Abstract
Background
Pain management after bariatric surgery remains challenging given the risk for analgesia-related adverse events (e.g., opioid use disorder, marginal ulcers). Identifying modifiable factors associated with patient-reported pain outcomes may improve quality of care. We evaluated the extent to which patient and procedural factors predict 7-day post-discharge pain intensity, pain interference, and satisfaction with pain management after bariatric surgery.
Methods
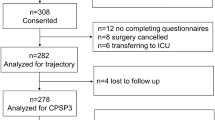
This prospective cohort study included adults undergoing laparoscopic bariatric surgery at two university-affiliated hospitals and one private clinic. Preoperative assessments included demographics, Pain Catastrophizing Scale (score range 0–52), Patient Activation Measure (low [< 55.1] vs. high [≥ 55.1]), pain expectation (0–10), and Patient-Reported Outcomes Measurement Information System-29 (PROMIS-29) anxiety and depression scales. At 7 days post-discharge, assessments included PROMIS-29 pain intensity (0–10) and pain interference scales (41.6–75.6), and satisfaction with pain management (high [10–9] vs. lower [8–0]). Linear and logistic regression were used to assess the association of pain outcomes with potential predictors.
Results
Three hundred and fifty-one patients were included (mean age = 44 ± 11 years, BMI = 45 ± 8 kg/m2, 77% female, 71% sleeve gastrectomy). At 7 days post-discharge, median (IQR) patient-reported pain intensity was 2.5 (1–5), pain interference was 55.6 (52.0–61.2), and 76% of patients reported high satisfaction with pain management. Pain intensity was predicted by preoperative anxiety (β + 0.04 [95% CI + 0.01 to + 0.07]) and pain expectation (+ 0.15 [+ 0.05 to + 0.25]). Pain interference was predicted by preoperative anxiety (+ 0.22 [+ 0.11 to + 0.33]), pain expectation (+ 0.47 [+ 0.10 to + 0.84]), and age (− 0.09 [− 0.174 to − 0.003]). Lower satisfaction was predicted by low patient activation (OR 1.94 [1.05–3.58]), higher pain catastrophizing (1.03 [1.003–1.05]), 30-day complications (3.27 [1.14–9.38]), and age (0.97 [0.948–0.998]).
Conclusion
Patient-related factors are important predictors of post-discharge pain outcomes after bariatric surgery. Our findings highlight the value of addressing educational, psychological, and coping strategies to improve postoperative pain outcomes.
Graphical abstract


Similar content being viewed by others
References
Brown WA, Kow L, Shikora S, Liem R, Welbourn R, Dixon J, Walton P, Kinsman R (2021) Sixth IFSO global registry report. https://www.ifso.com/pdf/ifso-6th-registry-report-2021.pdf. Accessed 18 Feb 2023.
Andalib A, Bouchard P, Bougie A, Loiselle SE, Demyttenaere S, Court O (2018) Variability in bariatric surgical care among various centers: a survey of all bariatric surgeons in the province of Quebec, Canada. Obes Surg 28(8):2327–2332. https://doi.org/10.1007/s11695-018-3157-4
Telem DA, Majid SF, Powers K, DeMaria E, Morton J, Jones DB (2017) Assessing national provision of care: variability in bariatric clinical care pathways. Surg Obes Relat Dis 13(2):281–284. https://doi.org/10.1016/j.soard.2016.08.002
Ibrahim AM, Ghaferi AA, Thumma JR, Dimick JB (2017) Variation in outcomes at bariatric surgery centers of excellence. JAMA Surg 152(7):629–636. https://doi.org/10.1001/jamasurg.2017.0542
Makki H, Mahdy T, Emile SH, Nofal H, Asaad Y, Abdulateef O, Rasheed M, Madyan A (2021) Analysis of emergency department visits and unplanned readmission after bariatric surgery: an experience from a tertiary referral center. Surg Laparosc Endosc Percutan Tech 32(1):107–113. https://doi.org/10.1097/SLE.0000000000001011
