Abstract
Background
Patient engagement technologies (PET) are an area of growing innovation and investment, but whether PET use in the setting of electronic medical record (EMR) supported patient portals are associated with improved outcomes is unknown. Therefore, we assessed PET and EMR activation among patients undergoing elective colorectal surgery on an enhanced recovery pathway.
Methods
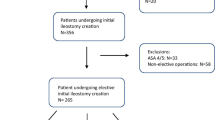
We identified adults undergoing elective colorectal surgery between 1/2017 and 7/2021. EMR activations were assessed and patients were considered PET users if they used a proprietary PET application. Multivariable logistic regression was used to identify factors associated with PET use and determine whether the level of engagement (percentage of messages read by the patient) was associated with 30-day outcomes.
Results
484 patients (53.5% PET users, 81.6% with an activated EMR patient portal, 30.8% ≥ 70 years of age) were included. PET users were younger, more likely to have their EMR portal activated and had decreased odds of prolonged length of stay [odds ratio (OR) 0.5, 95% confidence interval (CI) 0.4–0.8]. Among patients ≥ 70 years, PET users had reduced odds of readmissions (OR 0.2, 95% CI 0.1–0.9) compared to PET non-users. The most engaged PET users had decreased morbidity (OR 0.2, 95% CI 0.1–0.8) and readmissions (OR 0.3, 95% CI 0.1–0.8) compared to the least engaged PET users.
Conclusion
When controlling for EMR activation, patients who use PET, specifically those with higher levels of engagement or aged ≥ 70, have improved outcomes following elective colorectal surgery. Interventions aimed at increasing the adoption of PET among older adults may be warranted.





Similar content being viewed by others
References
Stitzenberg KB, Chang Y, Smith AB, Nielsen ME (2015) Exploring the burden of inpatient readmissions after major cancer surgery. J Clin Oncol 33:455–464
Wick EC, Shore AD, Hirose K, Ibrahim AM, Gearhart SL, Efron J et al (2011) Readmission rates and cost following colorectal surgery. Dis Colon Rectum 54:1475–1479
Guinier D, Mantion GA, Alves A, Kwiatkowski F, Slim K, Panis Y (2007) Risk factors of unplanned readmission after colorectal surgery: a prospective, multicenter study. Dis Colon Rectum 50:1316–1323
Keng CJS, Goriawala A, Rashid S, Goldstein R, Schmocker S, Easson A et al (2020) Home to stay: an integrated monitoring system using a mobile app to support patients at home following colorectal surgery. J Patient Exp 7:1241–1246
Smithson M, McLeod MC, Theiss L, Shao C, Kennedy G, Hollis R et al (2022) Ileostomy patients using patient engagement technology experience decreased length of stay. J Gastrointest Surg 26:635–642
Borsuk DJ, Al-Khamis A, Geiser AJ, Zhou D, Warner C, Kochar K et al (2019) S128: active post discharge surveillance program as a part of enhanced recovery after surgery protocol decreases emergency department visits and readmissions in colorectal patients. Surg Endosc 33:3816–3827
Symer MM, Abelson JS, Milsom J, McClure B, Yeo HL (2017) A mobile health application to track patients after gastrointestinal surgery: results from a pilot study. J Gastrointest Surg 21:1500–1505
Baldwin JL, Singh H, Sittig DF, Giardina TD (2017) Patient portals and health apps: pitfalls, promises, and what one might learn from the other. Healthcare (Amsterdam) 5:81–85
Diez Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ et al (2001) Neighborhood of residence and incidence of coronary heart disease. N Engl J Med 345:99–106
Nelson Kakulla B (2020) Older adults keep pace on tech usage. 2020 Tech Trends of the 50+. AARP Research, Washington, DC
Centers for Disease Control (2010) National hospital discharge survey: number of all-listed procedures for discharges from short-stay hospitals, by procedure category and age: United States. Centers for Disease Control, Atlanta
Rural Health Information Hub. (2010) Demographic changes and aging population. Rural Health Information Hub., Grand Forks
Gajdos C, Kile D, Hawn MT, Finlayson E, Henderson WG, Robinson TN (2013) Advancing age and 30-day adverse outcomes after nonemergent general surgeries. J Am Geriatr Soc 61:1608–1614
Irfan A, Lever JM, Fouad MN, Sleckman BP, Smith H, Chu DI et al (2022) Does health literacy impact technological comfort in cancer patients? Am J Surg 223:722–728
Theiss LM, Wood L, Shao C, Marques I, Kim DH, Hollis R et al (2023) Disparities in perioperative use of patient engagement technologies—not all use is equal. Ann Surg 277:e218–e225
Brown CS, Yang J, Meng Z, Henderson J, Dimick JB, Telem DA (2020) Trends in emergency department utilization following common operations in New York State, 2005–2014. Surg Endosc 34:1994–1999
Acknowledgements
None.
Funding
The authors received no funding for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Fergal J. Fleming receives author royalties from UpToDate, Inc. Larissa K. Temple is a recipient of Patient Centered Outcomes Research Institute (PCORI) research award (HIS-1602-34355) and the Agency for Healthcare Research and Quality (AHRQ) Grant [1R18HS026189-01A1]. Alexa D. Melucci, Kiersten Flodman, Anthony Loria, Holli L. Swanson, Mary K. Robinson, Michael J. Hasselberg, and Lara Evans have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Disclosure: Preliminary data from this manuscript was presented at the American College of Surgeons National Surgical Quality Improvement Program Quality and Safety Conference, July 15–17, 2022.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Melucci, A.D., Flodman, K., Loria, A. et al. Is there an outcome benefit? Patient engagement technology in addition to the electronic medical record patient portal following elective colorectal surgery. Surg Endosc 37, 9275–9282 (2023). https://doi.org/10.1007/s00464-023-10478-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10478-z