Abstract
Background
Diverting ileostomy and colostomy after total mesorectal excision reduces the risk of complications related to anastomotic leakages but is associated with a reduction in health-related quality of life and long-term economic consequences that are unknown. Our objective was to estimate the lifetime costs of stoma placement after rectal cancer resection in the U.S., England, and Germany.
Methods
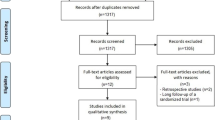
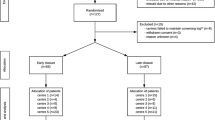
Input parameters were derived from quasi-systematic literature searches. Decision-analytic models with survival from colorectal cancer-adjusted life tables and country-specific stoma reversal proportions were created for the three countries to calculate lifetime costs. Main cost items were stoma maintenance costs and reimbursement for reversal procedures. Discounting was applied according to respective national guidelines. Sensitivity analysis was conducted to explore the impact of parameter uncertainty onto the results.
Results
The cohort starting ages and median survival were 63 and 11.5 years for the U.S., 69 years and 8.5 years for England, and 71 and 6.5 years for Germany. Lifetime discounted stoma-related costs were $26,311, £9512, and €10,021, respectively. All three models were most sensitive to the proportion of ostomy reversal, age at baseline, and discount rate applied.
Conclusion
Conservative model-based projections suggest that stoma care leads to significant long-term costs. Efforts to reduce the number of patients who need to undergo a diverting ostomy could result in meaningful cost savings.



Similar content being viewed by others
References
Schiergens TS, Hoffmann V, Schobel TN et al (2017) Long-term quality of life of patients with permanent end ileostomy: results of a nationwide cross-sectional survey. Dis Colon Rectum 60(1):51–60
Vonk-Klaassen SM, de Vocht HM, den Ouden ME, Eddes EH, Schuurmans MJ (2016) Ostomy-related problems and their impact on quality of life of colorectal cancer ostomates: a systematic review. Qual Life Res 25(1):125–133
Maydick Youngberg D (2014) Individuals with a permanent ostomy: quality of life and out-of-pocket financial costs for ostomy management. Nurs Econ 32:204
LeBlanc K, Heerschap C, Martins L, Butt B, Wiesenfeld S, Woo K (2019) The financial impact of living in Canada with an ostomy: a cross-sectional survey. J Wound Ostomy Cont Nurs 46(6):505–512
Dodgion CM, Neville BA, Lipsitz SR et al (2013) Do older Americans undergo stoma reversal following low anterior resection for rectal cancer? J Surg Res 183(1):238–245
Gadan S, Lindgren R, Floodeen H, Matthiessen P (2019) Reversal of defunctioning stoma following rectal cancer surgery: are we getting better? A population-based single centre experience. ANZ J Surg 89(4):403–407
Gessler B, Haglind E, Angenete E (2012) Loop ileostomies in colorectal cancer patients–morbidity and risk factors for nonreversal. J Surg Res 178(2):708–714
Taneja C, Netsch D, Rolstad BS, Inglese G, Eaves D, Oster G (2019) Risk and economic burden of peristomal skin complications following ostomy surgery. J Wound Ostomy Cont Nurs 46(2):143–149
Colwell JC, Pittman J, Raizman R, Salvadalena G (2018) A randomized controlled trial determining variances in ostomy skin conditions and the economic impact (Advocate Trial). J Wound Ostomy Cont Nurs 45(1):37–42
Maneesin S, Sampatanukul P, Lertmaharit S, Nagara CN, Prasopsanti K (2017) Health-related quality of life of patients living with ostomy in Thailand and cost implications. Asian Biomed 6(2):235–243
Vanleene V, De Mare L, Moldenaers I et al (2008) Estimation and comparison of ostomy appliance costs with tariffs in Belgium. Eur J Health Econ 9(1):17–22
