Abstract
Introduction
Minimally invasive liver resection (MILR) is widely recognized as a safe and beneficial procedure in the treatment of both malignant and benign liver diseases. Hepatolithiasis has traditionally been reported to be endemic only in East Asia, but has seen a worldwide uptrend in recent decades with increasingly frequent and invasive endoscopic instrumentation of the biliary tract for a myriad of conditions. To date, there has been a woeful lack of high-quality evidence comparing the laparoscopic (LLR) and robotic (RLR) approaches to treatment hepatolithiasis.
Methods
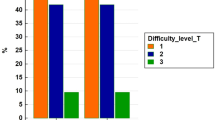
This is an international multicenter retrospective analysis of 273 patients who underwent RLR or LRR for hepatolithiasis at 33 centers in 2003–2020. The baseline clinicopathological characteristics and perioperative outcomes of these patients were assessed. To minimize selection bias, 1:1 (48 and 48 cases of RLR and LLR, respectively) and 1:2 (37 and 74 cases of RLR and LLR, respectively) propensity score matching (PSM) was performed.
Results
In the unmatched cohort, 63 (23.1%) patients underwent RLR, and 210 (76.9%) patients underwent LLR. Patient clinicopathological characteristics were comparable between the groups after PSM. After 1:1 and 1:2 PSM, RLR was associated with less blood loss (p = 0.003 in 1:2 PSM; p = 0.005 in 1:1 PSM), less patients with blood loss greater than 300 ml (p = 0.024 in 1:2 PSM; p = 0.027 in 1:1 PSM), and lower conversion rate to open surgery (p = 0.003 in 1:2 PSM; p < 0.001 in 1:1 PSM). There was no significant difference between RLR and LLR in use of the Pringle maneuver, median Pringle maneuver duration, 30-day readmission rate, postoperative morbidity, major morbidity, reoperation, and mortality.
Conclusion
Both RLR and LLR were safe and feasible for hepatolithiasis. RLR was associated with significantly less blood loss and lower open conversion rate.
Similar content being viewed by others
References
Lorio E et al (2020) Management of Hepatolithiasis: Review of the Literature. Curr Gastroenterol Rep 22(6):30
Lee SE et al (2008) Selection of appropriate liver resection in left hepatolithiasis based on anatomic and clinical study. World J Surg 32(3):413–418
Nakayama F, Koga A (1984) Hepatolithiasis: present status. World J Surg 8(1):9–14
Nakayama F et al (1991) Hepatolithiasis in East Asia: comparison between Japan and China. J Gastroenterol Hepatol 6(2):155–158
Lindström CG (1977) Frequency of gallstone disease in a well-defined Swedish population. A prospective necropsy study in Malmö. Scand J Gastroenterol 12(3):341–346
Pitt HA et al (1994) Intrahepatic stones. The transhepatic team approach. Ann Surg 219(5):527–535 (discussion 535–7)
Schmidt SC et al (2002) Right hepatic lobectomy for recurrent cholangitis after combined bile duct and right hepatic artery injury during laparoscopic cholecystectomy: a report of two cases. Langenbecks Arch Surg 387(3–4):183–187
Li H et al (2017) Laparoscopic VS open hepatectomy for hepatolithiasis: an updated systematic review and meta-analysis. World J Gastroenterol 23(43):7791–7806
Reich H et al (1991) Laparoscopic excision of benign liver lesions. Obstet Gynecol 78(5 Pt 2):956–958
Wakabayashi G, Cherqui D, Geller DA et al (2015) Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 261:619–629
Liu X et al (2018) Laparoscopic hepatectomy produces better outcomes for hepatolithiasis than open hepatectomy: an updated systematic review and meta-analysis. Int J Surg 51:151–163
Tomulescu V et al (2009) First year experience of robotic-assisted laparoscopic surgery with 153 cases in a general surgery department: indications, technique and results. Chirurgia (Bucur) 104(2):141–150
Simillis C et al (2007) Laparoscopic versus open hepatic resections for benign and malignant neoplasms–a meta-analysis. Surgery 141(2):203–211
Morel P et al (2017) Robotic versus open liver resections: a case-matched comparison. Int J Med Robot 13(3):e1800
Troisi RI et al (2013) Robot assistance in liver surgery: a real advantage over a fully laparoscopic approach? Results of a comparative bi-institutional analysis. Int J Med Robot 9(2):160–166
Shu J et al (2019) Robotic-assisted laparoscopic surgery for complex hepatolithiasis: a propensity score matching analysis. Surg Endosc 33(8):2539–2547
Lee KF et al (2016) Robotic liver resection for primary hepatolithiasis: is it beneficial? World J Surg 40(10):2490–2496
Belghiti J, Clavien PA, Gadzijev TB et al (2000) Terminology of liver anatomy and resections. HPB 2000(2):333–339
Clavien PA et al (2009) The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196
