Abstract
Background
Debate exists regarding the most appropriate type of mesh to use in ventral hernia repair (VHR). Meshes are broadly categorized as synthetic or biologic, each mesh with individual advantages and disadvantages. More recently developed biosynthetic mesh has characteristics of both mesh types. The current study aims to examine long-term follow-up data and directly compare outcomes—specifically hernia recurrence—of VHR with biosynthetic versus synthetic mesh.
Methods
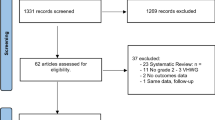
With IRB approval, consecutive cases of VHR (CPT codes 49,560, 49,561, 49,565, and 49,566 with 49,568) performed between 2013 and 2018 at a single institution were reviewed. Local NSQIP data was utilized for patient demographics, perioperative characteristics, CDC Wound Class, comorbidities, and mesh type. A review of electronic medical records provided additional variables including hernia defect size, postoperative wound events to six months, duration of follow-up, and incidence of hernia recurrence. Longevity of repair was measured using Kaplan–Meier method and adjusted Cox proportional hazards regression.
Results
Biosynthetic mesh was used in 101 patients (23%) and synthetic mesh in 338 (77%). On average, patients repaired using biosynthetic mesh were older than those with synthetic mesh (57 vs. 52 years; p = .008). Also, ASA Class ≥ III was more common in biosynthetic mesh cases (70.3% vs. 55.1%; p = .016). Patients repaired with biosynthetic mesh were more likely than patients with synthetic mesh to have had a prior abdominal infection (30.7% vs. 19.8%; p = .029). Using a Kaplan–Meier analysis, there was not a significant difference in hernia recurrence between the two mesh types, with both types having Kaplan Meir 5-year recurrence-free survival rates of about 72%.
Conclusion
Using Kaplan–Meier analysis, synthetic mesh and biosynthetic mesh result in comparable hernia recurrence rates and surgical site infection rates in abdominal wall reconstruction patients with follow-up to as long as five years.

Similar content being viewed by others
References
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240:578–583
Totten CF, Davenport DL, Ward ND, Roth JS (2016) Cost of ventral hernia repair using biologic or synthetic mesh. J Surg Res 203:459–465
Harris HW, Primus F, Young C, Carter JT, Lin M, Mukhtar RA, Yeh B, Allen IE, Freise C, Kim E, Sbitany H, Young DM, Hansen S (2021) Preventing recurrence in clean and contaminated hernias using biologic versus synthetic mesh in ventral hernia repair: the PRICE randomized clinical trial. Ann Surg 273:648–655
Beale EW, Hoxworth RE, Livingston EH, Trussler AP (2012) The role of biologic mesh in abdominal wall reconstruction: a systematic review of the current literature. Am J Surg 204:510–517. https://doi.org/10.1016/j.amjsurg.2012.03.009. (PMID: 23010617)
Darehzereshki A, Goldfarb M, Zehetner J, Moazzez A, Lipham JC, Mason RJ, Katkhouda N (2014) Biologic versus nonbiologic mesh in ventral hernia repair: a systematic review and meta-analysis. World J Surg 38:40–50
Kissane NA, Itani KM (2012) A decade of ventral hernia repairs with biologic acellular dermal matrix: what have we learned? Plast Recon Surg 130:194–202
Rosen MJ, Krpata DM, Ermlich B, Blatnik JA (2013) A 5-year clinical experience with single-staged repairs of infected or contaminated abdominal wall defects utilizing biologic mesh. Ann Surg 147:991–996
Martin DP, Badhwar A, Shah DV, Rizk S, Eldridge SN, Gagne DH, Ganatra A, Darois RE, Williams SF, Tai HC, Scott JR (2013) Characterization of poly-4-hydroxybutyrate mesh for hernia repair applications. J Surg Res 184:766–773
Rosen MJ, Bauer JJ, Harmaty M, Carbonell AM, Cobb WS, Matthews B, Goldblatt MI, Selzer DJ, Poulose BK, Hansson BM, Rosman C, Chao JJ, Jacobsen GR (2017) Prospective, longitudinal study of the recurrence, surgical site infection, and quality of life after contaminated ventral hernia repair using biosynthetic absorbable mesh: the COBRA study. Ann Surg 265:205–211
Miserez M, Jairam AP, Boersema GSA, Bayon Y, Jeekel J, Lange JF (2019) Resorbable synthetic meshes for abdominal wall defects in preclinical setting: a literature review. J Surg Res 237:67–75. https://doi.org/10.1016/j.jss.2018.11.054. (Epub 2019 Jan 30 PMID: 30710881)
Robinson TN, Clarke JH, Schoen J, Walsh MD (2005) Major mesh-related complications following hernia repair: events reported to the Food and Drug Administration. Surg Endosc 19:1556–1560. https://doi.org/10.1007/s00464-005-0120-y
