Abstract
Background
Some studies have demonstrated the short-term recovery course for patients who underwent laparoscopic gastrectomy according to preoperative computed tomography angiography (CTA) assessment. However, reports of the long-term oncological outcomes are still limited.
Methods
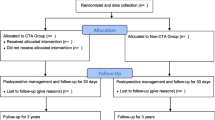
The data of 988 consecutive patients who underwent laparoscopic or robotic radical gastrectomy between January 2014 and September 2018 were analyzed retrospectively at our center, and propensity score matching was used to eliminate bias. Study cohorts were divided into the CTA group (n = 498) and the non-CTA group (n = 490) depending on whether preoperative CTA was available. The primary and secondary endpoints were the 3-year overall survival (OS) and disease-free survival (DFS) rates and the intraoperative course and short-term outcomes, respectively.
Results
431 patients were included in each group after PSM. Compared with the non-CTA group, the CTA group had more harvested lymph nodes and less operative time, blood loss, intraoperative vascular injury and total cost, especially in the subgroup analysis with BMI ≥ 25 kg/m2 patients. There was no difference in the 3 year OS and DFS between the CTA group and the non-CTA group. When further stratified by BMI < 25 or ≥ 25 kg/m2, the 3-year OS and DFS were significantly higher in the CTA group than in the non-CTA group in terms of BMI ≥ 25 kg/m2.
Conclusions
Laparoscopic or robotic radical gastrectomy based on preoperative perigastric artery CTA surgical decision-making has the possibility of improving short-term outcomes. However, there is no difference in the long-term prognosis, except for a subgroup of patients with BMI ≥ 25 kg/m2.
Graphical abstract




Similar content being viewed by others
References
Miller KD, Nogueira L, Mariotto AB, Rowland JH, Yabroff KR, Alfano CM, Jemal A, Kramer JL, Siegel RL (2019) Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin 69:363–385
Thrift AP, El-Serag HB (2020) Burden of gastric cancer. Clin Gastroenterol Hepatol 18:534–542
Hu Y, Huang C, Sun Y, Su X, Cao H, Hu J, Xue Y, Suo J, Tao K, He X, Wei H, Ying M, Hu W, Du X, Chen P, Liu H, Zheng C, Liu F, Yu J, Li Z, Zhao G, Chen X, Wang K, Li P, Xing J, Li G (2016) Morbidity and mortality of laparoscopic versus open D2 distal gastrectomy for advanced gastric cancer: a randomized controlled trial. J Clin Oncol 34:1350–1357
Yu J, Huang C, Sun Y, Su X, Cao H, Hu J, Wang K, Suo J, Tao K, He X, Wei H, Ying M, Hu W, Du X, Hu Y, Liu H, Zheng C, Li P, Xie J, Liu F, Li Z, Zhao G, Yang K, Liu C, Li H, Chen P, Ji J, Li G (2019) Effect of laparoscopic vs open distal gastrectomy on 3-year disease-free survival in patients with locally advanced gastric cancer: the class-01 randomized clinical trial. JAMA 321:1983–1992
Sunagawa H, Kinoshita T (2017) Three-dimensional computed tomography simulation for laparoscopic lymph node dissection in the treatment of proximal gastric cancer. Transl Gastroenterol Hepatol 2:54
Shen S, Cao S, Jiang H, Liu S, Liu X, Li Z, Liu D, Zhou Y (2019) The short-term outcomes of gastric cancer patients based on a proposal for a novel classification of perigastric arteries. J Gastrointest Surg. https://doi.org/10.1007/s11605-019-04427-2
Chen Y, Liu L, Wang X, Wang J, Yan Z, Cheng J, Gong G, Li G (2013) Body mass index and risk of gastric cancer: a meta-analysis of a population with more than ten million from 24 prospective studies. Cancer Epidemiol Biomark Prev 22:1395–1408
Dhar DK, Kubota H, Tachibana M, Kotoh T, Tabara H, Masunaga R, Kohno H, Nagasue N (2000) Body mass index determines the success of lymph node dissection and predicts the outcome of gastric carcinoma patients. Oncology 59:18–23
Tokunaga M, Hiki N, Fukunaga T, Ogura T, Miyata S, Yamaguchi T (2009) Effect of individual fat areas on early surgical outcomes after open gastrectomy for gastric cancer. J British Surg 96:496–500
Liu H, Wang F, Liu B, Zheng Z, Zhao J, Zhang J (2021) Application of three-dimensional reconstruction with a Hisense computer-assisted system in upper pancreatic lymph node dissection during laparoscopic-assisted radical gastrectomy. Asian J Surg. https://doi.org/10.1016/j.asjsur.2020.12.034
