Abstract
Background
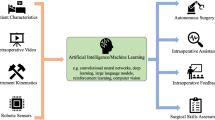
Robot-assisted surgery is today well-implemented in many surgical specialties, but requires another skill set than laparoscopy. Most often, robot-assisted surgery is considered add-on to laparoscopic skills but very little is known about the transfer of skills. The aim of the study was to examine to what extent surgical skills are transferable between laparoscopic and robot-assisted surgery.
Methods
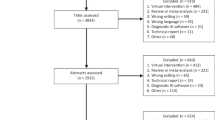
A systematic search was conducted in three databases (Ovid Medline, Embase, and Web of Science). Studies investigating transfer of skills between laparoscopy and robot-assisted surgery in either a phantom-based, simulation-based, animal model, or clinical setting were eligible for inclusion. Quality assessment was done using the Medical education research study quality instrument and educational New Ottawa Scale.
Results
Of 15,610 studies identified, 89 studies continued to full-text reading, and 37 studies were included. Four studies were found non-comparable and were left out of the results for the primary outcome. All 33 studies explored transfer from laparoscopy to robot-assisted surgery and 17 found a positive transfer whereas 15 did not. Only 11 studies explored transfer from robot-assisted surgery to laparoscopy, of which only three found a positive transfer.
Conclusion
An almost equal number of publications found a positive transfer and no transfer from laparoscopic to robot-assisted surgery. Fewer studies explored the transfer from robot-assisted surgery to laparoscopy. Very little evidence supports that surgeons trained solely in robot-assisted surgery can perform laparoscopy. This must be considered in future training programs as robot-assisted surgery is expected to become the first-in-line modality for many future surgeons.




Similar content being viewed by others
References
Figert PL, Park AE, Witzke DB et al (2001) Transfer of training in acquiring laparoscopic skills. J Am Coll Surg 193:533–537. https://doi.org/10.1016/s1072-7515(01)01069-9
Brown DC, Miskovic D, Tang B et al (2010) Impact of established skills in open surgery on the proficiency gain process for laparoscopic surgery. Surg Endosc 24:1420–1426. https://doi.org/10.1007/s00464-009-0792-9
Corcione F, Esposito C, Cuccurullo D et al (2005) Advantages and limits of robot-assisted laparoscopic surgery: preliminary experience. Surg Endosc 19:117–119. https://doi.org/10.1007/s00464-004-9004-9
Reznick RK, MacRae H (2006) Teaching surgical skills—changes in the wind. N Engl J Med 355:2664–2669. https://doi.org/10.1056/NEJMra054785
Hertz P, Houlind K, Jepsen J et al (2022) Identifying curriculum content for a cross-specialty robotic-assisted surgery training program: a Delphi study. Surg Endosc 36:4786–4794. https://doi.org/10.1007/s00464-021-08821-3
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Gordon M, Gibbs T (2014) STORIES statement: publication standards for healthcare education evidence synthesis. BMC Med 12:143. https://doi.org/10.1186/s12916-014-0143-0
National Institute for Heath and Care Research. PROSPERO—International prospective register of systematic reviews. https://www.crd.york.ac.uk/prospero/. Accessed 28 Nov 2021
McKeown S, Mir ZM (2021) Considerations for conducting systematic reviews: evaluating the performance of different methods for de-duplicating references. Syst Rev 10:38. https://doi.org/10.1186/s13643-021-01583-y
Cook DA, Levinson AJ, Garside S (2011) Method and reporting quality in health professions education research: a systematic review. Med Educ 45:227–238. https://doi.org/10.1111/j.1365-2923.2010.03890.x
Cook DA, Reed DA (2015) Appraising the quality of medical education research methods: the Medical Education Research Study Quality Instrument and the Newcastle-Ottawa Scale-Education. Acad Med 90:1067–1076. https://doi.org/10.1097/ACM.0000000000000786
Zihni A, Ge T, Ray S et al (2016) Transfer and priming of surgical skills across minimally invasive surgical platforms. J Surg Res 206:48–52. https://doi.org/10.1016/j.jss.2016.06.026
Vurgun N, Vongsurbchart T, Myszka A et al (2021) Medical student experience with robot-assisted surgery after limited laparoscopy exposure. J Robot Surg 15:443–450. https://doi.org/10.1007/s11701-020-01129-9