Rahbari NN et al (2011) Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery 149(5):713–724
Chen PD et al (2017) Robotic versus open hepatectomy for hepatocellular carcinoma: a matched comparison. Ann Surg Oncol 24(4):1021–1028
Tanaka S et al (2019) Validation of index-based IWATE criteria as an improved difficulty scoring system for laparoscopic liver resection. Surgery 165(4):731–740
Goh BKP et al (2021) Validation and comparison of the Iwate, IMM, Southampton and Hasegawa difficulty scoring systems for primary laparoscopic hepatectomies. HPB (Oxford) 23(5):770–776
Wakabayashi G (2016) What has changed after the Morioka consensus conference 2014 on laparoscopic liver resection? HBSN 5:281–2819
Tsung A et al (2014) Robotic versus laparoscopic hepatectomy: a matched comparison. Ann Surg 259(3):549–555
Croner RS et al (2016) Robotic liver surgery for minor hepatic resections: a comparison with laparoscopic and open standard procedures. Langenbecks Arch Surg 401(5):707–714
Kamarajah SK et al (2021) Robotic versus conventional laparoscopic liver resections: a systematic review and meta-analysis. Scand J Surg 110(3):290–300
Goh BKP et al (2019) Initial experience with robotic hepatectomy in Singapore: analysis of 48 resections in 43 consecutive patients. ANZ J Surg 89(3):201–205
Ho CM et al (2013) Systematic review of robotic liver resection. Surg Endosc 27(3):732–739
Sucandy I et al (2020) Robotic hepatectomy for benign and malignant liver tumors. J Robot Surg 14(1):75–80
Beard RE et al (2020) Long-term and oncologic outcomes of robotic versus laparoscopic liver resection for metastatic colorectal cancer: a multicenter, propensity score matching analysis. World J Surg 44(3):887–895
Wang ZZ et al (2019) Robotic vs laparoscopic hemihepatectomy: a comparative study from a single center. J Surg Oncol 120(4):646–653
Fagenson AM et al (2021) Minimally invasive hepatectomy in North America: laparoscopic versus robotic. J Gastrointest Surg 25(1):85–93
Goh BKP et al (2018) Changing trends and outcomes associated with the adoption of minimally invasive hepatectomy: a contemporary single-institution experience with 400 consecutive resections. Surg Endosc 32(11):4658–4665
Cheung TT et al (2018) The Asia Pacific Consensus Statement on laparoscopic liver resection for hepatocellular carcinoma: a report from the 7th Asia-Pacific Primary Liver Cancer Expert Meeting Held in Hong Kong. Liver Cancer 7(1):28–39
Luo LX, Yu ZY, Bai YN (2014) Laparoscopic hepatectomy for liver metastases from colorectal cancer: a meta-analysis. J Laparoendosc Adv Surg Tech A 24(4):213–222
Goh EL, Chidambaram S, Ma S (2018) Laparoscopic vs open hepatectomy for hepatocellular carcinoma in patients with cirrhosis: a meta-analysis of the long-term survival outcomes. Int J Surg 50:35–42
Yang HY et al (2021) Robotic major liver resections: surgical outcomes compared with open major liver resections. Ann Hepatobiliary Pancreat Surg 25(1):8–17
Lee KF et al (2021) Robotic versus open hemihepatectomy: a propensity score-matched study. Surg Endosc 35(5):2316–2323
Guan R et al (2019) Clinical efficacy of robot-assisted versus laparoscopic liver resection: a meta analysis. Asian J Surg 42(1):19–31
Hu L et al (2018) Effectiveness and safety of robotic-assisted versus laparoscopic hepatectomy for liver neoplasms: a meta-analysis of retrospective studies. Asian J Surg 41(5):401–416
Hu Y et al (2021) Robotic versus laparoscopic hepatectomy for malignancy: a systematic review and meta-analysis. Asian J Surg 44(4):615–628
Chong CC, Fuks D, Lee KF et al (2022) Propensity score-matched analysis comparing robotic and laparoscopic right and extended right hepatectomy. JAMA Surg 157:e220161
Yang HY, Choi GH, Chin KM et al (2022) Robotic and laparoscopic right anterior sectionectomy and central hepatectomy: multicentre propensity score-matched analysis. Br J Surg 109:311–314
Chiow AK, Fuks D, Choi GH et al (2021) International multicentre propensity score-matched analysis comparing robotic versus laparoscopic right posterior sectionectomy. Br J Surg 108:1513–1520
Chong CCN, Lok HT, Fung AKY et al (2020) Robotic versus laparoscopic hepatectomy: application of the difficulty scoring system. Surg Endosc 34:2000–2006
Fruscione M, Pickens R, Baker EH et al (2019) Robotic-assisted versus laparoscopic major liver resection: analysis of outcomes from a single center. HPB (Oxford) 21:906–911
Ciria R, Berardi G, Alconchel F et al (2020) The impact of robotics in liver surgery: a worldwide systematic review and short-term outcomes meta-analysis on 2728 cases. J Hepatobiliary Pancreat Sci 29:181–197
