Abstract
Background
Fundoplication is known to improve allograft outcomes in lung transplant recipients by reducing retrograde aspiration secondary to gastroesophageal reflux disease, a modifiable risk factor for chronic allograft dysfunction. Laparoscopic Nissen fundoplication has historically been the anti-reflux procedure of choice, but the procedure is associated with discernable rates of postoperative dysphagia and gas-bloat syndrome. Laparoscopic Toupet fundoplication, an alternate anti-reflux surgery with lower rates of foregut complications in the general population, is the procedure of choice on our institution’s lung transplant protocol. In this work, we evaluated the efficacy and safety of laparoscopic Toupet fundoplication in our lung transplant recipients.
Methods
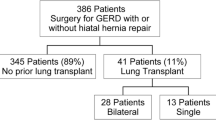
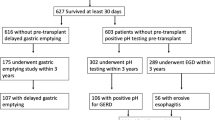
A prospective case series of 44 lung transplant recipients who underwent laparoscopic Toupet fundoplication by a single surgeon between September 2018 and November 2020 was performed. Preoperative and postoperative results from 24-h pH, esophageal manometry, gastric emptying, and pulmonary function studies were collected alongside severity of gastroesophageal reflux disease and other gastrointestinal symptoms.
Results
Median DeMeester score decreased from 25.9 to 5.4 after fundoplication (p < 0.0001), while percentage of time pH < 4 decreased from 7 to 1.1% (p < 0.0001). The severity of heartburn and regurgitation were also reduced (p < 0.0001 and p = 0.0029 respectively). Overall, pulmonary function, esophageal motility, gastric emptying, severity of bloating, and dysphagia were not significantly different post-fundoplication than pre-fundoplication. Patients with decreasing rates of FEV1 pre-fundoplication saw improvement in their rate of change of FEV1 post-fundoplication (p = 0.011). Median follow-up was 32.2 months post-fundoplication.
Conclusions
Laparoscopic Toupet fundoplication provides objective pathologic acid reflux control and symptomatic gastroesophageal reflux improvement in lung transplant recipients while preserving lung function and foregut motility. Thus, laparoscopic Toupet fundoplication is a safe and effective antireflux surgery alternative in lung transplant recipients.






Similar content being viewed by others
Abbreviations
- A1AT:
-
Alpha-1 anti-trypsin
- ARS:
-
Anti-reflux surgery
- ASA:
-
American Society of Anesthesiology
- BOS:
-
Bronchiolitis obliterans syndrome
- CLAD:
-
Chronic lung allograft dysfunction
- COPD:
-
Chronic obstructive pulmonary disease
- CF:
-
Cystic fibrosis
- CI:
-
Confidence interval
- DCI:
-
Distal contractile integral
- FEV1:
-
Forced expiratory volume in 1 s
- FVC:
-
Forced vital capacity
- GERD:
-
Gastroesophageal reflux disease
- GES:
-
Gastric emptying study
- GI:
-
Gastrointestinal
- HREM:
-
High-resolution esophageal manometry
- ILD:
-
Interstitial lung disease
- IQR:
-
Interquartile range
- IRP:
-
Integrated relaxation pressure
- ISHLT:
-
International Society for Heart and Lung Transplantation
- LARS:
-
Laparoscopic anti-reflux surgery
- LES:
-
Lower esophageal sphincter
- LESP:
-
Lower esophageal sphincter pressure
- LNF:
-
Laparoscopic Nissen fundoplication
- LTF:
-
Laparoscopic Toupet fundoplication
- LTx:
-
Lung transplant
- PFT:
-
Pulmonary function test
- PPI:
-
Proton pump inhibitor
References
Shah N, Force SD, Mitchell PO, Lin E, Lawrence EC, Easley K, Qian J, Ramirez A, Neujahr DC, Gal A, Leeper K, Pelaez A (2010) Gastroesophageal reflux disease is associated with an increased rate of acute rejection in lung transplant allografts. Transplant Proc 42:2702–2706. https://doi.org/10.1016/j.transproceed.2010.05.155
Hathorn KE, Chan WW, Lo W-K (2017) Role of gastroesophageal reflux disease in lung transplantation. World J Transplant 7:103–116. https://doi.org/10.5500/wjt.v7.i2.103
Patti MG, Vela MF, Odell DD, Richter JE, Fisichella PM, Vaezi MF (2016) The intersection of GERD, aspiration, and lung transplantation. J Laparoendosc Adv Surg Tech A 26:501–505. https://doi.org/10.1089/lap.2016.0170
Young JS, Coppolino A (2021) Esophageal disease in lung transplant patients. Ann Transl Med 9:900. https://doi.org/10.21037/atm-20-4934
Fisichella PM, Davis CS, Kovacs EJ (2012) A review of the role of GERD-induced aspiration after lung transplantation. Surg Endosc 26:1201–1204. https://doi.org/10.1007/s00464-011-2037-y
Roy SB, Elnahas S, Serrone R, Haworth C, Olson MT, Kang P, Smith MA, Bremner RM, Huang JL (2018) Early fundoplication is associated with slower decline in lung function after lung transplantation in patients with gastroesophageal reflux disease. J Thorac Cardiovasc Surg 155:2762-2771.e1. https://doi.org/10.1016/j.jtcvs.2018.02.009
