Abstract
Background
Post-lung transplant gastroparesis is a frequent debilitating complication of lung transplant recipients, as it can increase the risk for gastro-esophageal reflux disease and subsequent graft dysfunction. We performed a systematic review and meta-analysis to evaluate the efficacy and safety of GPOEM in lung transplant patients with refractory gastroparesis.
Methods
The present systematic review and meta-analysis wer performed according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses guidelines. We selected studies that analyzed the gastroparesis cardinal symptom index (GCSI) before and after the procedure to verify the efficacy of GPOEM. Random-effects model was used and the analysis was performed with STATA 17.
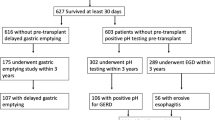
Results
Four observational studies (one conference abstract) with 104 patients were included in the meta-analysis. Prior treatments for gastroparesis included prokinetic agents and botulinum toxin in 78% (78/104) and 66.7% (66/99), respectively. Pooled estimate for clinical efficacy of GPOEM was 83% (95% CI 76%–90%). The pooled mean reduction in GCSI following the procedure was − 2.01 (− 2.35, − 1.65, p = 0.014). Three studies reported statistically significant improvement of gastro-esophageal retention or emptying in the post-GPOEM period. 30-day post-operative complications included minor or major bleeding (11.6%), severe reflux (1.2%), and pyloric stenosis (1.2%) requiring re-intervention. 90-day all-cause mortality was 2.6% with one patient dying from severe allograft rejection.
Conclusion
Our study showed that GPOEM is an effective and safe strategy for lung transplant patients with refractory gastroparesis and should be considered as a therapeutic strategy in this population. Larger multicenter trials are needed in the future to further evaluate the effect of GPOEM on allograft function and rates of rejection.



Similar content being viewed by others
References
Bobadilla JL, Jankowska-Gan E, Xu Q et al (2010) Reflux-induced collagen type v sensitization: potential mediator of bronchiolitis obliterans syndrome. Chest 138(2):363–370. https://doi.org/10.1378/chest.09-2610
Verleden GM, Besse T, Maes B (2002) Successful conversion from cyclosporine to tacrolimus for gastric motor dysfunction in a lung transplant recipient. Transplantation 73(12):1974–1976. https://doi.org/10.1097/00007890-200206270-00027
Suen HC, Hendrix H, Patterson GA (1999) Physiologic consequences of pneumonectomy. Consequences on the esophageal function. Chest Surg Clin N Am 9(2):475–483
Kayawake H, Chen-Yoshikawa TF, Motoyama H et al (2018) Gastrointestinal complications after lung transplantation in Japanese patients. Surg Today 48(9):883–890. https://doi.org/10.1007/s00595-018-1666-3
Raviv Y, D’Ovidio F, Pierre A et al (2012) Prevalence of gastroparesis before and after lung transplantation and its association with lung allograft outcomes. Clin Transplant 26(1):133–142. https://doi.org/10.1111/j.1399-0012.2011.01434.x
Jamie Dy F, Freiberger D, Liu E, Boyer D, Visner G, Rosen R (2017) Impact of gastroesophageal reflux and delayed gastric emptying on pediatric lung transplant outcomes. J Hear Lung Transplant 36(8):854–861. https://doi.org/10.1016/j.healun.2017.01.005
Bodet-Milin C, Querellou S, Oudoux A et al (2006) Delayed gastric emptying scintigraphy in cystic fibrosis patients before and after lung transplantation. J Hear Lung Transplant 25(9):1077–1083. https://doi.org/10.1016/j.healun.2006.04.013
Berkowitz N, Schulman LL, McGregor C, Markowitz D (1995) Gastroparesis after lung transplantation. Potential role in postoperative respiratory complications. Chest 108(6):1602–1607. https://doi.org/10.1378/chest.108.6.1602
Ahmad S, Shlobin OA, Nathan SD (2011) Pulmonary complications of lung transplantation. Chest 139(2):402–411. https://doi.org/10.1378/chest.10-1048
Adegunsoye A, Strek ME, Garrity E, Guzy R, Bag R (2017) Comprehensive care of the lung transplant patient. Chest 152(1):150–164. https://doi.org/10.1016/j.chest.2016.10.001
Arjuna A, Olson MT, Walia R, Bremner RM, Smith MA, Mohanakumar T (2021) An update on current treatment strategies for managing bronchiolitis obliterans syndrome after lung transplantation. Expert Rev Respir Med 15(3):339–350. https://doi.org/10.1080/17476348.2021.1835475
Camilleri M, Kuo B, Nguyen L et al (2022) ACG clinical guideline: gastroparesis. Am J Gastroenterol 117(8):1197–1220. https://doi.org/10.14309/ajg.0000000000001874
Bai Y, Xu M-J, Yang X et al (2010) A systematic review on intrapyloric botulinum toxin injection for gastroparesis. Digestion 81(1):27–34. https://doi.org/10.1159/000235917
Khashab MA, Stein E, Clarke JO et al (2013) Gastric peroral endoscopic myotomy for refractory gastroparesis: first human endoscopic pyloromyotomy (with video). Gastrointest Endosc 78(5):764–768. https://doi.org/10.1016/j.gie.2013.07.019
Spadaccini M, Maselli R, Chandrasekar VT et al (2020) Gastric peroral endoscopic pyloromyotomy for refractory gastroparesis: a systematic review of early outcomes with pooled analysis. Gastrointest Endosc 91(4):746-752.e5. https://doi.org/10.1016/j.gie.2019.11.039
