Abstract
Background
Studies have demonstrated that the learning curve plays an important role in robotic pancreatoduodenectomy (RPD). Although improved short-term outcomes of RPD after the learning curve have been reported compared to open pancreatoduodenectomy (OPD), there is a lack of long-term survival analyses.
Methods
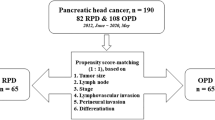
Patients who underwent curative intended RPD and OPD for pancreatic duct adenocarcinoma (PDAC) between January 2017 and June 2020 were retrospectively reviewed. A 1:2 propensity score matching (PSM) analysis was performed to balance the baseline characteristics between the RPD and OPD groups.
Results
Of the 548 patients (108 RPD and 440 OPD), 103 RPD patients were matched with 206 OPD patients after PSM. There were 194 (62.8%) men and 115 (37.2%) women, with a median age of 64 (58–69) years. The median overall survival (OS) in the RPD group was 33.2 months compared with 25.7 months in the OPD group (p = 0.058, log-rank). The median disease-free survival (DFS) following RPD was longer than the OPD (18.5 vs. 14.0 months, p = 0.011, log-rank). The RPD group has a lower incidence of local recurrence compared the OPD group (36.9% vs. 51.2%, p = 0.071). Multivariate Cox analysis demonstrated that RPD was independently associated with improved OS (HR 0.70, 95% CI 0.52–0.94, p = 0.019) and DFS (HR 0.66, 95% CI 0.50–0.88, p = 0.005).
Conclusion
After the learning curve, RPD had improved oncologic outcomes in PDAC patients compared to OPD. Future prospective randomized clinical trials will be required to validate these findings.


Similar content being viewed by others
References
Park W, Chawla A, O’Reilly EM (2021) Pancreatic cancer: a review. JAMA 326:851–862
Cameron JL, Riall TS, Coleman J, Belcher KA (2006) One thousand consecutive pancreaticoduodenectomies. Ann Surg 244:10–15
Kimura W, Miyata H, Gotoh M, Hirai I, Kenjo A, Kitagawa Y, Shimada M, Baba H, Tomita N, Nakagoe T, Sugihara K, Mori M (2014) A pancreaticoduodenectomy risk model derived from 8575 cases from a national single-race population (Japanese) using a web-based data entry system: the 30-day and in-hospital mortality rates for pancreaticoduodenectomy. Ann Surg 259:773–780
He J, Ahuja N, Makary MA, Cameron JL, Eckhauser FE, Choti MA, Hruban RH, Pawlik TM, Wolfgang CL (2014) 2564 resected periampullary adenocarcinomas at a single institution: trends over three decades. HPB (Oxford) 16:83–90
Wang M, Li D, Chen R, Huang X, Li J, Liu Y, Liu J, Cheng W, Chen X, Zhao W, Li J, Tan Z, Huang H, Li D, Zhu F, Qin T, Ma J, Yu G, Zhou B, Zheng S, Tang Y, Han W, Meng L, Ke J, Feng F, Chen B, Yin X, Chen W, Ma H, Xu J, Liu Y, Lin R, Dong Y, Yu Y, Liu J, Zhang H, Qin R (2021) Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours: a multicentre, open-label, randomised controlled trial. Lancet Gastroenterol Hepatol 6:438–447
Zhang Z, Yin T, Qin T, Pan S, Wang M, Zhang H, Qin R (2022) Comparison of laparoscopic versus open pancreaticoduodenectomy in patients with resectable pancreatic ductal adenocarcinoma: a propensity score-matching analysis of long-term survival. Pancreatology 22:317–324
