Abstract
Background
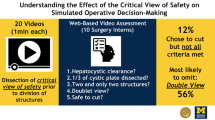
A novel 6-item objective, procedure-specific assessment for laparoscopic cholecystectomy incorporating the critical view of safety (LC-CVS OPSA) was developed to support trainee formative and summative assessments. The LC-CVS OPSA included two retraction items (fundus and infundibulum retraction) and four CVS items (hepatocystic triangle visualization, gallbladder-liver separation, cystic artery identification, and cystic duct identification). The scoring rubric for retraction consisted of poor (frequently outside of defined range), adequate (minimally outside of defined range) and excellent (consistently inside defined range) and for CVS items were “poor—unsafe”, “adequate—safe”, or “excellent—safe”.
Methods
A multi-national consortium of 12 expert LC surgeons applied the OPSA—LC CVS to 35 unique LC videos and one duplicate video. Primary outcome measure was inter-rater reliability as measured by Gwet’s AC2, a weighted measure that adjusts for scales with high probability of random agreement. Analysis of the inter-rater reliability was conducted on a collapsed dichotomous scoring rubric of “poor—unsafe” vs. “adequate/excellent—safe”.
Results
Inter-rater reliability was high for all six items ranging from 0.76 (hepatocystic triangle visualization) to 0.86 (cystic duct identification). Intra-rater reliability for the single duplicate video was substantially higher across the six items ranging from 0.91 to 1.00.
Conclusions
The novel 6-item OPSA LC CVS demonstrated high inter-rater reliability when tested with a multi-national consortium of LC expert surgeons. This brief instrument focused on safe surgical practice was designed to support the implementation of entrustable professional activities into busy surgical training programs. Instrument use coupled with video-based assessments creates novel datasets with the potential for artificial intelligence development including computer vision to drive assessment automation.
Graphical abstract



Similar content being viewed by others
References
Lindeman B, Petrusa E, Phitayakorn R (2017) Entrustable professional activities (EPAs) and applications to surgical training. Am Coll Surg. https://www.facs.org/for-medical-professionals/news-publications/journals/rise/articles/entrustable/. Accessed 1 Mar 2023
Frank JR, Snell LS, Cate OT, Holmboe ES, Carraccio C, Swing SR, Harris P, Glasgow NJ, Campbell C, Dath D, Harden RM, Iobst W, Long DM, Mungroo R, Richardson DL, Sherbino J, Silver I, Taber S, Talbot M, Harris KA (2010) Competency-based medical education: theory to practice. Med Teach. https://doi.org/10.3109/0142159X.2010.501190
Singh P, Aggarwal R, Zevin B, Grantcharov T, Darzi A (2014) A global Delphi consensus study on defining and measuring quality in surgical training. J Am Coll Surg. https://doi.org/10.1016/j.jamcollsurg.2014.03.051
Huang RJ, Limsui D, Triadafilopoulos G (2018) Video-based performance assessment in endoscopy: moving beyond “see one, do one, teach one”. Gastrointest Endosc. https://doi.org/10.1016/j.gie.2017.09.014
Ibrahim AM, Varban OA, Dimick JB (2016) Novel uses of video to accelerate the surgical learning curve. J Laparoendosc Adv Surg Tech A. https://doi.org/10.1089/lap.2016.0100
Ducournau F, Meyer N, Xavier F, Facca S, Liverneaux P (2021) Learning a MIPO technique for distal radius fractures: mentoring versus simple experience versus deliberate practice. Orthop Traumatol Surg Res. https://doi.org/10.1016/j.otsr.2021.102939
