Abstract
Background
It is increasingly recognized that complex abdominal wall reconstruction (cAWR) necessitates specialized training. No studies have been conducted to assess whether a volume-outcomes relationship is present in cAWR. We sought to determine if outcomes for patients undergoing cAWR varied based on surgeon volume among participants in the Abdominal Core Health Quality Collaborative (ACHQC).
Methods
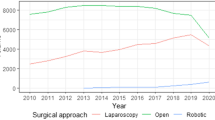
All patients with ventral hernias undergoing elective cAWR with component separation (lateral component release) were selected from ACHQC database. Surgeons were ranked based on annual number of cAWR procedures performed and then grouped in tertiles. Patient characteristics, hernia risk factors, operative details, and 30-days outcomes were evaluated.
Results
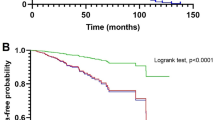
A total of 9206 patients were identified, of which 310 (3.4%), 723 (7.9%) and 8173 (88.7%) cAWRs were performed by low (105 surgeons), medium (49) and high-volume (66) surgeons, respectively. Patients operated upon by high-volume surgeons tended to have more comorbidities and higher ASA class (72.5% of class ≥ III, vs 53.5%). Hernia characteristics demonstrated that high-volume surgeons more commonly operated on patients presenting with recurrent hernias (50.2% vs 42%), wider hernias (13.5 cm vs 10.5 cm), associated ostomies (13% vs 3.6%), and prior of surgical site infections (32% vs 26%, P = 0.035). High-volume surgeons more commonly performed posterior component separation procedures (92% vs 84%), utilized permanent mesh (92% vs 88%), and placed mesh in sublay position. In spite of operating on more advanced hernias, high-volume surgeons achieved comparable rates (all P > 0.4) of 30-day surgical site infections (SSI: 6.9% vs 7.1%) and surgical site occurrences requiring procedural intervention (SSO-PI: 8.9% vs 10%).
Conclusions
High-volume surgeons maintain comparable outcomes following cAWR despite performing operations on patients with more comorbidities and advanced hernia disease. These findings should be integrated into the debates related to regionalizing abdominal wall reconstruction procedures among high-volume surgeons.


Similar content being viewed by others
References
Martin-Del-Campo LA, Weltz AS, Belyansky I, Novitsky YW (2018) Comparative analysis of perioperative outcomes of robotic versus open transversus abdominis release. Surg Endosc 32(2):840–845
Belyansky I, Daes J, Radu VG, Balasubramanian R, Reza Zahiri H, Weltz AS, Sibia US, Park A, Novitsky Y (2018) A novel approach using the enhanced-view totally extraperitoneal (eTEP) technique for laparoscopic retromuscular hernia repair. Surg Endosc 32(3):1525–1532
Novitsky YW, Fayezizadeh M, Majumder A, Neupane R, Elliott HL, Orenstein SB (2016) Outcomes of posterior component separation with transversus abdominis muscle release and synthetic mesh sublay reinforcement. Ann Surg 264(2):226–232
Krpata DM, Blatnik JA, Novitsky YW, Rosen MJ (2012) Posterior and open anterior components separations: a comparative analysis. Am J Surg 203(3):318–322 (discussion 322)
Shulkin JM, Mellia JA, Patel V, Naga HI, Morris MP, Christopher A, Heniford BT, Fischer JP (2022) Characterizing hernia centers in the United States: what defines a hernia center? Hernia 26(1):251–257
Pauli EM, Rosen MJ (2013) Open ventral hernia repair with component separation. Surg Clin N Am 93(5):1111–1133
Brennan M, Wong S, Faringer PD, Lim JH (2021) Head and neck tumor resection and free flap reconstruction in low-volume center. Ear Nose Throat J 100(9):647–650
Chowdhury MM, Dagash H, Pierro A (2007) A systematic review of the impact of volume of surgery and specialization on patient outcome. Br J Surg 94(2):145–161
Kockerling F, Sheen AJ, Berrevoet F, Campanelli G, Cuccurullo D, Fortelny R, Friis-Andersen H, Gillion JF, Gorjanc J, Kopelman D et al (2019) The reality of general surgery training and increased complexity of abdominal wall hernia surgery. Hernia 23(6):1081–1091
Albornoz CR, Cordeiro PG, Hishon L, Mehrara BJ, Pusic AL, McCarthy CM, Disa JJ, Matros E (2013) A nationwide analysis of the relationship between hospital volume and outcome for autologous breast reconstruction. Plast Reconstr Surg 132(2):192e–200e