Chang Y, Qu M, Wang L et al (2016) Robotic-assisted laparoscopic radical prostatectomy from a single Chinese center: a learning curve analysis. Urology 93:104–111. https://doi.org/10.1016/j.urology.2016.03.036
Kim IK, Kang J, Park YA et al (2014) Is prior laparoscopy experience required for adaptation to robotic rectal surgery?: Feasibility of one-step transition from open to robotic surgery. Int J Colorectal Dis 29:693–699. https://doi.org/10.1007/s00384-014-1858-2
Nio D, Bemelman WA, Balm R et al (2005) Laparoscopic vascular anastomoses: does robotic (Zeus-Aesop) assistance help to overcome the learning curve? Surg Endosc 19:1071–1076. https://doi.org/10.1007/s00464-004-2178-3
Sumi Y, Dhumane PW, Komeda K et al (2013) Learning curves in expert and non-expert laparoscopic surgeons for robotic suturing with the da Vinci((R)) surgical system. J Robot Surg 7:29–34. https://doi.org/10.1007/s11701-012-0336-5
Kowalewski KF, Schmidt MW, Proctor T et al (2018) Skills in minimally invasive and open surgery show limited transferability to robotic surgery: results from a prospective study. Surg Endosc 32:1656–1667. https://doi.org/10.1007/s00464-018-6109-0
Cetin T, Yalcin MY, Karaca E et al (2022) Laparoscopic surgery experience does not influence oncological and functional results of robotic-assisted laparoscopic prostatectomy. Urol J 89:240–243. https://doi.org/10.1177/03915603211004781
Sundelin MO, Paltved C, Kingo PS et al (2022) The transferability of laparoscopic and open surgical skills to robotic surgery. Adv Simul (Lond) 7:26. https://doi.org/10.1186/s41077-022-00223-2
Willuth E, Hardon SF, Lang F et al (2022) Robotic-assisted cholecystectomy is superior to laparoscopic cholecystectomy in the initial training for surgical novices in an ex vivo porcine model: a randomized crossover study. Surg Endosc 36:1064–1079. https://doi.org/10.1007/s00464-021-08373-6
Zapardiel I, Hernandez A, De Santiago J (2015) The efficacy of robotic driven handheld instruments for the acquisition of basic laparoscopic suturing skills. Eur J Obstet Gynecol Reprod Biol 186:106–109. https://doi.org/10.1016/j.ejogrb.2015.01.013
Anderberg M, Larsson J, Kockum CC et al (2010) Robotics versus laparoscopy—an experimental study of the transfer effect in maiden users. Ann Surg Innov Res 4:3. https://doi.org/10.1186/1750-1164-4-3
Angell J, Gomez MS, Baig MM et al (2013) Contribution of laparoscopic training to robotic proficiency. J Endourol 27:1027–1031. https://doi.org/10.1089/end.2013.0082
Belotto M, Coutinho L, Pacheco-Jr AM et al (2022) Influence of minimally invasive laparoscopic experience skills on robotic surgery dexterity. Arq Bras Cir Dig 34:e1604. https://doi.org/10.1590/0102-672020210003e1604
Blavier A, Nyssen A (2014) The effect of 2D and 3D visual modes on surgical task performance: role of expertise and adaptation processes. Cogn Technol Work 16:509–518. https://doi.org/10.1007/s10111-014-0281-3
Borahay MA, Haver MC, Eastham B et al (2013) Modular comparison of laparoscopic and robotic simulation platforms in residency training: a randomized trial. J Minim Invasive Gynecol 20:871–879. https://doi.org/10.1016/j.jmig.2013.06.005
Davila DG, Helm MC, Frelich MJ et al (2018) Robotic skills can be aided by laparoscopic training. Surg Endosc 32:2683–2688. https://doi.org/10.1007/s00464-017-5963-5
Finnerty BM, Afaneh C, Aronova A et al (2016) General surgery training and robotics: are residents improving their skills? Surg Endosc 30:567–573. https://doi.org/10.1007/s00464-015-4240-8
Hagen ME, Wagner OJ, Inan I et al (2009) Impact of IQ, computer-gaming skills, general dexterity, and laparoscopic experience on performance with the da Vinci surgical system. Int J Med Robot 5:327–331. https://doi.org/10.1002/rcs.264
Kanitra JJ, Khogali-Jakary N, Gambhir SB et al (2021) Transference of skills in robotic vs. laparoscopic simulation: a randomized controlled trial. BMC Surg 21:379. https://doi.org/10.1186/s12893-021-01385-y
Kilic GS, Walsh TM, Borahay M et al (2012) Effect of residents’ previous laparoscopic surgery experience on initial robotic suturing experience. ISRN Obstet Gynecol 2012:569456. https://doi.org/10.5402/2012/569456