Husereau D, Drummond M, Augustovski F, Standards Consolidated Health Economic Evaluation Reporting et al (2022) (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. Int J Technol Assess Health Care. https://doi.org/10.1017/S0266462321001732
Centers for Medicare Medicaid Services (2021) Medicare program; hospital inpatient prospective payment systems for acute care hospitals and the long‑term care hospital prospective payment system and policy changes and fiscal year 2022 rates; quality programs and Medicare promoting interoperability program requirements for eligible hospitals and critical access hospitals; changes to Medicaid provider enrollment; and changes to the Medicare shared savings program. Federal Register. https://www.federalregister.gov/documents/2021/08/13/2021-16519/medicare-program-hospital-inpatient-prospective-payment-systems-for-acute-care-hospitals-and-the
Centers for Medicare Medicaid Services (2020) July 2020 DMEPOS Fee Schedule Update. https://www.cms.gov/medicaremedicare-fee-service-paymentdmeposfeescheddmepos-feeschedule/dme20-c
Bassy N, Libutzki B (2019) PCN529 burden of illness in new ostomates: an analysis based on German claims data. Value Health. https://doi.org/10.1016/j.jval.2019.09.720
Macleod A, Stewart C (2019) National stoma quality improvement SLWG (NSQIG) final report. Scottish Executive Nurse Director Group (SEND). https://cdn.ps.emap.com/wp-content/uploads/sites/3/2020/08/STOMA-report-2020-Final.pdf
Kettle J (2019) East of England NHS Collaborative Procurement Hub Integrated Care Team StoMap Programme Baseline Report 2019. https://www.eoecph.nhs.uk/Files/Integrated%20Care/StoMap%20Baseline%20Report%20FINAL%20amended%2011.12.19.pdf
Batty L, Dillon A, Downing M, Kightley S, Hargreaves S, Smith J, Robinson J (2012) NHS Northamptonshire comprehensive stoma care guidelines. Information for general practitioners. https://1library.net/document/zlvm2g2y-northamptonshire-comprehensive-stoma-care-guidelines-information-general-practitioners.html
Institut für das Entgeltsystem im Krankenhaus (2021) Fallpauschalen-Katalog 2022. https://www.g-drg.de/ag-drg-system-2022/fallpauschalen-katalog/fallpauschalen-katalog-2022
DRG-Research Group. Webgrouper. https://www.drg-research-group.de/index.php?option=com_webgrouper&Itemid=107&view=webgrouper
Williams AO, Rojanasarot S, McGovern AM, Kumar A (2022) A systematic review of discounting in national health economic evaluation guidelines: healthcare value implications. J Comp Eff Res. https://doi.org/10.2217/cer-2022-0167
Arias E, Xu JQ (2022) United States life tables, 2019. National Vital Statistics Reports 70(19). Hyattsville, MD: National Center for Health Statistics. https://doi.org/10.15620/cdc:113096
Ries LAG, Melbert D, Krapcho M, Stinchcomb DG, Howlader N, Horner MJ, Mariotto A, Miller BA, Feuer EJ, Altekruse SF, Lewis DR, Clegg L, Eisner MP, Reichman M, Edwards BK (eds) (2008) SEER Cancer Statistics Review, 1975-2005, National Cancer Institute. Bethesda, MD. https://seer.cancer.gov/csr/1975_2005/
Surveillance Epidemiology and End Results Program (2019) Colon and rectum SEER relative survival rates by time since diagnosis, 2000–2018, by sex, all races, all ages, all stages. National Cancer Institute. https://seer.cancer.gov/statistics-network/explorer/application.html?site=20&data_type=4&graph_type=2&compareBy=sex&chk_sex_3=3&chk_sex_2=2&relative_survival_interval=5&race=1&age_range=1&stage=101&advopt_precision=1&advopt_show_ci=on&hdn_view=0&advopt_show_apc=on&advopt_display=2#resultsRegion0
Public Health England (2020) Geographical patterns of cancer survival in England: adults diagnosed 2014 to 2018 and followed up to 2019. https://view.officeapps.live.com/op/view.aspx?src=https%3A%2F%2Fassets.publishing.service.gov.uk%2Fgovernment%2Fuploads%2Fsystem%2Fuploads%2Fattachment_data%2Ffile%2F932964%2Fadultcancerfinal_ods_update051120.ods&wdOrigin=(2020).