Gan TJ (2017) Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res 10:2287–2298. https://doi.org/10.2147/JPR.S144066
Thapa P, Euasobhon P (2018) Chronic postsurgical pain: current evidence for prevention and management (2018). Korean J Pain 31(3):155–173. https://doi.org/10.3344/kjp.2018.31.3.155,July2
Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W (2013) Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology 118(4):934–944. https://doi.org/10.1097/ALN.0b013e31828866b3
Iamaroon A, Tangwiwat S, Nivatpumin P, Lertwacha T, Rungmongkolsab P, Pangthipampai P (2019) Risk factors for moderate to severe pain during the first 24 hours after laparoscopic bariatric surgery while receiving intravenous patient-controlled analgesia. Anesthesiol Res Pract 2019:6593736. https://doi.org/10.1155/2019/6593736
Schug SA, Raymann A (2011) Postoperative pain management of the obese patient. Best Pract Res Clin Anaesthesiol 25(1):73–81. https://doi.org/10.1016/j.bpa.2010.12.001
Heinberg LJ, Pudalov L, Alameddin H, Steffen K (2019) Opioids and bariatric surgery: a review and suggested recommendations for assessment and risk reduction. Surg Obes Relat Dis 15(2):314–321. https://doi.org/10.1016/j.soard.2018.11.019
Nasser K, Verhoeff K, Mocanu V, Kung JY, Purich K, Switzer NJ, Birch DW, Karmali S (2023) New persistent opioid use after bariatric surgery: a systematic review and pooled proportion meta-analysis. Surg Endosc 37(1):703–714. https://doi.org/10.1007/s00464-022-09291-x
Butt M, Eisler RA, Hu A, Rogers AM, Rigby A (2023) Incidence of substance use disorder following bariatric surgery: a retrospective cohort study. Obes Surg 33(3):890–896. https://doi.org/10.1007/s11695-022-06400-6
Doufas A (2014) Obstructive Sleep apnea, pain, and opioid analgesia in the postoperative patient. Curr Anesth Rep 4(1–9):2013. https://doi.org/10.1007/s40140-013-0047-0,December18
Garimella V, Cellini C (2013) Postoperative pain control. Clin Colon Rectal Surg 26(3):191–196. https://doi.org/10.1055/s-0033-1351138
Mechanick JI, Apovian C, Brethauer S, Garvey WT, Joffe AM, Kim J, Kushner RF, Lindquist R, Pessah-Pollack R, Seger J, Urman RD, Adams S, Cleek JB, Correa R, Figaro MK, Flanders K, Grams J, Hurley DL, Kothari S, Seger MV, Still CD (2019) Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures, 2019 update: cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, the Obesity Society, American Society for Metabolic & Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists. Endocr Pract 25(12):1346–1359. https://doi.org/10.4158/GL-2019-0406
Jain S, Lapointe-Gagner M, Alali N, Elhaj H, Poirier AS, Kaneva P, Alhashemi M, Lee L, Agnihotram RV, Feldman LS, Gagner M, Andalib A, Fiore JF Jr (2023) Prescription and consumption of opioids after bariatric surgery: a multicenter prospective cohort study. Surg Endosc (Epub ahead of print). https://doi.org/10.1007/s00464-023-10265-w.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP (2008) STROBE Initiative: the strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 61(4):344–349. https://doi.org/10.1016/j.jclinepi.2007.11.008
McGill University Health Center Patient Education Office (2017) A guide to bariatric surgery, Sept 8, 2017. https://www.muhcpatienteducation.ca/DATA/GUIDE/714_en~v~bariatric-surgery-muhc.pdf. Accessed 18 Mar 2023