Lund RJ, Wetcher GJ, Raiser F, Glaser K, Perdikis G, Gadenstätter M, Katada N, Filipi CJ, Hinder RA (1997) Laparoscopic Toupet fundoplication for gastroesophageal reflux disease with poor esophageal body motility. J Gastrointest Surg 1:301–308. https://doi.org/10.1016/s1091-255x(97)80049-2
Du X, Hu Z, Yan C, Zhang C, Wang Z, Wu J (2016) A meta-analysis of long follow-up outcomes of laparoscopic Nissen (total) versus Toupet (270°) fundoplication for gastro-esophageal reflux disease based on randomized controlled trials in adults. BMC Gastroenterol 16:88. https://doi.org/10.1186/s12876-016-0502-8
Håkanson BS, Lundell L, Bylund A, Thorell A (2019) Comparison of laparoscopic 270° posterior partial fundoplication vs total fundoplication for the treatment of gastroesophageal reflux disease: a randomized clinical trial. JAMA Surg 154:479–486. https://doi.org/10.1001/jamasurg.2019.0047
Shan C-X, Zhang W, Zheng X-M, Jiang D-Z, Liu S, Qiu M (2010) Evidence-based appraisal in laparoscopic Nissen and Toupet fundoplications for gastroesophageal reflux disease. World J Gastroenterol 16:3063–3071. https://doi.org/10.3748/wjg.v16.i24.3063
Khajanchee YS, O’Rourke RW, Lockhart B, Patterson EJ, Hansen PD, Swanstrom LL (2002) Postoperative symptoms and failure after antireflux surgery. Arch Surg 137:1008–1014. https://doi.org/10.1001/archsurg.137.9.1008
Fox MR, Sweis R, Yadlapati R, Pandolfino J, Hani A, Defilippi C, Jan T, Rommel N (2021) Chicago classification version 4.0© technical review: update on standard high-resolution manometry protocol for the assessment of esophageal motility. Neurogastroenterol Motil 33:e14120. https://doi.org/10.1111/nmo.14120
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications. Ann Surg 240:205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
R Core Team (2022) R: A language and environment for statistical computing. https://www.Rproject.org/
Wickham H, Vaughn D, Girlich M (2023) tidyr: tidy messy data. https://tidyr.tidyverse.org, https://github.com/tidyverse/tidyr.
Robertson AGN, Krishnan A, Ward C, Pearson JP, Small T, Corris PA, Dark JH, Karat D, Shenfine J, Griffin SM (2012) Anti-reflux surgery in lung transplant recipients: outcomes and effects on quality of life. Eur Respir J 39:691–697. https://doi.org/10.1183/09031936.00061811
Yodice M, Mignucci A, Shah V, Ashley C, Tadros M (2021) Preoperative physiological esophageal assessment for anti-reflux surgery: a guide for surgeons on high-resolution manometry and pH testing. World J Gastroenterol 27:1751–1769. https://doi.org/10.3748/wjg.v27.i16.1751
Castor JM, Wood RK, Muir AJ, Palmer SM, Shimpi RA (2010) Gastroesophageal reflux and altered motility in lung transplant rejection. Neurogastroenterol Motil 22:841–850. https://doi.org/10.1111/j.1365-2982.2010.01522.x
Verleden SE, Vos R, Vanaudenaerde BM, Verleden GM (2017) Chronic lung allograft dysfunction phenotypes and treatment. J Thorac Dis 9:2650–2659. https://doi.org/10.21037/jtd.2017.07.81
Hennessy SA, Hranjec T, Swenson BR, Kozower BD, Jones DR, Ailawadi G, Kron IL, Lau CL (2010) Donor factors are associated with bronchiolitis obliterans syndrome after lung transplantation. Ann Thorac Surg 89:1555–1562. https://doi.org/10.1016/j.athoracsur.2010.01.060
Analatos A, Håkanson BS, Ansorge C, Lindblad M, Lundell L, Thorell A (2022) Clinical outcomes of a laparoscopic total vs a 270° posterior partial fundoplication in chronic gastroesophageal reflux disease: a randomized clinical trial. JAMA Surg. https://doi.org/10.1001/jamasurg.2022.0805
Antonoff MB (2018) How much does early fundoplication for lung transplant recipients with gastroesophageal reflux disease truly help? Challenges in escaping the perils of retrospective review. J Thorac Cardiovasc Surg 155:2772–2773. https://doi.org/10.1016/j.jtcvs.2018.02.057
Acknowledgements
The authors would like to thank Sara H. Gray, Candice L. Rogers, and Stefanie L. Wright for their help with this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Kelly M. Herremans is funded by NHGRI T32 HG008958, but has no financial relationships with any pharmaceutical or device company. Drs. Celeste G. Yergin, Sheetal Patel, Andres Pelaez, Tiago Machuca, Alexander L. Ayzengart, and Manuel A. Amaris, MD have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yergin, C.G., Herremans, K.M., Patel, S. et al. Laparoscopic Toupet fundoplication: a safe and effective anti-reflux option in lung transplant recipients. Surg Endosc 37, 8429–8437 (2023). https://doi.org/10.1007/s00464-023-10245-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10245-0