Köckerling F, Alam NN, Antoniou SA, Daniels IR, Famiglietti F, Fortelny RH, Heiss MM, Kallinowski F, Kyle-Leinhase I, Mayer F, Miserez M, Montgomery A, Morales-Conde S, Muysoms F, Narang SK, Petter-Puchner A, Reinpold W, Scheuerlein H, Smietanski M, Stechemesser B, Strey C, Woeste G, Smart NJ (2018) What is the evidence for the use of biologic or biosynthetic meshes in abdominal wall reconstruction? Hernia 22:249–269. https://doi.org/10.1007/s10029-018-1735-y
FitzGerald JF, Kumar AS (2014) Biologic versus synthetic mesh in reinforcement: what are the pros and cons? Clin Colon Rectal Surg 27:140–148. https://doi.org/10.1055/s-0034-1394155
Mellia JA, Othman S, Naga HI, Messa CA 4th, Elfanagely O, Byrnes YM, Basta MN, Fischer JP (2020) Outcomes of poly-4-hydroxybutyrate mesh in ventral hernia repair: a systematic review and pooled analysis. Plas Reconstr Surg Glob Open 8:e3158
Sahoo S, Haskins IN, Huang LC, Krpata DM, Derwin KA, Poulose BK, Rosen MJ (2017) Early wound morbidity after open ventral hernia repair with biosynthetic or polypropylene mesh. J Am Coll Surg 225:472–480. https://doi.org/10.1016/j.jamcollsurg.2017.07.1067
Petersen K, Morrison J, Oprea V, Grischkan D, Koch A, Lorenz R, Bendavid R, Iakovlev V (2021) Necessary duration of follow-up to assess complications of mesh in hernia surgery: a time-lapse study based on 460 explants. Hernia 25:1239–1251. https://doi.org/10.1007/s10029-020-02297-1. (Epub 2020 Sep 22)
Zolin SJ, Krpata DM, Petro CC, Prabhu AS, Rosen SH, Thompson RD, Fafaj A, Thomas JD, Li-C H, Rosen MJ (2021) No winning in the battle of the bulge: Hernia recurrence after abdominal wall reconstruction. J Am Coll Surg 233:S96. https://doi.org/10.1016/j.jamcollsurg.2021.07.180
Nardi M Jr, Millo P, Brachet Contul R, Lorusso R, Usai A, Grivon M, Persico F, Ponte E, Bocchia P, Razzi S (2017) Laparoscopic ventral hernia repair with composite mesh: analysis of risk factors for recurrence in 185 patients with 5-years follow-up. Int J Surg 40:38–44
Keogh K, Slater K (2020) Comparison of biosynthetic versus synthetic mesh in clean and contaminated ventral hernia repairs. ANZ J Surg 90:542–546
Mercoli H, Tzedakis S, D’Ursol A, Nedelcu M, Memeo R, Meyer N, Vix M, Perretta S, Mutter D (2016) Postoperative complications as an independent risk factor for recurrence after laparoscopic ventral hernia repair: a prospective study of 417 patients with long-term follow-up. Surg Endosc 31:1469–1477
Finan KR, Vick CC, Kiefe CI, Neumayer L, Hawn MT (2005) Predictors of wound infection in ventral hernia repair. Am J Surg 190:676–681
Nguyen PT, Asarias JR, Pierce LM (2012) Influence of a new monofilament polyester mesh on inflammation and matrix remodeling. J Invest Surg 25:330–339
Bryan N, Ahswin H, Smart NJ, Bayon Y, Hunt JA (2012) In vitro activation of human leukocytes in response to contact with synthetic hernia meshes. Clin Biochem 45:672–676
Aydinuraz K, Ağalar C, Ağalar F, Ceken S, Duruyürek N, Vural T (2009) In vitro S. epidermidis and S. aureus adherence to composite and lightweight polypropylene grafts. J Surg Res 157:e79-86
Klinge U, Junge K, Spellerberg B, Piroth C, Klosterhalfen B, Schumpelick V (2002) Do multifilament alloplastic meshes increase the infection rate? Analysis of the polymeric surface, the bacteria adherence, and the in vivo consequences in a rat model. J Biomed Mater Res 63:765–771
Martin DP, Williams SF (2016) Medical applications of poly-4-hydroxybutyrate: a strong flexible absorbable biomaterial. Biochem Eng J 16:97–105
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. John S. Roth has the following to disclose: Grants from Beckton Dickinson & Company, Gore, and Advanced Medical Solutions (paid to institution); consulting for Beckton Dickinson & Company, Medtronic, and Abbvie. Mr. Benjamin G. Morrison, Mr. Kiah Gledhill, and Drs. Margaret A. Plymale and Daniel L. Davenport have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This manuscript was presented as an ePOSTER PRESENTATION at the 2021 SAGES Annual Meeting in Las Vegas, Nevada.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Morrison, B.G., Gledhill, K., Plymale, M.A. et al. Comparative long-term effectiveness between ventral hernia repairs with biosynthetic and synthetic mesh. Surg Endosc 37, 6044–6050 (2023). https://doi.org/10.1007/s00464-023-10082-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10082-1