Thorell A, MacCormick AD, Awad S, Reynolds N, Roulin D, Demartines N, Vignaud M, Alvarez A, Singh PM, Lobo DN (2016) Guidelines for perioperative care in bariatric surgery: enhanced recovery after surgery (ERAS) society recommendations. World J Surg 40(9):2065–2083. https://doi.org/10.1007/s00268-016-3492-3
Stenberg E, Dos Reis Falcão LF, O’Kane M, Liem R, Pournaras DJ, Salminen P, Urman RD, Wadhwa A, Gustafsson UO, Thorell A (2021) Guidelines for perioperative care in bariatric surgery: enhanced recovery after surgery (ERAS) society recommendations: a 2021 update. World J Surg 46(4):729–751. https://doi.org/10.1007/s00268-021-06394-9
Al-Masrouri S, Alnumay A, Vourtzoumis P, Court O, Demyttenaere S, Feldman LS, Andalib A (2022) Ambulatory sleeve gastrectomy: a prospective feasibility and comparative study of early postoperative morbidity. Surg Endosc. https://doi.org/10.1007/s00464-022-09721-w
van Boekel RLM, Vissers KCP, van der Sande R, Bronkhorst E, Lerou JGC, Steegers MAH (2017) Moving beyond pain scores: multidimensional pain assessment is essential for adequate pain management after surgery. PLoS ONE 12(5):e0177345. https://doi.org/10.1371/journal.pone.0177345
Hays RD, Spritzer KL, Schalet BD, Cella D (2018) PROMIS®-29 v2.0 profile physical and mental health summary scores. Qual Life Res 27(7):1885–1891. https://doi.org/10.1007/s11136-018-1842-3
van der Meij E, Anema JR, Huirne JAF, Terwee CB (2018) Using PROMIS for measuring recovery after abdominal surgery: a pilot study. BMC Health Serv Res 18(1):128. https://doi.org/10.1186/s12913-018-2929-9
Myles PS, Myles DB, Galagher W, Boyd D, Chew C, MacDonald N, Dennis A (2017) Measuring acute postoperative pain using the visual analog scale: the minimal clinically important difference and patient acceptable symptom state. Br J Anaesth 118(3):424–429. https://doi.org/10.1093/bja/aew466
HealthMeasures. PROMIS score cut points. https://staging.healthmeasures.net/score-and-interpret/interpret-scores/promis/promis-score-cut-points. Accessed 28 Mar 2023
Gordon DB, Polomano RC, Pellino TA, Turk DC, McCracken LM, Sherwood G, Paice JA, Wallace MS, Strassels SA, Farrar JT (2010) Revised American pain society patient outcome questionnaire (APS-POQ-R) for quality improvement of pain management in hospitalized adults: preliminary psychometric evaluation. J Pain 11(11):1172–1186. https://doi.org/10.1016/j.jpain.2010.02.012
Berkowitz R, Vu J, Brummett C, Waljee J, Englesbe M, Howard R (2021) The impact of complications and pain on patient satisfaction. Ann Surg 273(6):1127–1134. https://doi.org/10.1097/SLA.0000000000003621
Chowdhury MZI, Turin TC (2020) Variable selection strategies and its importance in clinical prediction modelling. Fam Med Community Health 8(1):e000262. https://doi.org/10.1136/fmch-2019-000262
Ip HY, Abrishami A, Peng PW, Wong J, Chung F (2009) Predictors of postoperative pain and analgesic consumption: a qualitative systematic review. Anesthesiology 111(3):657–677. https://doi.org/10.1097/ALN.0b013e3181aae87a
Nandi M, Schreiber KL, Martel MO, Cornelius M, Campbell CM, Haythornthwaite JA, Smith MT, Wright J, Aglio LS, Strichartz G, Edwards RR (2019) Sex differences in negative affect and postoperative pain in patients undergoing total knee arthroplasty. Biol Sex Differ 10(1):23. https://doi.org/10.1186/s13293-019-0237-7
Yang MMH, Hartley RL, Leung AA, Ronksley PE, Jetté N, Casha S, Riva-Cambrin J (2019) Preoperative predictors of poor acute postoperative pain control: a systematic review and meta-analysis. BMJ Open 9(4):e025091. https://doi.org/10.1136/bmjopen-2018-025091