Missori G, Serra F, Gelmini R (2022) A narrative review about difficult laparoscopic cholecystectomy: technical tips. Laparosc Surg. https://doi.org/10.21037/ls-22-16
Strasberg SM (2017) A perspective on the critical view of safety in laparoscopic cholecystectomy. Ann Laparosc Endosc Surg. https://doi.org/10.21037/ales.2017.04.08
Kapoor VK (2016) Medico-legal aspects of bile duct injury. J Minim Access Surg. https://doi.org/10.4103/0972-9941.169995
Flum DR, Cheadle A, Prela C, Dellinger EP, Chan L (2003) Bile duct injury during cholecystectomy and survival in Medicare beneficiaries. JAMA. https://doi.org/10.1001/jama.290.16.2168
Bektas H, Schrem H, Winny M, Klempnauer J (2007) Surgical treatment and outcome of iatrogenic bile duct lesions after cholecystectomy and the impact of different clinical classification systems. Br J Surg. https://doi.org/10.1002/bjs.5752
Brunt LM, Deziel DJ, Telem DA, Strasberg SM, Aggarwal R, Asbun H, Bonjer J, McDonald M, Alseidi A, Ujiki M, Riall TS, Hammill C, Moulton C-A, Pucher PH, Parks RW, Ansari MT, Connor S, Dirks RC, Anderson B, Altieri MS, Tsamalaidze L, Stefanidis D (2020) Safe cholecystectomy multi-society practice guideline and state of the art consensus conference on prevention of bile duct injury during cholecystectomy. Ann Surg. https://doi.org/10.1097/sla.0000000000003791
Wakabayashi G, Iwashita Y, Hibi T, Takada T, Strasberg SM, Asbun HJ, Endo I, Umezawa A, Asai K, Suzuki K, Mori Y, Okamoto K, Pitt HA, Han H-S, Hwang T-L, Yoon Y-S, Yoon D-S, Choi I-S, Huang WS-W, Giménez ME, Garden OJ, Gouma DJ, Belli G, Dervenis C, Jagannath P, Chan AC, Lau WY, Liu K-H, Su C-H, Misawa T, Nakamura M, Horiguchi A, Tagaya N, Fujioka S, Higuchi R, Shikata S, Noguchi Y, Ukai T, Yokoe M, Cherqui D, Honda G, Sugioka A, de Santibañes E, Supe AN, Tokumura H, Kimura T, Yoshida M, Mayumi T, Kitano S, Inomata M, Hirata K, Sumiyama Y, Inui K, Yamamoto M (2018) Tokyo guidelines 2018: surgical management of acute cholecystitis: safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. https://doi.org/10.1002/jhbp.517
Eikermann M, Siegel R, Broeders I, Dziri C, Fingerhut A, Gutt C, Jaschinski T, Nassar A, Paganini AM, Pieper D, Targarona E, Schrewe M, Shamiyeh A, Strik M, Neugebauer EA (2012) Prevention and treatment of bile duct injuries during laparoscopic cholecystectomy: the clinical practice guidelines of the European Association for Endoscopic Surgery (EAES). Surg Endosc. https://doi.org/10.1007/s00464-012-2511-1
Jin Y, Liu R, Chen Y, Liu J, Zhao Y, Wei A, Li Y, Li H, Xu J, Wang X, Li A (2022) Critical view of safety in laparoscopic cholecystectomy: a prospective investigation from both cognitive and executive aspects. Front Surg. https://doi.org/10.3389/fsurg.2022.946917
Deal SB, Alseidi AA (2017) Concerns of quality and safety in public domain surgical education videos: an assessment of the critical view of safety in frequently used laparoscopic cholecystectomy videos. J Am Coll Surg. https://doi.org/10.1016/j.jamcollsurg.2017.08.01
Nijssen MAJ, Schreinemakers JMJ, van der Schelling GP, Crolla RMPH, Rijken AM (2016) Improving critical view of safety in laparoscopic cholecystectomy by teaching interventions. J Surg Educ. https://doi.org/10.1016/j.jsurg.2015.11.015
Jung YK, Kwon YJ, Choi D, Lee KG (2016) What is the safe training to educate the laparoscopic cholecystectomy for surgical residents in early learning curve. J Minim Invasive Surg. https://doi.org/10.7602/jmis.2015.19.2.70
Nickel F, Hendrie JD, Stock C, Salama M, Preukschas AA, Senft JD, Kowalewski KF, Wagner M, Kenngott HG, Linke GR, Fischer L, Müller-Stich BP (2016) Direct observation versus endoscopic video recording-based rating with the objective structured assessment of technical skills for training of laparoscopic cholecystectomy. Eur Surg Res. https://doi.org/10.1159/000444449