AghaieMeybodi M, Qumseya BJ, Shakoor D et al (2019) Efficacy and feasibility of GPOEM in management of patients with refractory gastroparesis: a systematic review and meta-analysis. Endosc Int open 7(3):E322–E329. https://doi.org/10.1055/a-0812-1458
Martinek J, Hustak R, Mares J et al (2022) Endoscopic pyloromyotomy for the treatment of severe and refractory gastroparesis: a pilot, randomised, sham-controlled trial. Gut 71(11):2170–2178. https://doi.org/10.1136/gutjnl-2022-326904
Rappaport JMP, Raja S, Gabbard S et al (2022) Endoscopic pyloromyotomy is feasible and effective in improving post-lung transplant gastroparesis. J Thorac Cardiovasc Surg 164(3):711-719.e4. https://doi.org/10.1016/j.jtcvs.2021.10.063
Ichkhanian Y, Hwang JH, Ofosu A et al (2022) Role of gastric per-oral endoscopic myotomy (GPOEM) in post-lung transplant patients: a multicenter experience. Endosc Int open 10(6):E832–E839. https://doi.org/10.1055/a-1797-9587
Vitton V, BenoîtD’Journo X, Reynaud-Gaubert M, Barthet M, Gonzalez J-M (2021) Gastric peroral endoscopic myotomy (GPOEM) for severe gastroparesis after lung transplantation: A promising minimally invasive option. Clin Transplant 35(9):e14434. https://doi.org/10.1111/ctr.14434
Li A, Ofosu A, Kim W, Podboy A, Esquivel M, Hwang JH (2021) Gastric peroral endoscopic myotomy (GPOEM) improves symptoms and need for hospital admission for gastroparesis and lung transplant patients. Am J Gastroenterol 116:S466
Xu J, Chen T, Elkholy S et al (2018) Gastric peroral endoscopic myotomy (GPOEM) as a treatment for refractory gastroparesis: long-term outcomes. Can J Gastroenterol Hepatol 2018:6409698. https://doi.org/10.1155/2018/6409698
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Revicki DA, Rentz AM, Dubois D et al (2003) Development and validation of a patient-assessed gastroparesis symptom severity measure: the gastroparesis cardinal symptom index. Aliment Pharmacol Ther 18(1):141–150. https://doi.org/10.1046/j.1365-2036.2003.01612.x
Wells G, Shea B, O’Connell D et al (2014) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Podboy A, Clarke J, Nguyen L, Mooney J, Dhillon GS, Hwang J (2020) Outcomes of gastric per-oral endoscopic pyloromyotomy for severe gastroparesis in a lung transplant patient population. J Hear Lung Transplant 39(4):S317. https://doi.org/10.1016/j.healun.2020.01.714
Ichkhanian Y, Vosoughi K, AghaieMeybodi M et al (2021) Comprehensive analysis of adverse events associated with gastric peroral endoscopic myotomy: an international multicenter study. Surg Endosc 35(4):1755–1764. https://doi.org/10.1007/s00464-020-07570-z
Kamal F, Khan MA, Lee-Smith W et al (2022) Systematic review with meta-analysis: one-year outcomes of gastric peroral endoscopic myotomy for refractory gastroparesis. Aliment Pharmacol Ther 55(2):168–177. https://doi.org/10.1111/apt.16725
Spadaccini M, Maselli R, Thoguluva-Chandrasekar V et al (2019) Gastricperoral endoscopic pyloromyotomy for refractory gastroparesis: a systematic review with pooled analysis. United Eur Gastroenterol J 7(8):975–976. https://doi.org/10.1177/205064061985467
Khush KK, Cherikh WS, Chambers DC et al (2018) The international thoracic organ transplant registry of the international society for heart and lung transplantation: thirty-fifth adult heart transplantation report-2018; focus theme: multiorgan transplantation. J Hear lung Transplant Off Publ Int Soc Hear Transplant 37(10):1155–1168. https://doi.org/10.1016/j.healun.2018.07.022
Hathorn KE, Chan WW, Lo W-K (2017) Role of gastroesophageal reflux disease in lung transplantation. World J Transplant 7(2):103–116. https://doi.org/10.5500/wjt.v7.i2.103
Li A, Ofosu A, Kim W, Podboy A, Esquivel M, Hwang JH (2021) Gastric peroral endoscopic myotomy (GPOEM) improves symptoms and need for hospital admission for gastroparesis and lung transplant patients. Am J Gastroenterol 116:S466. https://doi.org/10.1409/01.ajg.0000777436.28650.16
Verleden SE, Sacreas A, Vos R, Vanaudenaerde BM, Verleden GM (2016) Advances in understanding bronchiolitis obliterans after lung transplantation. Chest 150(1):219–225. https://doi.org/10.1016/j.chest.2016.04.014
Blackett JW, Benvenuto L, Leiva-Juarez MM, D’Ovidio F, Arcasoy S, Jodorkovsky D (2022) Risk Factors and outcomes for gastroparesis after lung transplantation. Dig Dis Sci 67(6):2385–2394. https://doi.org/10.1007/s10620-021-07249-y
Derousseau T, Chan WW, Cangemi D, Kaza V, Lo W-K, Gavini S (2022) Delayed gastric emptying in prelung transplant patients is associated with posttransplant acute cellular rejection independent of reflux. J Clin Gastroenterol 56(2):e121–e125. https://doi.org/10.1097/MCG.0000000000001502
Funding
This research received no specific grant support from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Spyridon Peppas, Dr. Akram I Ahmad, Dr. Nadera Altork, and Dr. Won Kyoo Cho have no conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Peppas, S., Ahmad, A.I., Altork, N. et al. Efficacy and safety of gastric per-oral endoscopic myotomy (GPOEM) in lung transplant patients with refractory gastroparesis: a systematic review and meta-analysis. Surg Endosc 37, 6695–6703 (2023). https://doi.org/10.1007/s00464-023-10287-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10287-4