van Hilst J, de Rooij T, Bosscha K, Brinkman DJ, van Dieren S, Dijkgraaf MG, Gerhards MF, de Hingh IH, Karsten TM, Lips DJ, Luyer MD, Busch OR, Festen S, Besselink MG, Van Hilst J, De Rooij T, Bosscha K, Brinkman DJ, Van Dieren S, Dijkgraaf MG, Gerhards MF, De Hingh IH, Karsten TM, Lips DJ, Luyer MD, Busch OR, Festen S, Besselink MG, Marsman HA, Van Gulik TM, Wicherts DA, Eshuis WJ, Stibbe LA, Nieveen van Dijkum EJM, Van Hooft JE, Fockens P, Van Laarhoven HW, Wilmink JW, Van de Vijver MJ, Bijlsma MF, Verheij J, Nio CY, Van Lienden KP, Van Tienhoven G, Schoorlemmer A, Creemers G-J, Van Eijck CHJ, Groot Koerkamp B, Bruno MJ, Eskens F, Nuyttens JJ, Pek C, Van der Schelling GP, Seerden TC, Patijn GA, Nieuwenhuijs VB, De Groot JW, Bonsing BA, Vahrmeijer A, Swijnenburg RJ, Mieog JSD, Van der Harst E, Den Dulk M, Olde Damink S, Dejong CHC, Van Dam R, De Vos JM, Liem MSL, Van Laarhoven CJHM, Van Goor H, Van den Boezem PB, Van der Kolk BM, Stommel MWJ, Hermans JJ, Van Geenen EJM, Radema SA, Brosens LA, Scheepers JJG, Roos D, Boerma D, Te Riele W, Van Santvoort HC, Bollen TL, Wit F, Molenaar IQ, Haj Mohammad N, Van Leeuwen MS, Roele A, De Jong KP, De Meijer VE, Klaase JM, Kazemier G, Zonderhuis B, Daams F, Meijerink MR, Latenstein A, Van Rijssen LB, Nota C, Van Halsema E, Van Veldhuisen E, Vogel J, Janssen K, Scholten L, Daamen L, Walma M, Strijker M, Prins M, Zwart M, Suker M, Rombouts S, Mungroop T, Vissers F, Korrel M (2019) Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): a multicentre, patient-blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol Hepatol 4:199–207
Giulianotti PC, Mangano A, Bustos RE, Gheza F, Fernandes E, Masrur MA, Gangemi A, Bianco FM (2018) Operative technique in robotic pancreaticoduodenectomy (RPD) at University of Illinois at Chicago (UIC): 17 steps standardized technique: lessons learned since the first worldwide RPD performed in the year 2001. Surg Endosc 32:4329–4336
Kim HS, Kim H, Han Y, Lee M, Kang YH, Sohn HJ, Kang JS, Kwon W, Jang JY (2022) ROBOT-assisted pancreatoduodenectomy in 300 consecutive cases: annual trend analysis and propensity score-matched comparison of perioperative and long-term oncologic outcomes with the open method. J Hepatobiliary Pancreat Sci 29:301–310
Girgis MD, Zenati MS, King JC, Hamad A, Zureikat AH, Zeh HJ, Hogg ME (2021) Oncologic outcomes after robotic pancreatic resections are not inferior to open surgery. Ann Surg 274:e262–e268
Liu Q, Zhao Z, Zhang X, Wang W, Han B, Chen X, Tan X, Xu S, Zhao G, Gao Y, Gan Q, Yuan J, Ma Y, Dong Y, Liu Z, Wang H, Fan F, Liu J, Lau WY, Liu R (2021) Perioperative and oncological outcomes of robotic versus open pancreaticoduodenectomy in low-risk surgical candidates: a multicenter propensity score-matched study. Ann Surg 277:e864–e871
McMillan MT, Zureikat AH, Hogg ME, Kowalsky SJ, Zeh HJ, Sprys MH, Vollmer CM Jr (2017) A propensity score-matched analysis of robotic vs open pancreatoduodenectomy on incidence of pancreatic fistula. JAMA Surg 152:327–335
