Abstract
Background
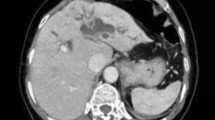
This study aimed to investigate the safety and efficacy of laparoscopic anatomical left hemihepatectomy guided by the middle hepatic vein (MHV) for the treatment of patients with hepatolithiasis who had a history of upper abdominal surgery.
Methods
Retrospective data analysis was performed on patients who underwent laparoscopic left hepatectomy for hepatolithiasis and with previous upper abdominal surgery at the Second Affiliated Hospital of Nanchang University from January 2018 to April 2022. According to the different surgical approaches, patients were divided into laparoscopic anatomical left hepatectomy guided by the MHV group (MHV-AH group) and laparoscopic traditional anatomical left hepatectomy not guided by the MHV group (non-MHV-AH group).
Results
This study included 81 patients, with 37 and 44 patients in the MHV-AH and non-MHV-AH groups, respectively. There was no significant difference in the basic information between the two groups. Five cases were converted to laparotomy, and the remaining were successfully completed under laparoscopy. Compared to the non-MHV-AH group, the MHV-AH group had a slightly longer operation time (319.30 min vs 273.93 min, P = 0.032), lower bile leakage rate (5.4% vs 20.5%, P = 0.047), stone residual rate (2.7% vs 20.5%, P = 0.015), stone recurrence rate (5.4% vs 22.7%, P = 0.028), and cholangitis recurrence rate (2.7% vs 22.7%, P = 0.008).There were no significant differences in the results of other observation indices between the groups.
Conclusions
Laparoscopic anatomical left hepatectomy guided by the MHV is safe and effective in the treatment of left hepatolithiasis with a history of upper abdominal surgery. It does not increase intraoperative bleeding and reduces the risk of postoperative bile leakage, residual stones, stone recurrence, and cholangitis recurrence.



Similar content being viewed by others
References
Tazuma S, Unno M, Igarashi Y, Inui K, Uchiyama K, Kai M, Tsuyuguchi T, Maguchi H, Mori T, Yamaguchi K, Ryozawa S, Nimura Y, Fujita N, Kubota K, Shoda J, Tabata M, Mine T, Sugano K, Watanabe M, Shimosegawa T (2017) Evidence-based clinical practice guidelines for cholelithiasis 2016. J Gastroenterol 52:276–300
Jarufe N, Figueroa E, Muñoz C, Moisan F, Varas J, Valbuena JR, Bambs C, Martínez J, Pimentel F (2012) Anatomic hepatectomy as a definitive treatment for hepatolithiasis: a cohort study. HPB (Oxford) 14:604–610
Liao C, Wang D, Huang L, Bai Y, Yan M, Zhou S, Qiu F, Lai Z, Wang Y, Tian Y, Zheng X, Chen S (2021) A new strategy of laparoscopic anatomical hemihepatectomy guided by the middle hepatic vein combined with transhepatic duct lithotomy for complex hemihepatolithiasis: a propensity score matching study. Surgery 170:18–29
Liao KX, Chen L, Ma L, Cao L, Shu J, Sun TG, Li XS, Wang XJ, Li JW, Chen J, Cao Y, Zheng SG (2022) Laparoscopic middle-hepatic-vein-guided anatomical hemihepatectomy in the treatment of hepatolithiasis: a 10-year case study. Surg Endosc 36:881–888
Huang ZQ, Huang XQ, Zhang WZ, Xu LN, Yang T, Zhang AQ, Dong JH (2008) Liver resection in hepatolithiasis: 20-year’s evolution. Zhonghua Wai Ke Za Zhi 46:1450–1452
Makuuchi M (2013) Surgical treatment for HCC–special reference to anatomical resection. Int J Surg 11(Suppl 1):S47-49
Lorio E, Patel P, Rosenkranz L, Patel S, Sayana H (2020) Management of hepatolithiasis: review of the literature. Curr Gastroenterol Rep 22:30