Surgery B (2016) Robotic and laparoscopic surgery Committee of Chin: Guideline for laparoscopic gastrectomy for gastric cancer (2016 edition). Chinese Journal of Digestive Surgery 15:851–857
Japanese Gastric Cancer A (2011) Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 14:113–123
Zhang X, Tanigawa N (2009) Learning curve of laparoscopic surgery for gastric cancer, a laparoscopic distal gastrectomy-based analysis. Surg Endosc 23:1259–1264
Kang BH, Xuan Y, Hur H, Ahn CW, Cho YK, Han S-U (2012) Comparison of surgical outcomes between robotic and laparoscopic gastrectomy for gastric cancer: the learning curve of robotic surgery. J Gastric Cancer 12:156–163
jp JGCAjkk-ma, (2011) Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 14:113–123
Dindo D, Demartines N, Clavien P-A (2004) Classification of surgical complications. Ann Surg 240:205–213
Wang FH, Zhang XT, Li YF, Tang L, Qu XJ, Ying JE, Zhang J, Sun LY, Lin RB, Qiu H, Wang C, Qiu MZ, Cai MY, Wu Q, Liu H, Guan WL, Zhou AP, Zhang YJ, Liu TS, Bi F, Yuan XL, Rao SX, Xin Y, Sheng WQ, Xu HM, Li GX, Ji JF, Zhou ZW, Liang H, Zhang YQ, Jin J, Shen L, Li J, Xu RH (2021) The Chinese Society of Clinical Oncology (CSCO): Clinical guidelines for the diagnosis and treatment of gastric cancer, 2021. Cancer Commun (Lond). https://doi.org/10.1002/cac2.12193
Egner JR (2010) AJCC cancer staging manual. Jama 304:1726–1727
Choi S, Song JH, Lee S, Cho M, Kim YM, Kim HI, Hyung WJ (2022) Trends in clinical outcomes and long-term survival after robotic gastrectomy for gastric cancer: a single high-volume center experience of consecutive 2000 patients. Gastric Cancer 25:275–286
Nakagawa M, Kojima K, Inokuchi M, Kato K, Sugita H, Kawano T, Sugihara K (2014) Patterns, timing and risk factors of recurrence of gastric cancer after laparoscopic gastrectomy: reliable results following long-term follow-up. Eur J Surg Oncol (EJSO) 40:1376–1382
Michels NA (1966) Newer anatomy of the liver and its variant blood supply and collateral circulation. Am J Surg 112:337–347
Hiatt JR, Gabbay J, Busuttil RW (1994) Surgical anatomy of the hepatic arteries in 1000 cases. Ann Surg 220:50
Lipshutz B (1917) A composite study of the coeliac axis artery. Ann Surg 65:159
López-Andújar R, Moya A, Montalvá E, Berenguer M, De Juan M, San Juan F, Pareja E, Vila JJ, Orbis F, Prieto M (2007) Lessons learned from anatomic variants of the hepatic artery in 1081 transplanted livers. Liver Transpl 13:1401–1404
Song S-Y, Chung JW, Yin YH, Jae HJ, Kim H-C, Jeon UB, Cho BH, So YH, Park JH (2010) Celiac axis and common hepatic artery variations in 5002 patients: systematic analysis with spiral CT and DSA. Radiology 255:278–288
Kozhevnikova T (1977) Age and individual characteristics in the structure of the celiac trunk in man. Arkhiv Anatomii, Gistologii i Embriologii 72:19–25
Silveira LAd, Silveira FBC, Fazan VPS (2009) Arterial diameter of the celiac trunk and its branches: anatomical study. Acta cirurgica brasileira 24:43–47
Oki E, Sakaguchi Y, Hiroshige S, Kusumoto T, Kakeji Y, Maehara Y (2011) Preservation of an aberrant hepatic artery arising from the left gastric artery during laparoscopic gastrectomy for gastric cancer. J Am Coll Surg 212:e25–e27
Gao Y, Hu J, Zhang X, Zhang M, Wang D, Zheng X, Liu S, Lu Y (2019) Use of hisense computer-assisted surgery system enhances infrapyloric lymph node dissection for gastric cancer. J Surg Res 242:31–39
Natsume T, Shuto K, Yanagawa N, Akai T, Kawahira H, Hayashi H, Matsubara H (2011) The classification of anatomic variations in the perigastric vessels by dual-phase CT to reduce intraoperative bleeding during laparoscopic gastrectomy. Surg Endosc 25:1420–1424
Willard C-D, Kjaestad E, Stimec BV, Edwin B, Ignjatovic D, Oresland T, Bakka AO, Reiertsen O, Færden AE, Thorsen Y, Andersen SN, Negaard A, Dicko A, Pfeffer F, Forsmo H, Ytre-Hauge S, Nesgaard JM, Jacobsen R, von Brandis KML, Suhrke P, Luzon J, Sevinç B, Andersen BT, Gaupset R, Bergamaschi R, Pullig F, Baral J, Ruiz MG, Lindstrøm J, Sheikh AE, Strommen T, Group RCCS (2019) Preoperative anatomical road mapping reduces variability of operating time, estimated blood loss, and lymph node yield in right colectomy with extended D3 mesenterectomy for cancer. Int J Colorectal Dis 34:151–160
