597. https://doi.org/10.1016/j.jamcollsurg.2013.05.023
Ouyang W, Dass C, Zhao H, Kim C, Criner G, COPDGene Investigators (2016) Multiplanar MDCT measurement of esophageal hiatus surface area: association with hiatal hernia and GERD. Surg Endosc 30(6):2465–2472. https://doi.org/10.1007/s00464-015-4499-9
Kao AM, Ross SW, Otero J, Maloney SR, Prasad T, Augenstein VA, Heniford BT, Colavita PD (2020) Use of computed tomography volumetric measurements to predict operative techniques in paraesophageal hernia repair. Surg Endosc 34(4):1785–1794. https://doi.org/10.1007/s00464-019-06930-8
Boru CE, Rengo M, Iossa A, De Angelis F, Massaro M, Spagnoli A, Guida A, Laghi A, Silecchia G (2021) Hiatal surface area’s CT scan measurement is useful in hiatal hernia’s treatment of bariatric patients. Minim Invasive Ther Allied Technol 30(2):86–93. https://doi.org/10.1080/13645706.2019.1683033
Kahrilas PJ, Kim HC, Pandolfino JE (2008) Approaches to the diagnosis and grading of hiatal hernia. Best Pract Res Clin Gastroenterol 22(4):601–616. https://doi.org/10.1016/j.bpg.2007.12.007
Schlottmann F, Herbella FA, Patti MG (2017) Understanding the Chicago classification: from tracings to patients. J Neurogastroenterol Motil 23(4):487–494. https://doi.org/10.5056/jnm17026
Hayward J (1961) The lower end of the oesophagus. Thorax 16(1):36–41. https://doi.org/10.1136/thx.16.1.36
Tolone S, Savarino E, Zaninotto G, Gyawali CP, Frazzoni M, de Bortoli N, Frazzoni L, Del Genio G, Bodini G, Furnari M, Savarino V, Docimo L (2018) High-resolution manometry is superior to endoscopy and radiology in assessing and grading sliding hiatal hernia: a comparison with surgical in vivo evaluation. United Eur Gastroenterol J 6(7):981–989. https://doi.org/10.1177/2050640618769160
Liu M, Stefanova DI, Finnerty BM, Schnoll-Sussman FH, Katz PO, Fahey TJ 3rd, Zarnegar R (2022) The impact of pneumoperitoneum on esophagogastric junction distensibility during anti-reflux surgery. Surg Endosc 36(1):367–374. https://doi.org/10.1007/s00464-021-08291-7
Koch OO, Schurich M, Antoniou SA, Spaun G, Kaindlstorfer A, Pointner R, Swanstrom LL (2014) Predictability of hiatal hernia/defect size: is there a correlation between pre- and intraoperative findings? Hernia 18(6):883–888. https://doi.org/10.1007/s10029-012-1033-z
Martinelo V, Mardiros Herbella FA, Patti MG (2015) High-resolution manometry findings in patients with an intrathoracic stomach. Am Surg 81(4):354–357
Iorio P, Vanderbecq Q, Mouhadi SE, Arrivé L (2023) Imaging of the biliary tract. Curr Opin Gastroenterol 39(2):59–66. https://doi.org/10.1097/MOG.0000000000000912
Wallner B (2009) Endoscopically defined gastroesophageal junction coincides with the anatomical gastroesophageal junction. Surg Endosc 23(9):2155–2158. https://doi.org/10.1007/s00464-008-0238-9
Batirel HF, Uygur-Bayramicli O, Giral A, Ekici B, Bekiroglu N, Yildizeli B, Yüksel M (2010) The size of the esophageal hiatus in gastroesophageal reflux pathophysiology: outcome of intraoperative measurements. J Gastrointest Surg 14(1):38–44. https://doi.org/10.1007/s11605-009-1047-8
Koch OO, Kaindlstorfer A, Antoniou SA, Asche KU, Granderath FA, Pointner R (2012) Influence of the esophageal hiatus size on the lower esophageal sphincter, on reflux activity and on symptomatology. Dis Esophagus 25(3):201–208. https://doi.org/10.1111/j.1442-2050.2011.01238.x
Menezes MA, Herbella FAM (2017) Pathophysiology of gastroesophageal reflux disease. World J Surg 41(7):1666–1671. https://doi.org/10.1007/s00268-017-3952-4
Herbella FAM, Schlottmann F, Patti MG (2018) Pathophysiology of gastroesophageal reflux disease: how an antireflux procedure works (or does not work). Updates Surg 70(3):343–347. https://doi.org/10.1007/s13304-018-0562-0
Funding
Dr. Fernando Herbella was funded by CNPq, a Federal governmental funding Brazilian agency under #302838/2021-0.
Author information
Authors and Affiliations
Contributions
AVS, FAMH: conception and design, acquisition of data, analysis and interpretation of data, drafting the article, and final approval of the version to be published. CED, PV: conception and design, acquisition of data, and final approval of the version to be published. WCGMN, RPP, FDT: acquisition of data and final approval of the version to be published. RCK, MGP: review for intellectual content and final approval of the version to be published.
Corresponding author
Ethics declarations
Disclosures
Fernando Herbella was funded by CNPq, a Federal government funding Brazilian agency under #302838/2021-0. André V. Santana, Carlos E. Domene, Paula Volpe, William C. G. M. Neto, Rodrigo P. Polízio, Fernando D. Tamamoto, Rafael C. Katayama, and Marco G. Patti have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Meeting presentation: Poster presentation at the SSAT annual meeting, May, 2023, Chicago.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Santana, A.V., Herbella, F.A.M., Domene, C.E. et al. High-resolution 3-dimensional tomography may be a useful tool for understanding the anatomy of hiatal hernias and surgical planning of patients eligible for laparoscopic or robotic antireflux surgery. Surg Endosc 38, 780–786 (2024). https://doi.org/10.1007/s00464-023-10599-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10599-5