Abstract
Background/aims
Due to the possible metachronous recurrence of gastric neoplasia, surveillance gastroscopy is mandatory after endoscopic resection for gastric neoplasia. However, there is no consensus on the surveillance gastroscopy interval. This study aimed to find an optimal interval of surveillance gastroscopy and to investigate the risk factors for metachronous gastric neoplasia.
Methods
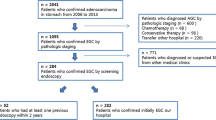
Medical records were reviewed retrospectively in patients who underwent endoscopic resection for gastric neoplasia in 3 teaching hospitals from June 2012 to July 2022. Patients were divided into two groups; annual surveillance vs. biannual surveillance. The incidence of metachronous gastric neoplasia was identified, and the risk factors for metachronous gastric neoplasia were investigated.
Results
Among the 1,533 patients who underwent endoscopic resection for gastric neoplasia, 677 patients were enrolled in this study (annual surveillance 302, biannual surveillance 375). Metachronous gastric neoplasia was observed in 61 patients (annual surveillance 26/302, biannual surveillance 32/375, P = 0.989), and metachronous gastric adenocarcinoma was observed in 26 patients (annual surveillance 13/302, biannual surveillance 13/375, P = 0.582). All the lesions were removed by endoscopic resection successfully. In a multivariate analysis, severe atrophic gastritis on gastroscopy was an independent risk factor for metachronous gastric adenocarcinoma (odds ratio 3.8, 95% confidence interval 1.4‒10.1; P = 0.008).
Conclusions
Meticulous observation to detect the metachronous gastric neoplasia is necessary for patients with severe atrophic gastritis during follow-up gastroscopy after endoscopic resection for gastric neoplasia. Annual surveillance gastroscopy might be enough after endoscopic resection for gastric neoplasia.



Similar content being viewed by others
References
Najmeh S, Cools-Lartigue J, Mueller C, Ferri LE (2016) Comparing laparoscopic to endoscopic resections for early gastric cancer in a high volume North American Center. J Gastrointest Surg 20(9):1547–1553
Kim SJ, Choi CW, Nam HS, Kang DH, Kim HW, Park SB, Ryu DG (2020) Factors associated with conversion to snare resection during gastric endoscopic submucosal dissection. Surg Endosc 34(4):1585–1591
Liu Q, Ding L, Qiu X, Meng F (2020) Updated evaluation of endoscopic submucosal dissection versus surgery for early gastric cancer: a systematic review and meta-analysis. Int J Surg 73:28–41
Nam SY, Jeon SW, Lee HS, Kwon YH, Park H, Choi JW (2017) Long-term follow-up of pepsinogen I/II ratio after eradication of Helicobacter pylori in patients who underwent endoscopic mucosal resection for gastric cancer. Dig Liver Dis 49(5):500–506
Ryu SJ, Kim BW, Kim BG, Kim JH, Kim JS, Kim JI, Park JM, Oh JH, Kim TH, Kim JJ, Park SM, Park CH, Song KY, Lee JH, Kim SG, Kim DJ, Kim W (2016) Endoscopic submucosal dissection versus surgical resection for early gastric cancer: a retrospective multicenter study on immediate and long-term outcome over 5 years. Surg Endosc 30(12):5283–5289
Abdelfatah MM, Barakat M, Ahmad D, Ibrahim M, Ahmed Y, Kurdi Y, Grimm IS, Othman MO (2019) Long-term outcomes of endoscopic submucosal dissection versus surgery in early gastric cancer: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol 31(4):418–424
Abe S, Oda I, Suzuki H, Nonaka S, Yoshinaga S, Nakajima T, Sekiguchi M, Mori G, Taniguchi H, Sekine S, Katai H, Saito Y (2015) Long-term surveillance and treatment outcomes of metachronous gastric cancer occurring after curative endoscopic submucosal dissection. Endoscopy 47(12):1113–1118
Choi MK, Kim GH, Park DY, Song GA, Kim DU, Ryu DY, Lee BE, Cheong JH, Cho M (2013) Long-term outcomes of endoscopic submucosal dissection for early gastric cancer: a single-center experience. Surg Endosc 27(11):4250–4258
Ono H, Yao K, Fujishiro M, Oda I, Uedo N, Nimura S, Yahagi N, Iishi H, Oka M, Ajioka Y, Fujimoto K (2021) Guidelines for endoscopic submucosal dissection and endoscopic mucosal resection for early gastric cancer (second edition). Dig Endosc 33(1):4–20
Park CH, Yang DH, Kim JW, Kim JH, Kim JH, Min YW, Lee SH, Bae JH, Chung H, Choi KD, Park JC, Lee H, Kwak MS, Kim B, Lee HJ, Lee HS, Choi M, Park DA, Lee JY, Byeon JS, Park CG, Cho JY, Lee ST, Chun HJ (2020) Clinical practice guideline for endoscopic resection of early gastrointestinal cancer. Clin Endosc 53(2):142–166