Kramp KH, van Det MJ, Hoff C, Lamme B, Veeger NJGM, Pierie J-PEN (2015) Validity and reliability of global operative assessment of laparoscopic skills (goals) in novice trainees performing a laparoscopic cholecystectomy. J Surg Educ. https://doi.org/10.1016/j.jsurg.2014.08.006
Hatala R, Cook DA, Brydges R, Hawkins R (2015) Constructing a validity argument for the Objective Structured Assessment of Technical Skills (OSATS): a systematic review of validity evidence. Adv Health Sci Educ Theory Pract. https://doi.org/10.1007/s10459-015-9593-1
Kramp KH, van Det MJ, Veeger NJGM, Pieria J-PEN (2015) Validity, reliability and support for implementation of independence-scaled procedural assessment in laparoscopic surgery. Surg Endosc. https://doi.org/10.1007/s00464-015-4254-2
Glarner CE, McDonald RJ, Smith AB, Leverson GE, Peyre S, Pugh CM, Greenberg CC, Greenberg JA, Foley EF (2013) Utilizing a novel tool for the comprehensive assessment of resident operative performance. J Surg Educ. https://doi.org/10.1016/j.jsurg.2013.07.009
Adrales G, Ardito F, Chowbey P, Morales-Conde S, Ferreres AR, Hensman C, Martin D, Matthaei H, Ramshaw B, Roberts JK, Schrem H, Sharma A, Tabiri S, Vibert E, Woods MS (2023) A multi-national, video-based qualitative study to refine training guidelines for assigning an “unsafe” score in laparoscopic cholecystectomy critical view of safety (in press)
Caresyntax (2023) Platform. https://caresyntax.com/platform/. Accessed 1 Mar 2023
Gwet KL (2008) Computing inter-rater reliability and its variance in the presence of high agreement. Br J Math Stat Psychol. https://doi.org/10.1348/000711006x126600
Gwet KL (2014) Handbook of inter-rater reliability: the definitive guide to measuring the extent of agreement among raters, 4th edn. Advanced Analytics LLC, Gaithersburg
Wongpakaran N, Wongpakaran T, Wedding D, Gwet KL (2013) A comparison of Cohen’s Kappa and Gwet’s AC1 when calculating inter-rater reliability coefficients: a study conducted with personality disorder samples. BMC Med Res Methodol. https://doi.org/10.1186/1471-2288-13-61
Blood E, Spratt KF (2007) Disagreement on agreement: two alternative agreement coefficients, SAS Global Forum 2007. https://support.sas.com/resources/papers/proceedings/proceedings/forum2007/186-2007.pdf. Accessed 1 Mar 2023
Chevallay M, Liot E, Fournier I, Abbassi Z, Peloso A, Hagen ME, Mönig SP, Morel P, Toso C, Buchs N, Miskovic D, Ris F, Jung MK (2022) Implementation and validation of a competency assessment tool for laparoscopic cholecystectomy. Surg Endosc. https://doi.org/10.1007/s00464-022-09264-0
Van Zwieten TH, Okkema S, Kramp KH, de Jong K, Van Det MJ, Pierie J-PEN (2022) Procedure-based assessment for laparoscopic cholecystectomy can replace global rating scales. Minim Invasiv Ther Allied Technol. https://doi.org/10.1080/13645706.2021.1995000
Bethlehem MS, Kramp KH, van Det MJ, ten Cate Hoedemaker HO, Veeger NJ, Pierie JP (2014) Development of a standardized training course for laparoscopic procedures using Delphi methodology. J Surg Educ. https://doi.org/10.1016/j.jsurg.2014.04.009
Kramp KH, van Det MJ, Veeger NJGM, Pierie J-PEN (2015) Validity, reliability and support for implementation of independence-scaled procedural assessment in laparoscopic surgery. Surg Endosc. https://doi.org/10.1007/s00464-015-4254-2
Champagne BJ (2013) Effective teaching and feedback strategies in the OR and beyond. Clin Colon Rectal Surg. https://doi.org/10.1055/s-0033-1356725