Kinjo S, Sands LP, Lim E, Paul S, Leung JM (2012) Prediction of postoperative pain using path analysis in older patients. J Anesth 26(1):1–8. https://doi.org/10.1007/s00540-011-1249-6,October20,2011
Government of Ontario Anti-Racism Directorate (2018) Data standards for the identification and monitoring of systemic racism. https://www.ontario.ca/document/data-standards-identification-and-monitoring-systemic-racism. Accessed 13 Mar 2023
Perry M, Baumbauer K, Young EE, Dorsey SG, Taylor JY, Starkweather AR (2019) The influence of race, ethnicity and genetic variants on postoperative pain intensity: an integrative literature review. Pain Manag Nurs 20(3):198–206. https://doi.org/10.1016/j.pmn.2018.11.002
Nixon DC, Schafer KA, Cusworth B, McCormick JJ, Johnson JE, Klein SE (2019) Preoperative anxiety effect on patient-reported outcomes following foot and ankle surgery. Foot Ankle Int 40(9):1007–1011. https://doi.org/10.1177/1071100719850806
Christian Z, Afuwape O, Johnson ZD, Adeyemo E, Barrie U, Dosselman LJ, Pernik MN, Hall K, Aoun SG, Bagley CA (2021) Evaluating the impact of psychiatric disorders on preoperative pain ratings, narcotics use, and the PROMIS-29 quality domains in spine surgery candidates. Cureus 13(1):e12768. https://doi.org/10.7759/cureus.12768
Schreyer C, Salwen-Deremer JK, Montanari A, Holloway B, Coughlin JW (2018) Pain perceptions in bariatric surgery candidates: the role of pain catastrophizing. Surg Obes Relat Dis 14(11):S89. https://doi.org/10.1016/j.soard.2018.09.169
Sullivan MJL, Bishop SR, Pivik J (1995) The pain catastrophizing scale: development and validation. Psych Assess 7(4):524–532. https://doi.org/10.1037/1040-3590.7.4.524
Andrawis J, Akhavan S, Chan V, Lehil M, Pong D, Bozic KJ (2015) Higher preoperative patient activation associated with better patient-reported outcomes after total joint arthroplasty. Clin Orthop Relat Res 473(8):2688–2697. https://doi.org/10.1007/s11999-015-4247-4
Hibbard JH, Stockard J, Mahoney ER, Tusler M (2004) Development of the patient activation measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res 39(4–1):1005–1026. https://doi.org/10.1111/j.1475-6773.2004.00269.x
Doan LV, Blitz J (2020) Preoperative assessment and management of patients with pain and anxiety disorders. Curr Anesthesiol Rep 10(1):28–34. https://doi.org/10.1007/s40140-020-00367-9
Clark ME, Gironda RJ, Young RW (2003) Development and validation of the pain outcomes questionnaire-VA. J Rehabil Res Dev 40(5):381–395. https://doi.org/10.1682/jrrd.2003.09.0381
Willingham MD, Vila MR, Ben Abdallah A, Avidan MS, Haroutounian S (2021) Factors contributing to lingering pain after surgery: the role of patient expectations. Anesthesiology 134(6):915–924. https://doi.org/10.1097/ALN.0000000000003754
Maciejewski ML, Smith VA, Berkowitz TSZ, Arterburn DE, Bradley KA, Olsen MK, Liu CF, Livingston EH, Funk LM, Mitchell JE (2020) Long-term opioid use after bariatric surgery. Surg Obes Relat Dis 16(8):1100–1110. https://doi.org/10.1016/j.soard.2020.04.037
Hider AM, Bonham AJ, Carlin AM, Finks JF, Ghaferi AA, Varban OA, Ehlers AP (2022) Impact of concurrent hiatal hernia repair during laparoscopic sleeve gastrectomy on patient-reported gastroesophageal reflux symptoms: a state-wide analysis. Surg Obes Relat Dis 19(6):619–625. https://doi.org/10.1016/j.soard.2022.12.021
Tian C, Lee Y, Oparin Y, Hong D, Shanthanna H (2021) Benefits of transversus abdominis plane block on postoperative analgesia after bariatric surgery: a systematic review and meta-analysis. Pain Physician 24(5):345–358
