Abstract
Background
Hernias in patients with ascites are common, however we know very little about the surgical repair of hernias within this population. The study of these repairs has largely remained limited to single center and case studies, lacking a population-based study on the topic.
Study design
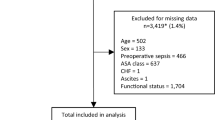
The Michigan Surgical Quality Collaborative and its corresponding Core Optimization Hernia Registry (MSQC-COHR) which captures specific patient, hernia, and operative characteristics at a population level within the state was used to conduct a retrospective review of patients with ascites undergoing ventral or inguinal hernia repair between January 1, 2020 and May 3, 2022. The primary outcome observed was incidence and surgical approach for both ventral and inguinal hernia cohorts. Secondary outcomes included 30-day adverse clinical outcomes as listed here: (ED visits, readmission, reoperation and complications) and surgical priority (urgent/emergent vs elective).
Results
In a cohort of 176 patients with ascites, surgical repair of hernias in patients with ascites is a rare event (1.4% in ventral hernia cohort, 0.2% in inguinal hernia cohort). The post-operative 30-day adverse clinical outcomes in both cohorts were greatly increased compared to those without ascites (ventral: 32% inguinal: 30%). Readmission was the most common complication in both inguinal (n = 14, 15.9%) and ventral hernia (n = 17, 19.3%) groups. Although open repair was most common for both cohorts (ventral: 86%, open: 77%), minimally invasive (MIS) approaches were utilized. Ventral hernias presented most commonly urgently/emergently (60%), and in contrast many inguinal hernias presented electively (72%).
Conclusion
A population-level, ventral and incisional hernia database capturing operative details for 176 patients with ascites. There was variation in the surgical approaches performed for this rare event and opportunities for optimization in patient selection and timing of repair.
Similar content being viewed by others
References
Telem DA, Schiano T, Divino CM (2010) Complicated hernia presentation in patients with advanced cirrhosis and refractory ascites: management and outcome. Surgery 148(3):538–543. https://doi.org/10.1016/j.surg.2010.01.002
Guo C, Liu Q, Wang Y, Li J (2020) Umbilical hernia repair in cirrhotic patients with ascites: a systemic review of literature. Surg Laparosc Endosc Percutan Tech. https://doi.org/10.1097/SLE.0000000000000891
Ecker BL et al (2014) Hernia repair in the presence of ascites. J Surg Res 190(2):471–477. https://doi.org/10.1016/j.jss.2014.05.039
Wang H, Fu J, Qi X, Sun J, Chen Y (2019) Laparoscopic totally extraperitoneal (TEP) inguinal hernia repair in patients with liver cirrhosis accompanied by ascites. Medicine 98(43):e17078. https://doi.org/10.1097/MD.0000000000017078
Li J, Qin C, Lai D, Hu Y, Wang L (2020) Safety and effectiveness of inguinal hernia repair in patients with liver cirrhosis: a retrospective study and literature review. Hernia 24(3):489–494. https://doi.org/10.1007/s10029-019-02087-4
Englesbe MJ, Dimick JB, Sonnenday CJ, Share DA, Campbell DAJ (2007) The Michigan surgical quality collaborative: will a statewide quality improvement initiative pay for itself? Ann Surg 246(6):1100–1103. https://doi.org/10.1097/SLA.0b013e31815c3fe5
Poulose BK et al (2012) Epidemiology and cost of ventral hernia repair: making the case for hernia research. Hernia 16(2):179–183. https://doi.org/10.1007/s10029-011-0879-9
Brooks DC (2023) Overview of treatment for inguinal and femoral hernia in adults. UpToDate. https://www.uptodate.com/contents/overview-of-treatment-for-inguinal-and-femoral-hernia-in-adults/print?search=incidence%20inguinal%20hernia&source=search_result&selectedTitle=3~114&usage_type=default&display_rank=3. Accessed 26 Jan 2023
Weyhe D, Tabriz N, Sahlmann B, Uslar V-N (2017) Risk factors for perioperative complications in inguinal hernia repair—a systematic review. Innov Surg Sci 2(2):47–52. https://doi.org/10.1515/iss-2017-0008
Howard R et al (2021) Hospital and surgeon variation in 30-day complication rates after ventral hernia repair. Am J Surg 222(2):417–423. https://doi.org/10.1016/j.amjsurg.2020.12.021
Simons MP et al (2018) International guidelines for groin hernia management. Hernia 22(1):1–165. https://doi.org/10.1007/s10029-017-1668-x
Juo Y-Y, Skancke M, Holzmacher J, Amdur RL, Lin PP, Vaziri K (2017) Laparoscopic versus open ventral hernia repair in patients with chronic liver disease. Surg Endosc 31(2):769–777. https://doi.org/10.1007/s00464-016-5031-6
Kykalos S, Machairas N, Ntikoudi E, Dorovinis P, Molmenti EP, Sotiropoulos GC (2021) Inguinal hernias in cirrhotic patients: from diagnosis to treatment. Surg Innov 28(5):620–627. https://doi.org/10.1177/1553350621995058
Marsman HA, Heisterkamp J, Halm JA, Tilanus HW, Metselaar HJ, Kazemier G (2007) Management in patients with liver cirrhosis and an umbilical hernia. Surgery 142(3):372–375. https://doi.org/10.1016/j.surg.2007.05.006
Funding
Agency for Healthcare Research and Quality, K08HS025778-01A1, Dana Telem.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Justin Dimick—a cofounder of ArborMetrix, Inc, Dana A Telem—Consulting fees from Medtronic. Devon Cassidy, Zhihong Shao, Ryan Howard, Michael Englesbe, Justin Dimick, Dana A Telem, Anne P Ehlers have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cassidy, D.E., Shao, Z., Howard, R. et al. Variability in surgical approaches to hernias in patients with ascites. Surg Endosc 38, 735–741 (2024). https://doi.org/10.1007/s00464-023-10598-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10598-6