Abstract
Background
Evidence for how to best train surgical residents for robotic bariatric procedures is lacking. We developed targeted educational resources to promote progression on the robotic bariatric learning curve. This study aimed to characterize the effect of resources on resident participation in robotic bariatric procedures.
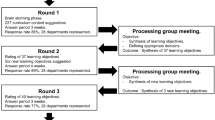
Methods
Performance metrics from the da Vinci Surgical System were retrospectively reviewed for sleeve gastrectomy (SG) and Roux-en-Y gastric bypass (RYGB) cases involving general surgery trainees with a single robotic bariatric surgeon. Pictorial case guides and narrated operative videos were developed for these procedures and disseminated to trainees. Percent active control time (%ACT)—amount of trainee console time spent in active instrument manipulations over total active time from both consoles—was the primary outcome measure following dissemination. One-way ANOVA, Student’s t-tests, and Pearson correlations were applied.
Results
From September 2020 to July 2021, 50 cases (54% SG, 46% RYGB) involving 14 unique trainees (PGY1-PGY5) were included. From November 2021 to May 2022 following dissemination, 29 cases (34% SG, 66% RYGB) involving 8 unique trainees were included. Mean %ACT significantly increased across most trainee groups following resource distribution: 21% versus 38% for PGY3s (p = 0.087), 32% versus 45% for PGY4s (p = 0.0009), and 38% versus 57% for PGY5s (p = 0.0015) and remained significant when stratified by case type. Progressive trainee %ACT was not associated with total active time for SG cases before or after intervention (pre r = − 0.0019, p = 0.9; post r = − 0.039, p = 0.9). It was moderately positively associated with total active time for RYGB cases before dissemination (r = 0.46, p = 0.027) but lost this association following intervention (r = 0.16, p = 0.5).
Conclusion
Use of targeted educational resources promoted increases in trainee participation in robotic bariatric procedures with more time spent actively operating at the console. As educators continue to develop robotic training curricula, efforts should include high-quality resource development for other sub-specialty procedures. Future work will examine the impact of increased trainee participation on clinical and patient outcomes.
Graphical abstract





Similar content being viewed by others
References
Armijo PR, Pagkratis S, Boilesen E, Tanner T, Oleynikov D (2018) Growth in robotic-assisted procedures is from conversion of laparoscopic procedures and not from open surgeons’ conversion: a study of trends and costs. Surg Endosc 32(4):2106–2113
Scarritt T, Hsu CH, Maegawa FB, Ayala AE, Mobily M, Ghaderi I (2021) Trends in utilization and perioperative outcomes in robotic-assisted bariatric surgery using the MBSAQIP database: a 4-year analysis. Obes Surg 31(2):854–861
Tatarian T, Yang J, Wang J et al (2021) Trends in the utilization and perioperative outcomes of primary robotic bariatric surgery from 2015 to 2018: a study of 46,764 patients from the MBSAQIP data registry. Surg Endosc 35(7):3915–3922
Fourman MM, Saber AA (2012) Robotic bariatric surgery: a systematic review. Surg Obes Relat Dis 8(4):483–488
Li K, Zou J, Tang J, Di J, Han X, Zhang P (2016) Robotic versus laparoscopic bariatric surgery: a systematic review and meta-analysis. Obes Surg 26(12):3031–3044
Zhang Z, Miao L, Ren Z, Li Y (2021) Robotic bariatric surgery for the obesity: a systematic review and meta-analysis. Surg Endosc 35(6):2440–2456
Toro JP, Lin E, Patel AD (2015) Review of robotics in foregut and bariatric surgery. Surg Endosc 29(1):1–8
Jung MK, Hagen ME, Buchs NC, Buehler LH, Morel P (2017) Robotic bariatric surgery: a general review of the current status. Int J Med Robot. https://doi.org/10.1002/rcs.1834
Sanchez BR, Mohr CJ, Morton JM, Safadi BY, Alami RS, Curet MJ (2005) Comparison of totally robotic laparoscopic Roux-en-Y gastric bypass and traditional laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis 1(6):549–554
Starnes CC, Gochnour DC, Hall B, Wilson EB, Snyder BE (2015) The economy of motion of the totally robotic gastric bypass: technique, learning curve, and outcomes of a fellowship-trained, robotic bariatric surgeon. J Laparoendosc Adv Surg Tech A 25(5):411–418
Goldberg I, Yang J, Park J et al (2018) Surgical trainee impact on bariatric surgery safety. Surg Endosc 33(9):3014–3025
Winder JS, Juza RM, Sasaki J, Rogers AM, Pauli EM, Haluck RS, Estes SJ, Lyn-Sue JR (2016) Implementing a robotics curriculum at an academic general surgery training program: our initial experience. J Robot Surg 10(3):209–2013
Mustafa S, Handren E, Farmer D, Ontiveros E, Ogola GO, Leeds SG (2019) Robotic curriculum enhances minimally invasive general surgery residents’ education. J Surg Educ 76(2):548–553
Gerull W, Zihni A, Awad M (2020) Operative performance outcomes of a simulator-based robotic skills curriculum. Surg Endosc 34(10):4543–4548