Porter ED, Bessen SY, Molloy IB, Kelly JL, Ramkumar N, Phillips JD, Loehrer AP, Wilson MZ, Hasson RM, Ivatury SJ, Henkin JR, Barth RJ Jr (2021) Guidelines for patient-centered opioid prescribing and optimal FDA-compliant disposal of excess pills after inpatient operation: prospective clinical trial. J Am Coll Surg 232(6):823–835.e2. https://doi.org/10.1016/j.jamcollsurg.2020.12.057
Willingham M, Rangrass G, Curcuru C, Ben Abdallah A, Wildes TS, McKinnon S, Kronzer A, Sharma A, Helsten D, Hall B, Avidan MS, Haroutounian S (2020) Association between postoperative complications and lingering post-surgical pain: an observational cohort study. Br J Anaesth 124(2):214–221. https://doi.org/10.1016/j.bja.2019.10.012
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Bicket MC, Long JJ, Pronovost PJ, Alexander GC, Wu CL (2017) Prescription opioid analgesics commonly unused after surgery: a systematic review. JAMA Surg 152(11):1066–1071. https://doi.org/10.1001/jamasurg.2017.0831
Austin PC, Steyerberg EW (2015) The number of subjects per variable required in linear regression analyses. J Clin Epidemiol 68(6):627–636. https://doi.org/10.1016/j.jclinepi.2014.12.014
Jenkins DG, Quintana-Ascencio PF (2020) A solution to minimum sample size for regressions. PLoS ONE 15(2):e0229345. https://doi.org/10.1371/journal.pone.0229345
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR (1996) A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 49(12):1373–1379. https://doi.org/10.1016/s0895-4356(96)00236-3
Bursac Z, Gauss CH, Williams DK, Hosmer DW (2008) Purposeful selection of variables in logistic regression. Source Code Biol Med 3:17. https://doi.org/10.1186/1751-0473-3-17
Azur MJ, Stuart EA, Frangakis C, Leaf PJ (2011) Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res 20(1):40–49. https://doi.org/10.1002/mpr.329
Sterne JA, White IR, Carlin JB, Spratt M, Royston P, Kenward MG, Wood AM, Carpenter JR (2009) Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 338:b2393. https://doi.org/10.1136/bmj.b2393
Thabane L, Mbuagbaw L, Zhang S, Samaan Z, Marcucci M, Ye C, Thabane M, Giangregorio L, Dennis B, Kosa D, Borg Debono V, Dillenburg R, Fruci V, Bawor M, Lee J, Wells G, Goldsmith CH (2013) A tutorial on sensitivity analyses in clinical trials: the what, why, when and how. BMC Med Res Methodol 13:92. https://doi.org/10.1186/1471-2288-13-92
Petrini L, Arendt-Nielsen L (2020) Understanding pain catastrophizing: putting pieces together. Front Psychol 11:603420. https://doi.org/10.3389/fpsyg.2020.603420
Pogatzki-Zahn EM, Segelcke D, Schug SA (2017) Postoperative pain-from mechanisms to treatment. Pain Rep 2(2):e588. https://doi.org/10.1097/PR9.0000000000000588
Sipilä RM, Haasio L, Meretoja TJ, Ripatti S, Estlander AM, Kalso EA (2017) Does expecting more pain make it more intense? Factors associated with the first week pain trajectories after breast cancer surgery. Pain 158(5):922–930. https://doi.org/10.1097/j.pain.0000000000000859
Kain ZN, Sevarino F, Alexander GM, Pincus S, Mayes LC (2000) Preoperative anxiety and postoperative pain in women undergoing hysterectomy: a repeated-measure design. J Psychosom Res 49(6):417–422. https://doi.org/10.1016/s0022-3999(00)00189-6
Darnall BD (2016) Pain psychology and pain catastrophizing in the perioperative setting: a review of impacts, interventions, and unmet needs. Hand Clin 32(1):33–39. https://doi.org/10.1016/j.hcl.2015.08.005