Office for National Statistics (2021) National life tables: UK. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/lifeexpectancies/datasets/nationallifetablesunitedkingdomreferencetables
Munich Cancer Registry (2021) ICD-10 C18-C20: colorectal cancer incidence and mortality Munich, Germany
Munich Cancer Registry (2021) ICD-10 C18-C20: colorectal cancer survival. Munich, Germany
Kaufmännische Krankenkasse. Leitfaden für den Vertragsbeitritt gemäß § 127 Abs. 2 SGB V, 2022
Majano SB, Di Girolamo C, Rachet B et al (2019) Surgical treatment and survival from colorectal cancer in Denmark, England, Norway, and Sweden: a population-based study. Lancet Oncol 20(1):74–87
Siegel RL, Miller KD, Goding Sauer A et al (2020) Colorectal cancer statistics, 2020. Cancer J Clin 70(3):145–64
Statistisches Bundesamt (Destatis) (2022) Deaths, life expectancy GENESIS-Online. Die Datenbank des Statistischen Bundesamtes des Statistischen Bundesamtes. https://www.destatis.de/EN/Themes/Society-Environment/Population/Deaths-Life-Expectancy/database-teaser.html
National Bowel Cancer Audit commissioned by the Healthcare Quality Improvement Partnership (HQIP) (2020) National Bowel Cancer Audit Annual Report. https://www.nboca.org.uk/content/uploads/2020/12/NBOCA-2020-Annual-Report.pdf
Sier M, Van Gelder L, Ubbink D, Bemelman W, Oostenbroek R (2015) Factors affecting timing of closure and non-reversal of temporary ileostomies. Int J Colorectal Dis 30(9):1185–1192
Liu C, Bhat S, Sharma P, Yuan L, O’Grady G, Bissett I (2021) Risk factors for readmission with dehydration after ileostomy formation: a systematic review and meta-analysis. Colorectal Dis 23(5):1071–1082
Keller DS, Khorgami Z, Swendseid B, Khan S, Delaney CP (2014) Identifying causes for high readmission rates after stoma reversal. Surg Endosc 28(4):1263–1268
Bailey C, Wheeler J, Birks M, Farouk R (2003) The incidence and causes of permanent stoma after anterior resection. Colorectal Dis 5(4):331–334
Lordan J, Heywood R, Shirol S, Edwards D (2007) Following anterior resection for rectal cancer, defunctioning ileostomy closure may be significantly delayed by adjuvant chemotherapy: a retrospective study. Colorectal Dis 9(5):420–422
De Hous N, Lefevre J, D’Urso A, Van den Broeck S, Komen N (2020) Intraluminal bypass devices as an alternative to protective ostomy for prevention of colorectal anastomotic leakage: a systematic review of the literature. Colorectal Dis 22(11):1496–1505
De Hous N, Khosrovani C, Lefevre JH, D’Urso A, Komen N (2022) Evaluation of the SafeHeal Colovac+ anastomosis protection device: a preclinical study. Surg Innov. https://doi.org/10.1177/15533506211051274
D’urso A, Komen N, Lefevre JH, (2020) Intraluminal flexible sheath for the protection of low anastomosis after anterior resection: results from a first-in-human trial on 15 patients. Surg Endosc 34:5107–5116
Kang SI, Kim S, Kim JH (2022) Two-year follow-up results of the use of a fecal diverting device as a substitute for a defunctioning stoma. Int J Colorectal Dis 37(4):835–841
Reshef A, Ben-Arie G, Pinsk I (2019) Protection of colorectal anastomosis with an intraluminal bypass device for patients undergoing an elective anterior resection: a pilot study. Tech Coloproctol 23:565–571
Rolls N, Yssing C, Bøgelund M, Håkan-Bloch J, de Fries JL (2022) Utilities associated with stoma-related complications: peristomal skin complications and leakages. J Med Econ 25(1):1005–1014
Meisner S, Lehur P-A, Moran B, Martins L, Jemec GBE (2012) Peristomal skin complications are common, expensive, and difficult to manage: a population based cost modeling study. PLoS ONE 7(5):e37813
Maydick DR (2014) Individuals with a permanent ostomy: quality of life and out-of-pocket financial costs for ostomy management. Nurs Econ 32(4):204
Coons SJ, Chongpison Y, Wendel CS, Grant M, Krouse RS (2007) Overall quality of life and difficulty paying for ostomy supplies in the veterans affairs ostomy health-related quality of life study: an exploratory analysis. Med Care 45:891–895
Buckley BS, Gonzalez JPS, Razon-Gonzalez EVB, Lopez MPJ (2012) The people that the ostomy industry forgot. Br J Gen Pract 62(603):544–545
Acknowledgements
The authors would like to express their gratitude to Gerd Gottschalk for collaborating on earlier stages of this work and to Simon Weber for his help in data collection and visualization.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Wing Tech Inc. (Dr. Khoa N. Cao, Anne M. Ryschon, Dr. Jan B. Pietzsch, and—during employment—Dr, Benjamin O. Geisler) has received consulting fees from SafeHeal SAS, a maker of an investigational device to avoid or reduce stoma. Drs. Geisler, Cao, and Pietzsch and Ms. Ryschon report no other relevant conflicts of interest. Dr. Karim Alavi and Niels Komen have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Geisler, B.P., Cao, K.N., Ryschon, A.M. et al. Cost associated with diverting ostomy after rectal cancer surgery: a transnational analysis. Surg Endosc 37, 7759–7766 (2023). https://doi.org/10.1007/s00464-023-10300-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10300-w