Winston CB, Lee NA, Jarnagin WR, Teitcher J, DeMatteo RP, Fong Y, Blumgart LH (2007) CT angiography for delineation of celiac and superior mesenteric artery variants in patients undergoing hepatobiliary and pancreatic surgery. AJR Am J Roentgenol 189:W13-19
Lee S-W, Shinohara H, Matsuki M, Okuda J, Nomura E, Mabuchi H, Nishiguchi K, Takaori K, Narabayashi I, Tanigawa N (2003) Preoperative simulation of vascular anatomy by three-dimensional computed tomography imaging in laparoscopic gastric cancer surgery. J Am Coll Surg 197:927–936
Kulig J, Sierzega M, Kolodziejczyk P, Dadan J, Drews M, Fraczek M, Jeziorski A, Krawczyk M, Starzynska T, Wallner G (2010) Implications of overweight in gastric cancer: a multicenter study in a Western patient population. Eur J Surg Oncol (EJSO) 36:969–976
Lee JH, Paik YH, Lee JS, Ryu KW, Kim CG, Park SR, Kim YW, Kook MC, Nam B-h, Bae J-M (2007) Abdominal shape of gastric cancer patients influences short-term surgical outcomes. Ann Surg Oncol 14:1288–1294
Wu XS, Wu WG, Li ML, Yang JH, Ding QC, Zhang L, Mu JS, Gu J, Dong P, Lu JH, Liu YB (2013) Impact of being overweight on the surgical outcomes of patients with gastric cancer: a meta-analysis. World J Gastroenterol 19:4596–4606
Romero FR, Rais-Bahrami S, Muntener M, Brito FAR, Jarrett TW, Kavoussi LR (2008) Laparoscopic partial nephrectomy in obese and non-obese patients: comparison with open surgery. Urology 71:806–809
Williams TK, Rosato EL, Kennedy EP, Chojnacki KA, Andrel J, Hyslop T, Doria C, Sauter PK, Bloom J, Yeo CJ, Berger AC (2009) Impact of obesity on perioperative morbidity and mortality after pancreaticoduodenectomy. J Am Coll Surg 208:210–217
Kodera Y, Ito S, Yamamura Y, Mochizuki Y, Fujiwara M, Hibi K, Ito K, Akiyama S, Nakao A (2004) Obesity and outcome of distal gastrectomy with D2 lymphadenectomy for carcinoma. Hepatogastroenterology 51:1225–1228
Jiang J, Teng Y, Fan Z, Khan S, Xia Y (2014) Does obesity affect the surgical outcome and complication rates of spinal surgery? A meta-analysis. Clin Orthop Relat Res 472:968–975
Meng C, Cao S, Liu X, Li L, He Q, Xia L, Jiang L, Chu X, Wang X, Wang H, Hui X, Sun Z, Huang S, Duan Q, Yang D, Zhang H, Tian Y, Li Z, Zhou Y (2021) Effect of preoperative CT angiography examination on the clinical outcome of patients with BMI >/= 25.0 kg/m2 undergoing laparoscopic gastrectomy: study protocol for a multicentre randomized controlled trial. Trials 22:912
Acknowledgements
We would like to thank the participants for their contributions to this study.
Funding
This study was funded by Shandong Provincial Natural Science Foundation, China (Grant No. ZR202103040182); the National Natural Science Youth Foundation of China (Grant No. 82103577).
Author information
Authors and Affiliations
Contributions
YZ and CM: conceived and designed the study; CM: drafted the manuscript; SC, YT, SS, XL, ZL, YK, and XW: completed data acquisition, data management and statistical analysis; YL, YS, JX, XZ, HY, HZ, ZJ: revised manuscript critically for important intellectual content; DZ: provided great technical assistance throughout the experiment's design and data processing; All authors contributed to this article and approved the submitted version.
Corresponding author
Ethics declarations
Disclosures
Cheng Meng, Shougen Cao, Yulong Tian, Shuai Shen, Xiaodong Liu, Zequn Li, Yu Li, Yuqi Sun, Jianfei Xu, Xingqi Zhang, Ying Kong, Xujie Wang, Hao Yang, Hao Zhong, Zhuoyu Jia, Dongfeng Zhang, Yanbing Zhou have no conflicts of interest or financial ties to disclose.
Ethical approval
This study was approved by the Affiliated Hospital of Qingdao University ethics review committee (Approval Number QYFYWZLL-26829). All procedures have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This study was accepted as poster session at the 15th International Gastric Cancer Congress (IGCC 2023), from June 14 to 17, 2023 in Yokohama, Japan.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Meng, C., Cao, S., Tian, Y. et al. Short- and long-term outcomes of laparoscopic or robotic radical gastrectomy based on preoperative perigastric artery CTA surgical decision-making: a high-volume center retrospective study with propensity score matching. Surg Endosc 37, 6930–6942 (2023). https://doi.org/10.1007/s00464-023-10170-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10170-2