American Board of Surgery (2022) Entrustable professional activities. https://www.absurgery.org/default.jsp?epahome. Accessed 1 Mar 2023
Stahl CC, Collins E, Jung SA, Rosser AA, Kraut AS, Schnapp BH, Westergaard M, Hamedani AG, Minter RM, Greenberg JA (2020) Implementation of entrustable professional activities into a general surgery residency. J Surg Educ. https://doi.org/10.1016/j.jsurg.2020.01.012
Brasel KJ, Klingensmith ME, Englander R, Grambau M, Buyske J, Sarosi G, Minter R (2019) Entrustable professional activities in general surgery: development and implementation. J Surg Educ. https://doi.org/10.1016/j.jsurg.2019.04.003
Vedula SS, Ishii M, Hager GD (2017) Objective assessment of surgical technical skill and competency in the operating room. Annu Rev Biomed Eng. https://doi.org/10.1146/annurev-bioeng-071516-044435
Egert M, Steward JE, Sundaram CP (2020) Machine learning and artificial intelligence in surgical fields. Indian J Surg Oncol. https://doi.org/10.1007/s13193-020-01166-8
Hashimoto DA, Rosman G, Witkowski ER, Stafford C, Navarette-Welton AJ, Rattner DW, Lillemoe KD, Rus DL, Meireles OR (2019) Computer vision analysis of intraoperative video: automated recognition of operative steps in laparoscopic sleeve gastrectomy. Ann Surg. https://doi.org/10.1097/sla.0000000000003460
Mascagni P, Alapatt D, Urade T, Vardazaryan A, Mutter D, Marescaux J, Costamagna G, Dallemagne B, Padoy N (2021) A computer vision platform to automatically locate critical events in surgical videos: documenting safety in laparoscopic cholecystectomy. Ann Surg. https://doi.org/10.1097/SLA.0000000000004736
Vedula SS, Hager GD (2017) Surgical data science: the new knowledge domain. Innov Surg Sci. https://doi.org/10.1515/iss-2017-0004
Watanabe Y, Bilgic E, Lebedeva E, McKendy KM, Feldman LS, Fried GM, Vassiliou MC (2016) A systematic review of performance assessment tools for laparoscopic cholecystectomy. Surg Endosc. https://doi.org/10.1007/s00464-015-4285-8
Acknowledgements
The authors wish to thank Justin Smith for analytical support and Health Analytics, LLC for administrative and medical writing support in preparing the manuscript.
Funding
This work was supported by Caresyntax sponsored this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Adrales reported receipt of support for this manuscript and consulting fees from Caresyntax. Ardito reported receipt of support for this manuscript, consulting fees, payment or honoraria, participation on a data safety monitoring or advisory board and a leadership or fiduciary role on a review board with Caresyntax. Chowbey and Matthaei reported receipt of support for this manuscript from Caresyntax. Morales-Conde, Ferreres, and Martin reported receipt of support for this manuscript and payment or honoraria from Caresyntax. Hensman reported receipt of support for this manuscript, payment or honoraria and participation on a data safety monitoring or advisory board with Caresyntax. Ramshaw, Schrem, Sharma, Tabiri, and Vibert reported receipt of support for this manuscript, consulting fees and payment or honoraria from Caresyntax. Woods is an employee of Caresyntax.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Adrales, G., Ardito, F., Chowbey, P. et al. Laparoscopic cholecystectomy critical view of safety (LC-CVS): a multi-national validation study of an objective, procedure-specific assessment using video-based assessment (VBA). Surg Endosc 38, 922–930 (2024). https://doi.org/10.1007/s00464-023-10479-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10479-y