Japanese Gastric Cancer Association (1998) Japanese classification of gastric carcinoma—2nd English edition. Gastric Cancer 1(1):10–24
Cho CJ, Ahn JY, Jung HY, Jung K, Oh HY, Na HK, Jung KW, Lee JH, Kim DH, Choi KD, Song HJ, Lee GH, Kim JH, Kim SO (2017) The incidence and locational predilection of metachronous tumors after endoscopic resection of high-grade dysplasia and early gastric cancer. Surg Endosc 31(1):389–397
Kim YI, Park JY, Kim BJ, Hwang HW, Hong SA, Kim JG (2020) Risk of metachronous gastric neoplasm occurrence during intermediate-term follow-up period after endoscopic submucosal dissection for gastric dysplasia. Sci Rep 10(1):6747
Kimura K, Takemoto T (1969) An endoscopic recognition of the atrophic border and its significance in chronic gastritis. Endoscopy 1(3):87–97
Dixon MF, Genta RM, Yardley JH, Correa P (1996) Classification and grading of gastritis. The updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994. Am J Surg Pathol 20(10):1161–1181
Yoon H, Kim N, Shin CM, Lee HS, Kim BK, Kang GH, Kim JM, Kim JS, Lee DH, Jung HC (2016) Risk factors for metachronous gastric neoplasms in patients who underwent endoscopic resection of a gastric neoplasm. Gut Liver 10(2):228–236
Ajani JA, D’Amico TA, Bentrem DJ, Chao J, Cooke D, Corvera C, Das P, Enzinger PC, Enzler T, Fanta P, Farjah F, Gerdes H, Gibson MK, Hochwald S, Hofstetter WL, Ilson DH, Keswani RN, Kim S, Kleinberg LR, Klempner SJ, Lacy J, Ly QP, Matkowskyj KA, McNamara M, Mulcahy MF, Outlaw D, Park H, Perry KA, Pimiento J, Poultsides GA, Reznik S, Roses RE, Strong VE, Su S, Wang HL, Wiesner G, Willett CG, Yakoub D, Yoon H, McMillian N, Pluchino LA (2022) Gastric Cancer, Version 2.2022, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Cancer Netw 20(2):167–192
Shin GY, Cho HJ, Park JM, Lim CH, Cho YK, Choi MG (2020) Increased incidence of metachronous gastric neoplasm after endoscopic resection in patients with synchronous gastric neoplasm. BMC Gastroenterol 20(1):206
Park TY, Jeong SJ, Kim TH, Lee J, Park J, Kim TO, Park YE (2020) Long-term outcomes of patients with gastric adenoma in Korea: a retrospective observational study. Medicine 99(12):e19553
Nam SY, Choi IJ, Park KW, Kim CG, Lee JY, Kook MC, Lee JS, Park SR, Lee JH, Ryu KW, Kim YW (2009) Effect of repeated endoscopic screening on the incidence and treatment of gastric cacer in health screenes. Eur J Gastroenterol Hepatol 21(8):855–860
Choi IJ, Kook MC, Kim YI, Cho SJ, Lee JY, Kim CG, Park B, Nam BH (2018) Helicobacter pylori therapy for the prevention of metachronous gastric cancer. N Engl J Med 378(12):1085–1095
Nakata R, Nagami Y, Hashimoto A, Sakai T, Ominami M, Fukunaga S, Otani K, Hosomi S, Tanaka F, Ohira M, Taira K, Yamagami H, Tanigawa T, Watanabe T, Fujiwara Y (2021) Successful eradication of Helicobacter pylori could prevent metachronous gastric cancer: a propensity matching analysis. Digestion 102(2):236–245
Kim SJ, Choi CW, Kang DH, Kim HW, Park SB (2021) Comparison of biannual and annual endoscopic gastric cancer surveillance after endoscopic resection. Surg Endosc 36(3):1806–1813
Li WQ, Zhang JY, Ma JL, Li ZX, Zhang L, Zhang Y, Guo Y, Zhou T, Li JY, Shen L, Liu WD, Han ZX, Blot WJ, Gail MH, Pan KF, You WC (2019) Effects of Helicobacter pylori treatment and vitamin and garlic supplementation on gastric cancer incidence and mortality: follow-up of a randomized intervention trial. BMJ 366:l5016
Yan L, Chen Y, Chen F, Tao T, Hu Z, Wang J, You J, Wong BCY, Chen J, Ye W (2022) Effect of Helicobacter pylori eradication on gastric cancer prevention: updated report from a randomized controlled trial with 26.5 years of follow-up. Gastroenterology 163(1):154–162
Funding
None declared.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Younghee Choe, Dr. Byung-Wook Kim, Dr. Tae Ho Kim, Dr. Jun-Won Chung, Dr. Jongwon Kim, Dr. Soo-Young Na, and Dr. Joon Sung Kim have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Choe, Y., Kim, BW., Kim, T.H. et al. The optimal interval of surveillance gastroscopy after endoscopic resection for gastric neoplasia: a multicenter cohort study. Surg Endosc 37, 7556–7562 (2023). https://doi.org/10.1007/s00464-023-10259-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10259-8