Asbun HJ, Moekotte AL, Vissers FL, Kunzler F, Cipriani F, Alseidi A, D’Angelica MI, Balduzzi A, Bassi C, Bjornsson B, Boggi U, Callery MP, Del Chiaro M, Coimbra FJ, Conrad C, Cook A, Coppola A, Dervenis C, Dokmak S, Edil BH, Edwin B, Giulianotti PC, Han HS, Hansen PD, van der Heijde N, van Hilst J, Hester CA, Hogg ME, Jarufe N, Jeyarajah DR, Keck T, Kim SC, Khatkov IE, Kokudo N, Kooby DA, Korrel M, de Leon FJ, Lluis N, Lof S, Machado MA, Demartines N, Martinie JB, Merchant NB, Molenaar IQ, Moravek C, Mou YP, Nakamura M, Nealon WH, Palanivelu C, Pessaux P, Pitt HA, Polanco PM, Primrose JN, Rawashdeh A, Sanford DE, Senthilnathan P, Shrikhande SV, Stauffer JA, Takaori K, Talamonti MS, Tang CN, Vollmer CM, Wakabayashi G, Walsh RM, Wang SE, Zinner MJ, Wolfgang CL, Zureikat AH, Zwart MJ, Conlon KC, Kendrick ML, Zeh HJ, Hilal MA, Besselink MG, International Study Group on Minimally Invasive Pancreas S (2020) The Miami International Evidence-based guidelines on minimally invasive pancreas resection. Ann Surg 271:1–14
Watkins AA, Kent TS, Gooding WE, Boggi U, Chalikonda S, Kendrick ML, Walsh RM, Zeh HJ 3rd, Moser AJ (2018) Multicenter outcomes of robotic reconstruction during the early learning curve for minimally-invasive pancreaticoduodenectomy. HPB (Oxford) 20:155–165
Shi Y, Wang W, Qiu W, Zhao S, Wang J, Weng Y, Huo Z, Jin J, Wang Y, Deng X, Shen B, Peng C (2021) Learning curve from 450 cases of robot-assisted pancreaticoduocectomy in a high-volume pancreatic center: optimization of operative procedure and a retrospective study. Ann Surg 274:e1277–e1283
Papageorge MV, de Geus SWL, Woods AP, Ng SC, McAneny D, Tseng JF, Kenzik KM, Sachs TE (2022) The effect of hospital versus surgeon volume on short-term patient outcomes after pancreaticoduodenectomy: a SEER-medicare analysis. Ann Surg Oncol 29:2444–2451
Shi Y, Jin J, Qiu W, Weng Y, Wang J, Zhao S, Huo Z, Qin K, Wang Y, Chen H, Deng X, Peng C, Shen B (2020) Short-term outcomes after robot-assisted vs open pancreaticoduodenectomy after the learning curve. JAMA Surg 155:389–394
Chen H, Wang W, Ying X, Deng X, Peng C, Cheng D, Shen B (2020) Predictive factors for postoperative pancreatitis after pancreaticoduodenectomy: a single-center retrospective analysis of 1465 patients. Pancreatology 20:211–216
Tol JA, Gouma DJ, Bassi C, Dervenis C, Montorsi M, Adham M, Andren-Sandberg A, Asbun HJ, Bockhorn M, Buchler MW, Conlon KC, Fernandez-Cruz L, Fingerhut A, Friess H, Hartwig W, Izbicki JR, Lillemoe KD, Milicevic MN, Neoptolemos JP, Shrikhande SV, Vollmer CM, Yeo CJ, Charnley RM, International Study Group on Pancreatic S (2014) Definition of a standard lymphadenectomy in surgery for pancreatic ductal adenocarcinoma: a consensus statement by the International Study Group on Pancreatic Surgery (ISGPS). Surgery 156:591–600
Fu N, Qin K, Li J, Jin J, Jiang Y, Deng X, Shen B (2022) Who could complete and benefit from the adjuvant chemotherapy regarding pancreatic ductal adenocarcinoma? A multivariate-adjusted analysis at the pre-adjuvant chemotherapy timing. Cancer Med 11:3397–3406
Zureikat AH, Moser AJ, Boone BA, Bartlett DL, Zenati M, Zeh HJ 3rd (2013) 250 robotic pancreatic resections: safety and feasibility. Ann Surg 258:554–559 (discussion 559-562)