Geraci G, D’Orazio B, Rizzuto S, Cajozzo M, Modica G (2017) Videolaparoscopic cholecystectomy in patients with previous abdominal surgery. Personal experience and literature review. Clin Ter 168:e357–e360
Zhu J, Sun G, Hong L, Li X, Li Y, Xiao W (2018) Laparoscopic common bile duct exploration in patients with previous upper abdominal surgery. Surg Endosc 32:4893–4899
Isetani M, Morise Z, Kawabe N, Tomishige H, Nagata H, Kawase J, Arakawa S (2015) Pure laparoscopic hepatectomy as repeat surgery and repeat hepatectomy. World J Gastroenterol 21:961–968
Wu JM, Lin HF, Chen KH, Tseng LM, Tsai MS, Huang SH (2007) Impact of previous abdominal surgery on laparoscopic appendectomy for acute appendicitis. Surg Endosc 21:570–573
Kovachev S, Ganovska A, Atanasova V, Sergeev S, Mutafchiyski V, Vladov N (2015) Open laparoscopy–A modified Hasson technique. Akush Ginekol (Sofiia) 54:52–56
Ahn KS, Han HS, Yoon YS, Cho JY, Kim JH (2011) Laparoscopic liver resection in patients with a history of upper abdominal surgery. World J Surg 35:1333–1339
Zheng S (2018) Anatomical basis and clinical value of liver parenchyma transection guided by the hepatic vein. Chin J Practical Surg 38:360–362
Huang Y, Liao A, Pu X, Yang J, Lv T, Yan L, Yang J, Wu H, Jiang L (2022) A randomized controlled trial of effect of 15- or 25-minute intermittent Pringle maneuver on hepatectomy for hepatocellular carcinoma. Surgery 171:1596–1604
Lin CX, Guo Y, Lau WY, Zhang GY, Huang YT, He WZ, Lai EC (2013) Optimal central venous pressure during partial hepatectomy for hepatocellular carcinoma. Hepatobiliary Pancreat Dis Int 12:520–524
Smyrniotis V, Kostopanagiotou G, Theodoraki K, Tsantoulas D, Contis JC (2004) The role of central venous pressure and type of vascular control in blood loss during major liver resections. Am J Surg 187:398–402
Cecconello I, Pollara WM, Zilberstein B, Saldanha LB, Pinotti HW (1984) Histopathology of the common bile duct in choledocholithiasis. Arq Gastroenterol 20:137–143
El-Geidie AA (2010) Is the use of T-tube necessary after laparoscopic choledochotomy? J Gastrointest Surg 14:844–848
Ivanov D, Milosević P (2010) Primary closure of the common bile duct in the treatment of choledocholithiasis. Med Pregl 63:99–103
Cheon YK, Cho YD, Moon JH, Lee JS, Shim CS (2009) Evaluation of long-term results and recurrent factors after operative and nonoperative treatment for hepatolithiasis. Surgery 146:843–853
Acknowledgements
We would like to thank the contributions of all of the patients in our study. This research was funded by grants from the National Natural Science Foundation of China (No.82160578); the Natural Science Foundation of Jiangxi Province, China (No. 20232BAB216076 and 20202BAB216029); the Health Department of Jiangxi Province, China (No.20201066 and 202210033); and the Research Project of Education Department of Jiangxi Province, China (No.GJJ2200227).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosures
Yuting Fan, Jian Huang, Liangzhi Xu, Qi Xu, Xinguo Tang, Kangpeng Zheng, wei Hu, Jinghang Liu, Jiyang Wang, Tiande Liu, Bo Liang, Hu Xiong, Wen Li, Xiaowei Fu, and Lu Fang have no conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fan, Y., Huang, J., Xu, L. et al. Laparoscopic anatomical left hemihepatectomy guided by middle hepatic vein in the treatment of left hepatolithiasis with a history of upper abdominal surgery. Surg Endosc 37, 9116–9124 (2023). https://doi.org/10.1007/s00464-023-10458-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10458-3