Tuggle CT, Patel A, Broer N, Persing JA, Sosa JA, Au AF (2014) Increased hospital volume is associated with improved outcomes following abdominal-based breast reconstruction. J Plast Surg Hand Surg 48(6):382–388
Billig JI, Lu Y, Momoh AO, Chung KC (2017) A nationwide analysis of cost variation for autologous free flap breast reconstruction. JAMA Surg 152(11):1039–1047
DeBord J, Novitsky Y, Fitzgibbons R, Miserez M, Montgomery A (2018) SSI, SSO, SSE, SSOPI: the elusive language of complications in hernia surgery. Hernia 22(5):737–738
Cunningham AJ, Howell B, Polites S, Krishnaswami S, Hughey E, Terry S, Fox J, Azarow K (2020) Establishing best practices for structured NSQIP review. Am J Surg 219(5):865–868
Sugerman HJ, Kellum JM Jr, Reines HD, DeMaria EJ, Newsome HH, Lowry JW (1996) Greater risk of incisional hernia with morbidly obese than steroid-dependent patients and low recurrence with prefascial polypropylene mesh. Am J Surg 171(1):80–84
Kulkarni GS, Urbach DR, Austin PC, Fleshner NE, Laupacis A (2013) Higher surgeon and hospital volume improves long-term survival after radical cystectomy. Cancer 119(19):3546–3554
Shahian DM, Normand SL (2003) The volume-outcome relationship: from Luft to Leapfrog. Ann Thorac Surg 75(3):1048–1058
Nordin P, van der Linden W (2008) Volume of procedures and risk of recurrence after repair of groin hernia: national register study. BMJ 336(7650):934–937
Borenstein SH, To T, Wajja A, Langer JC (2005) Effect of subspecialty training and volume on outcome after pediatric inguinal hernia repair. J Pediatr Surg 40(1):75–80
Aquina CT, Kelly KN, Probst CP, Iannuzzi JC, Noyes K, Langstein HN, Monson JR, Fleming FJ (2015) Surgeon volume plays a significant role in outcomes and cost following open incisional hernia repair. J Gastrointest Surg 19(1):100–110 (discussion 110)
Finan KR, Vick CC, Kiefe CI, Neumayer L, Hawn MT (2005) Predictors of wound infection in ventral hernia repair. Am J Surg 190(5):676–681
Dunne JR, Malone DL, Tracy JK, Napolitano LM (2003) Abdominal wall hernias: risk factors for infection and resource utilization. J Surg Res 111(1):78–84
Birkmeyer JD, Dimick JB (2009) Understanding and reducing variation in surgical mortality. Annu Rev Med 60:405–415
Durbin BL, Faulkner JD, Jernigan R, Hope D, Jacob B, Hope WW (2022) Patient referrals for hernia consultations through the International Hernia Collaboration (IHC) online social media platform. Am Surg 88(5):1026–1027
Jones DB, Stefanidis D, Korndorffer JR Jr, Dimick JB, Jacob BP, Schultz L, Scott DJ (2017) SAGES University MASTERS Program: a structured curriculum for deliberate, lifelong learning. Surg Endosc 31(8):3061–3071
Chen XP, Cochran A, Harzman AE, Ellison EC (2021) A novel operative coaching program for general surgery chief residents improves operative efficiency. J Surg Educ 78(4):1097–1102
Greenberg CC, Dombrowski J, Dimick JB (2016) Video-based surgical coaching: an emerging approach to performance improvement. JAMA Surg 151(3):282–283
Huynh D, Fadaee N, Gok H, Wright A, Towfigh S (2021) Thou shalt not trust online videos for inguinal hernia repair techniques. Surg Endosc 35(10):5724–5728
Cakmak G (2021) Evaluation of scientific quality of Youtube video content related to umbilical hernia. Cureus 13(4):e14675
Funding
No funding was obtained for the conduct of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Vahagn Nikolian: Reports educator and consultancy fees on behalf of Intuitive Surgical, Medtronic, and Caresyntax. Artem Shmelev, Molly Barron, Jordan Bray have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Invited Submission related to podium presentation at SAGES 2023. Montreal, Quebec.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shmelev, A., Olsen, M.A., Bray, J.O. et al. Surgeon volumes: preserving appropriate surgical outcomes in higher-risk patient populations undergoing abdominal wall reconstruction. Surg Endosc 37, 7582–7590 (2023). https://doi.org/10.1007/s00464-023-10286-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10286-5