Lai EC, Yang GP, Tang CN (2012) Robot-assisted laparoscopic pancreaticoduodenectomy versus open pancreaticoduodenectomy: a comparative study. Int J Surg 10:475–479
Vining CC, Kuchta K, Schuitevoerder D, Paterakos P, Berger Y, Roggin KK, Talamonti MS, Hogg ME (2020) Risk factors for complications in patients undergoing pancreaticoduodenectomy: a NSQIP analysis with propensity score matching. J Surg Oncol 122:183–194
Rosemurgy A, Ross S, Bourdeau T, Craigg D, Spence J, Alvior J, Sucandy I (2019) Robotic pancreaticoduodenectomy is the future: here and now. J Am Coll Surg 228:613–624
Weng Y, Jiang Y, Fu N, Jin J, Shi Y, Huo Z, Deng X, Peng C, Shen B (2021) Oncological outcomes of robotic-assisted versus open pancreatoduodenectomy for pancreatic ductal adenocarcinoma: a propensity score-matched analysis. Surg Endosc 35:3437–3448
Mirkin KA, Greenleaf EK, Hollenbeak CS, Wong J (2018) Minimally invasive surgical approaches offer earlier time to adjuvant chemotherapy but not improved survival in resected pancreatic cancer. Surg Endosc 32:2387–2396
Chan JWY, Yu PSY, Yang JH, Yuan EQ, Jia H, Peng J, Lau RWH, Ng CSH (2020) Surgical access trauma following minimally invasive thoracic surgery. Eur J Cardiothorac Surg 58:i6–i13
Sammour T, Kahokehr A, Chan S, Booth RJ, Hill AG (2010) The humoral response after laparoscopic versus open colorectal surgery: a meta-analysis. J Surg Res 164:28–37
Lyu Y, Cheng Y, Wang B, Zhao S, Chen L (2020) Comparison of 3 minimally invasive methods versus open distal pancreatectomy: a systematic review and network meta-analysis. Surg Laparosc Endosc Percutan Tech 31:104–112
Qu L, Zhiming Z, Xianglong T, Yuanxing G, Yong X, Rong L, Yee LW (2018) Short- and mid-term outcomes of robotic versus laparoscopic distal pancreatosplenectomy for pancreatic ductal adenocarcinoma: a retrospective propensity score-matched study. Int J Surg 55:81–86
Lof S, van der Heijde N, Abuawwad M, Al-Sarireh B, Boggi U, Butturini G, Capretti G, Coratti A, Casadei R, D’Hondt M, Esposito A, Ferrari G, Fusai G, Giardino A, Groot Koerkamp B, Hackert T, Kamarajah S, Kauffmann EF, Keck T, Marudanayagam R, Nickel F, Manzoni A, Pessaux P, Pietrabissa A, Rosso E, Salvia R, Soonawalla Z, White S, Zerbi A, Besselink MG, Abu Hilal M, European Consortium on Minimally Invasive Pancreatic S (2021) Robotic versus laparoscopic distal pancreatectomy: multicentre analysis. Br J Surg 108:188–195
Topal H, Aerts R, Laenen A, Collignon A, Jaekers J, Geers J, Topal B (2022) Survival after minimally invasive vs open surgery for pancreatic adenocarcinoma. JAMA Netw Open 5:e2248147
Funding
None.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
Haoda Chen, Yuanchi Weng, Shulin Zhao, Weishen Wang, Yuchen Ji, Chenghong Peng, Xiaxing Deng, and Baiyong Shen have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, H., Weng, Y., Zhao, S. et al. Robotic versus open pancreatoduodenectomy in patients with pancreatic duct adenocarcinoma after the learning curve: a propensity score-matched analysis. Surg Endosc 38, 821–829 (2024). https://doi.org/10.1007/s00464-023-10530-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10530-y