Kim HJ, Choi GS, Park JS et al (2014) Comparison of surgical skills in laparoscopic and robotic tasks between experienced surgeons and novices in laparoscopic surgery: an experimental study. Ann Coloproctol 30:71–76. https://doi.org/10.3393/ac.2014.30.2.71
Moncayo S, Compagnon R, Caire F et al (2020) Transition effects from laparocscopic to robotic surgery skills in small cavities. J Robot Surg 14:525–530. https://doi.org/10.1007/s11701-019-01024-y
Prasad SM, Maniar HS, Soper NJ et al (2002) The effect of robotic assistance on learning curves for basic laparoscopic skills. Am J Surg 183:702–707. https://doi.org/10.1016/s0002-9610(02)00871-1
Sarle R, Tewari A, Shrivastava A et al (2004) Surgical robotics and laparoscopic training drills. J Endourol 18:63–66. https://doi.org/10.1089/089277904322836703 (discussion 66–67)
Thomaier LOM, Abernethy M, Paka C, Chen CCG (2017) Laparoscopic and robotic skills are transferable in a simulation setting: a randomized controlled trial. Surg Endosc 31:3279–3285. https://doi.org/10.1007/s00464-016-5359-y
Ashley CW, Donaldson K, Evans KM et al (2019) Surgical cross-training with surgery naive learners: implications for resident training. J Surg Educ 76:1469–1475. https://doi.org/10.1016/j.jsurg.2019.06.015
Blavier A, Gaudissart Q, Cadiere GB et al (2007) Comparison of learning curves and skill transfer between classical and robotic laparoscopy according to the viewing conditions: implications for training. Am J Surg 194:115–121. https://doi.org/10.1016/j.amjsurg.2006.10.014
Ghazanfar S, Qureshi S, Zubair M et al (2021) Is laparoscopic experience helpful in simulator based robotic training in general surgery? J Pak Med Assoc 71:2198–2202. https://doi.org/10.47391/JPMA.05-779
Hassan SO, Dudhia J, Syed LH et al (2015) Conventional laparoscopic vs robotic training: which is better for naive users? A randomized prospective crossover study. J Surg Educ 72:592–599. https://doi.org/10.1016/j.jsurg.2014.12.008
Panait L, Shetty S, Shewokis PA et al (2014) Do laparoscopic skills transfer to robotic surgery? J Surg Res 187:53–58. https://doi.org/10.1016/j.jss.2013.10.014
Pimentel M, Cabral RD, Costa MM et al (2018) Does previous laparoscopic experience influence basic robotic surgical skills? J Surg Educ 75:1075–1081. https://doi.org/10.1016/j.jsurg.2017.11.005
Shakir F, Jan H, Kent A (2016) 3D straight-stick laparoscopy versus 3D robotics for task performance in novice surgeons: a randomised crossover trial. Surg Endosc 30:5380–5387. https://doi.org/10.1007/s00464-016-4893-y
Teishima J, Hattori M, Inoue S et al (2012) Impact of laparoscopic experience on the proficiency gain of urologic surgeons in robot-assisted surgery. J Endourol 26:1635–1638. https://doi.org/10.1089/end.2012.0308
Yoo BE, Kim J, Cho JS et al (2015) Impact of laparoscopic experience on virtual robotic simulator dexterity. J Minim Access Surg 11:68–71. https://doi.org/10.4103/0972-9941.147696
Zihni A, Gerull WD, Cavallo JA et al (2018) Comparison of precision and speed in laparoscopic and robot-assisted surgical task performance. J Surg Res 223:29–33. https://doi.org/10.1016/j.jss.2017.07.037
Obek C, Hubka M, Porter M et al (2005) Robotic versus conventional laparoscopic skill acquisition: implications for training. J Endourol 19:1098–1103. https://doi.org/10.1089/end.2005.19.1098
Kirkman MA (2013) Deliberate practice, domain-specific expertise, and implications for surgical education in current climes. J Surg Educ 70:309–317. https://doi.org/10.1016/j.jsurg.2012.11.011
Bransford JD, Schwartz DL (1999) Rethinking transfer: a simple proposal with multiple implications. American Educational Research Association, Washington
Leberman S, McDonald L (2006) The transfer of learning participants’ perspectives of adult education and training. Routledge, New York
Fundamentals of Laparoscopic Surgery—the definite laparoscopic skills enhancement and assessment module. https://www.flsprogram.org/
Lerner V, DeStephano C, Ulrich A et al (2021) A systematic review of validity evidence for the fundamentals of laparoscopic surgery examination in gynecology. J Minim Invasive Gynecol 28:1313–1324. https://doi.org/10.1016/j.jmig.2021.04.010