Chen R, Rodrigues Armijo P, Krause C, Siu KC, Oleynikov D, SAGES Robotic Task Force (2020) A comprehensive review of robotic surgery curriculum and training for residents, fellows, and postgraduate surgical education. Surg Endosc 34(1):361–367
Mota P, Carvalho N, Carvalho-Dias E, João Costa M, Correia-Pinto J, Lima E (2018) Video-based surgical learning: improving trainee education and preparation for surgery. J Surg Educ 75(3):828–835
Rapp AK, Healy MG, Charlton ME, Keith JN, Rosenbaum ME, Kapadia MR (2016) YouTube is the most frequently used educational video source for surgical preparation. J Surg Educ 73(6):1072–1076
Clanahan JM, Yee A, Awad MM (2023) Active control time: an objective performance metric for trainee participation in robotic surgery. J Robot Surg. https://doi.org/10.1007/s11701-023-01628-5
Iranmanesh P, Morel P, Wagner OJ, Inan I, Pugin F, Hagen ME (2010) Set-up and docking of the da Vinci surgical system: prospective analysis of initial experience. Int J Med Robot 6(1):57–60
van der Schans EM, Hiep MAJ, Consten ECJ, Broeders IAMJ (2020) From Da Vinci Si to Da Vinci Xi: realistic times in draping and docking the robot. J Robot Surg 14(6):835–839
Rahimi AO, Ho K, Chang M, Gasper D, Ashouri Y, Dearmon-Moore D, Hsu CH, Ghaderi I (2022) A systematic review of robotic surgery curricula using a contemporary educational framework. Surg Endosc. https://doi.org/10.1007/s00464-022-09788-5
Kern DE, Thomas PA, Bass EB, Howard DM (1998) Curriculum development for medical education: a six step approach. JHU Press, Baltimore
Sánchez R, Rodríguez O, Rosciano J et al (2016) Robotic surgery training: construct validity of Global Evaluative Assessment of Robotic Skills (GEARS). J Robot Surg 10(3):227–231
Addison P, Yoo A, Duarte-Ramos J et al (2021) Correlation between operative time and crowd-sourced skills assessment for robotic bariatric surgery. Surg Endosc 35(9):5303–5309
Krell RW, Birkmeyer NJ, Reames BN et al (2014) Effects of resident involvement on complication rates after laparoscopic gastric bypass. J Am Coll Surg 218(2):253–260
Doyon L, Moreno-Koehler A, Ricciardi R, Nepomnayshy D (2016) Resident participation in laparoscopic Roux-en-Y gastric bypass: a comparison of outcomes from the ACS-NSQIP database. Surg Endosc 30(8):3216–3224
Martinovski M, Navratil AL, Zeni T, Jonker M, Ferraro J, Albright J, Cleary RK (2017) Effects of resident or fellow participation in sleeve gastrectomy and gastric bypass: results from the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP). J Am Coll Surg 225(4):S14
de’Angelis N, Gavriilidis P, Martínez-Pérez A et al (2019) Educational value of surgical videos on YouTube: quality assessment of laparoscopic appendectomy videos by senior surgeons vs. novice trainees. World J Emerg Surg 14(22):1–11
Deal SB, Alseidi AA (2017) Concerns of quality and safety in public domain surgical education videos: an assessment of the critical view of safety in frequently used laparoscopic cholecystectomy videos. J Am Coll Surg 225(6):725–730
Rodriguez HA, Young MT, Jackson HT, Oelschlager BK, Wright AS (2018) Viewer discretion advised: is YouTube a friend or foe in surgical education? Surg Endosc 32(4):1724–1728
Jackson HT, Hung CS, Potarazu D et al (2022) Attending guidance advised: educational quality of surgical videos on YouTube. Surg Endosc 36(6):4189–4198
Celentano V, Smart N, McGrath J et al (2018) LAP-VEGaS practice guidelines for reporting of educational videos in laparoscopic surgery: a joint trainers and trainees consensus statement. Ann Surg 268(6):920–926
Celentano V, Smart N, Cahill RA et al (2021) Development and validation of a recommended checklist for assessment of surgical videos quality: the LAParoscopic surgery Video Educational GuidelineS (LAP-VEGaS) video assessment tool. Surg Endosc 35(3):1362–1369
Acknowledgements
The authors thank Sylvia Padilla for her assistance with organization of performance metric data obtained from the da Vinci Surgical System.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Awad has educational grants from Applied Medical, Bard/BD Medical, Baxter, Ethicon, Medtronic, Stryker, and Intuitive Surgical for resident simulation training. Dr. Dimou is a consultant for Intuitive Surgical. Dr. Clanahan has no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplement 3: Robotic sleeve gastrectomy operative video narration(MP4 2467087 kb)
Supplement 4: Robotic Roux-en-Y gastric bypass operative video narration (MP4 4662000 kb)
464_2023_10436_MOESM5_ESM.docx
Supplement 5: Active control time by case type and trainee level at baseline (A) and following resource dissemination (B) (DOCX 15 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Clanahan, J.M., Awad, M.M. & Dimou, F.M. Use of targeted educational resources to improve robotic bariatric surgery training. Surg Endosc 38, 894–901 (2024). https://doi.org/10.1007/s00464-023-10436-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10436-9