Kleiman V, Clarke H, Katz J (2011) Sensitivity to pain traumatization: a higher-order factor underlying pain-related anxiety, pain catastrophizing and anxiety sensitivity among patients scheduled for major surgery. Pain Res Manag 16(3):169–177. https://doi.org/10.1155/2011/932590
Khorfan R, Shallcross ML, Yu B, Sanchez N, Parilla S, Coughlin JM, Johnson JK, Bilimoria KY, Stulberg JJ (2020) Preoperative patient education and patient preparedness are associated with less postoperative use of opioids. Surgery 167(5):852–858. https://doi.org/10.1016/j.surg.2020.01.002
Villa G, Lanini I, Amass T, Bocciero V, Scirè Calabrisotto C, Chelazzi C, Romagnoli S, De Gaudio AR, Lauro Grotto R (2020) Effects of psychological interventions on anxiety and pain in patients undergoing major elective abdominal surgery: a systematic review. Perioper Med (Lond) 9(1):38. https://doi.org/10.1186/s13741-020-00169-x
Sariati S, Yunitasari E, Hidayati L (2020) Education-based mobile apps platform in patients undergoing surgery: a systematic review. Jurnal Ners 15:19–24. https://doi.org/10.20473/jn.v15i1Sp.18899
Akca A, Yilmaz G, Esmer AC, Yuksel S, Koroglu N, Cetin BA (2020) Use of video-based multimedia information to reduce anxiety before office hysteroscopy. Wideochir Inne Tech Maloinwazyjne 15(2):329–336. https://doi.org/10.5114/wiitm.2019.89378
Prakash B (2010) Patient satisfaction. J Cutan Aesthet Surg 3(3):151–155. https://doi.org/10.4103/0974-2077.74491
Harris AB, Kebaish F, Riley LH, Kebaish KM, Skolasky RL (2020) The engaged patient: patient activation can predict satisfaction with surgical treatment of lumbar and cervical spine disorders. J Neurosurg Spine 7:1–7. https://doi.org/10.3171/2019.11.SPINE191159
Dumitra T, Ganescu O, Hu R, Fiore JF Jr, Kaneva P, Mayo N, Lee L, Liberman AS, Chaudhury P, Ferri L, Feldman LS (2022) Association between patient activation and health care utilization after thoracic and abdominal surgery. JAMA Surg 156(1):e205002. https://doi.org/10.1001/jamasurg.2020.5002
Shah VO, Carroll C, Mals R, Ghahate D, Bobelu J, Sandy P, Colleran K, Schrader R, Faber T, Burge MR (2015) A home-based educational intervention improves patient activation measures and diabetes health indicators among Zuni Indians. PLoS ONE 10(5):e0125820. https://doi.org/10.1371/journal.pone.0125820
Imeri H, Desselle S, Hetemi D, Hoti K (2021) Mobile electronic devices as means of facilitating patient activation and health professional empowerment related to information seeking on chronic conditions and medications: qualitative study. JMIR Mhealth Uhealth 9(8):e26300. https://doi.org/10.2196/26300
You DS, Ziadni MS, Hettie G, Darnall BD, Cook KF, Von Korff MR, Mackey SC (2022) Comparing perceived pain impact between younger and older adults with high impact chronic pain: a cross-sectional qualitative and quantitative survey. Front Pain Res (Lausanne) 3:850713. https://doi.org/10.3389/fpain.2022.850713
Rahmqvist M (2001) Patient satisfaction in relation to age, health status and other background factors: a model for comparisons of care units. Int J Qual Health Care 13(5):385–390. https://doi.org/10.1093/intqhc/13.5.385
Altman DG, Royston P (2006) The cost of dichotomising continuous variables. BMJ 332(7549):1080. https://doi.org/10.1136/bmj.332.7549.1080
Aamir MA, Sahebally SM, Heneghan H (2021) Transversus abdominis plane block in laparoscopic bariatric surgery—a systematic review and meta-analysis of randomized controlled trials. Obes Surg 31(1):133–142. https://doi.org/10.1007/s11695-020-04898-2