Zendejas B, Ruparel RK, Cook DA (2016) Validity evidence for the Fundamentals of Laparoscopic Surgery (FLS) program as an assessment tool: a systematic review. Surg Endosc 30:512–520. https://doi.org/10.1007/s00464-015-4233-7
Kirwan C, Birchall D (2006) Transfer of learning from management development programmes: testing the Holton model. Int J Train Dev 10:252–268. https://doi.org/10.1111/j.1468-2419.2006.00259.x
Chahal B, Aydin A, Amin MSA et al (2022) Transfer of open and laparoscopic skills to robotic surgery: a systematic review. J Robot Surg. https://doi.org/10.1007/s11701-022-01492-9
Bjerrum F, Sorensen JL, Konge L et al (2016) Randomized trial to examine procedure-to-procedure transfer in laparoscopic simulator training. Br J Surg 103:44–50. https://doi.org/10.1002/bjs.9966
Miller GE (1990) The assessment of clinical skills/competence/performance. Acad Med 65:S63-67. https://doi.org/10.1097/00001888-199009000-00045
Kolozsvari NO, Kaneva P, Brace C et al (2011) Mastery versus the standard proficiency target for basic laparoscopic skill training: effect on skill transfer and retention. Surg Endosc 25:2063–2070. https://doi.org/10.1007/s00464-011-1743-9
Thomsen ASS, Kiilgaard JF, la Cour M et al (2017) Is there inter-procedural transfer of skills in intraocular surgery? A randomized controlled trial. Acta Ophthalmol 95:845–851. https://doi.org/10.1111/aos.13434
Jacobsen ME, Gustafsson A, Jorgensen PG et al (2021) Practicing procedural skills is more effective than basic psychomotor training in knee arthroscopy: a randomized study. Orthop J Sports Med 9:2325967120985129. https://doi.org/10.1177/2325967120985129
Yudkowsky R, Park YS, Downing SM (2019) Assessment in health professions education, 2nd edn. Routledge, Milton Park
Hajian S (2019) Transfer of learning and teaching: a review of transfer theories and effective instructional practices. J Educ IAFOR 7:93–111. https://doi.org/10.22492/ije.7.1.06
Leijte E, de Blaauw I, Van Workum F et al (2020) Robot assisted versus laparoscopic suturing learning curve in a simulated setting. Surg Endosc 34:3679–3689. https://doi.org/10.1007/s00464-019-07263-2
Hanzly M, Frederick A, Creighton T et al (2015) Learning curves for robot-assisted and laparoscopic partial nephrectomy. J Endourol 29:297–303. https://doi.org/10.1089/end.2014.0303
Pietersen PI, Bjerrum F, Tolsgaard MG et al (2022) Standard setting in simulation-based training of surgical procedures: a systematic review. Ann Surg 275:872–882. https://doi.org/10.1097/SLA.0000000000005209
Borgersen NJ, Naur TMH, Sorensen SMD et al (2018) Gathering validity evidence for surgical simulation: a systematic review. Ann Surg 267:1063–1068. https://doi.org/10.1097/SLA.0000000000002652
Cook DA, Hatala R (2015) Got power? A systematic review of sample size adequacy in health professions education research. Adv Health Sci Educ Theory Pract 20:73–83. https://doi.org/10.1007/s10459-014-9509-5
Schünemann HBJ, Brożek J, Guyatt G, Oxman A (2013) GRADE handbook for grading quality of evidence and strength of recommendations. The GRADE Working Group. http://www.guidelinedevelopment.org/handbook. Accessed 20 Mar 2014
Dawe SR, Pena GN, Windsor JA et al (2014) Systematic review of skills transfer after surgical simulation-based training. Br J Surg 101:1063–1076. https://doi.org/10.1002/bjs.9482
Safiejko K, Tarkowski R, Koselak M et al (2021) Robotic-assisted vs. standard laparoscopic surgery for rectal cancer resection: a systematic review and meta-analysis of 19,731 patients. Cancers (Basel). https://doi.org/10.3390/cancers14010180
Cuk P, Kjaer MD, Mogensen CB et al (2022) Short-term outcomes in robot-assisted compared to laparoscopic colon cancer resections: a systematic review and meta-analysis. Surg Endosc 36:32–46. https://doi.org/10.1007/s00464-021-08782-7
Acknowledgements
N/A.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Pia Iben Pietersen, Peter Hertz, Rikke Groth Olsen, Louise Birch Møller, Lars Konge, and Flemming Bjerrum have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pietersen, P.I., Hertz, P., Olsen, R.G. et al. Transfer of skills between laparoscopic and robot-assisted surgery: a systematic review. Surg Endosc 37, 9030–9042 (2023). https://doi.org/10.1007/s00464-023-10472-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10472-5