Boerboom SL, de Haes A, Vd Wetering L, Aarts EO, Janssen IMC, Geurts JW, Kamphuis ET (2018) Preperitoneal bupivacaine infiltration reduces postoperative opioid consumption, acute pain, and chronic postsurgical pain after bariatric surgery: a randomized controlled trial. Obes Surg 28(10):3102–3110. https://doi.org/10.1007/s11695-018-3341-6
Stamenkovic DM, Bezmarevic M, Bojic S, Unic-Stojanovic D, Stojkovic D, Slavkovic DZ, Bancevic V, Maric N, Karanikolas M (2021) Updates on wound infiltration use for postoperative pain management: a narrative review. J Clin Med 10(20):4659. https://doi.org/10.3390/jcm10204659
Wilson JA, Romagnuolo J, Byrne TK, Morgan K, Wilson FA (2006) Predictors of endoscopic findings after Roux-en-Y gastric bypass. Am J Gastroenterol 101(10):2194–2199. https://doi.org/10.1111/j.1572-0241.2006.00770.x
Coblijn UK, Goucham AB, Lagarde SM, Kuiken SD, van Wagensveld BA (2014) Development of ulcer disease after Roux-en-Y gastric bypass, incidence, risk factors, and patient presentation: a systematic review. Obes Surg 24(2):299–309. https://doi.org/10.1007/s11695-013-1118-5
Begian A, Samaan JS, Hawley L, Alicuben ET, Hernandez A, Samakar K (2021) The use of nonsteroidal anti-inflammatory drugs after sleeve gastrectomy. Surg Obes Relat Dis 17(3):484–488. https://doi.org/10.1016/j.soard.2020.11.016
Erdogan Kayhan G, Sanli M, Ozgul U, Kirteke R, Yologlu S (2018) Comparison of intravenous ibuprofen and acetaminophen for postoperative multimodal pain management in bariatric surgery: a randomized controlled trial. J Clin Anesth 50(5–11):2018. https://doi.org/10.1016/j.jclinane.2018.06.030,June20
Abou Zeid H, Kallab R, Najm MA, Jabbour H, Noun R, Sleilati F, Chucri S, Dagher C, Sleilaty G, Naccache N (2019) Safety and efficacy of non-steroidal anti-inflammatory drugs (NSAIDs) used for analgesia after bariatric surgery: a retrospective case-control study. Obes Surg 29(3):911–916. https://doi.org/10.1007/s11695-018-3608-y
Scott MJ, McEvoy MD, Gordon DB, Grant SA, Thacker JKM, Wu CL, Gan TJ, Mythen MG, Shaw AD, Miller TE et al (2017) American Society for Enhanced Recovery (ASER) and Perioperative Quality Initiative (POQI) joint consensus statement on optimal analgesia within an enhanced recovery pathway for colorectal surgery: part 2—from PACU to the transition home. Perioper Med (Lond) 6:7.https://doi.org/10.1186/s13741-017-0063-6
Acknowledgements
The authors would also like to acknowledge the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) for their financial support in making this research possible.
Funding
This study was funded by a Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) Grant awarded to Dr. Julio Fiore Jr., Dr. Amin Andalib, and Dr. Michel Gagner.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Julio F. Fiore Jr., Amin Andalib, and Michel Gagner received a research grant from the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) to conduct this study. Maxime Lapointe-Gagner, Shrieda Jain, Naser Alali, Hiba Elhaj, Anne-Sophie Poirier, Pepa Kaneva, Mohsen Alhashemi, Raman Agnihotram, Lawrence Lee, and Liane Feldman have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lapointe-Gagner, M., Jain, S., Alali, N. et al. Predictors of post-discharge pain and satisfaction with pain management after laparoscopic bariatric surgery: a prospective cohort study. Surg Endosc 37, 8611–8622 (2023). https://doi.org/10.1007/s00464-023-10307-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10307-3