Stiles ZE, Behrman SW, Glazer ES et al (2017) Predictors and implications of unplanned conversion during minimally invasive hepatectomy: an analysis of the ACS-NSQIP database. HPB (Oxford) 19:957–965
Li C, Wen T (2017) Surgical management of hepatolithiasis: a minireview. Intractable Rare Dis Res 6(2):102–105
Jin RA et al (2016) Total laparoscopic left hepatectomy for primary hepatolithiasis: eight-year experience in a single center. Surgery 159(3):834–841
Aziz H et al (2021) Hospitalization costs and outcomes of open, laparoscopic, and robotic liver resections. Am Surg 88:31348211011063
Daskalaki D et al (2017) Financial impact of the robotic approach in liver surgery: a comparative study of clinical outcomes and costs between the robotic and open technique in a single institution. J Laparoendosc Adv Surg Tech A 27(4):375–382
Acknowledgements
International robotic and laparoscopic liver resection study group investigators: Chung-Yip Chan (Department of Hepatopancreatobiliary and Transplant Surgery, Singapore General Hospital/ National Cancer Centre Singapore, Singapore); Juul Meurs (Department of Digestive and Hepatobiliary/Pancreatic Surgery, Groeninge Hospital, Kortrijk, Belgium); Celine De Meyere (Department of Digestive and Hepatobiliary/Pancreatic Surgery, Groeninge Hospital, Kortrijk, Belgium); Eric C. H. Lai (Department of Surgery, Pamela Youde Nethersole Eastern Hospital, Hong Kong SAR, China); Felix Krenzien (Department of Surgery, Campus Charité Mitte and Campus Virchow-Klinikum, Charité-Universitätsmedizin, Corporate Member of Freie Universität Berlin, and Berlin Institute of Health, Berlin, Germany); Moritz Schmelzle (Department of Surgery, Campus Charité Mitte and Campus Virchow-Klinikum, Charité-Universitätsmedizin, Corporate Member of Freie Universität Berlin, and Berlin Institute of Health, Berlin, Germany); Prashant Kadam (Department of Hepatopancreatobiliary and Liver Transplant Surgery, University Hospitals Birmingham NHS Foundation Trust, Birmingham, United Kingdom); Roberto Montalti (Department of Clinical Medicine and Surgery, Division of HPB, Minimally Invasive and Robotic Surgery, Federico II University Hospital Naples, Naples, Italy); Mariano Giglio (Department of Clinical Medicine and Surgery, Division of HPB, Minimally Invasive and Robotic Surgery, Federico II University Hospital Naples, Naples, Italy); Kit-Fai Lee (Division of Hepatobiliary and Pancreatic Surgery, Department of Surgery, Prince of Wales Hospital, The Chinese University of Hong Kong, New Territories, Hong Kong SAR, China); Diana Salimgereeva (Department of Hepato-Pancreato-Biliary Surgery, Moscow Clinical Scientific Center, Moscow, Russia); Ruslan Alikhanov (Department of Hepato-Pancreato-Biliary Surgery, Moscow Clinical Scientific Center, Moscow, Russia); Lip Seng Lee (Hepatopancreatobiliary Unit, Department of Surgery, Changi General Hospital, Singapore); Mikel Gastaca (Hepatobiliary Surgery and Liver Transplantation Unit, Biocruces Bizkaia Health Research Institute, Cruces University Hospital, University of the Basque Country, Bilbao, Spain); Jae Young Jang (Department of General Surgery, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea); Chetana Lim (Department of Digestive, HBP and Liver Transplantation, Hopital Pitie-Salpetriere, Sorbonne Universite, Paris, France; Phan Phuoc Nghia (HPB Surgery Department, University Medical Center, Ho Chi Minh City); Masayuki Kojima (Department of Surgery, Fujita Health University School of Medicine, Aichi, Japan); Yutaro Kato (Department of Surgery, Fujita Health University School of Medicine, Aichi, Japan); Mansour Saleh (Department of Hepatobiliary Surgery, Assistance Publique Hopitaux de Paris, Centre Hepato-Biliaire, Paul-Brousse Hospital, Villejuif, France); Franco Pascual (Department of Hepatobiliary Surgery, Assistance Publique Hopitaux de Paris, Centre Hepato-Biliaire, Paul-Brousse Hospital, Villejuif, France); Fabricio Ferreira Coelho (Liver Surgery Unit, Department of Gastroenterology, University of Sao Paulo School of Medicine, Sao Paulo, Brazil); Jaime Arthur Pirola Kruger (Liver Surgery Unit, Department of Gastroenterology, University of Sao Paulo School of Medicine, Sao Paulo, Brazil); Astmund Avdem Fretland (The Intervention Centre and Department of HPB Surgery, Oslo University Hospital, Oslo University, Oslo, Norway); Jacob Ghotbi (The Intervention Centre and Department of HPB Surgery, Oslo University Hospital, Oslo University, Oslo, Norway); Bernardo Dalla Valle (General and Hepatobiliary Surgery, Department of Surgery, Dentistry, Gynecology and Pediatrics, University of Verona, GB Rossi Hospital, Verona, Italy); Yoelimar Guzmán (General & Digestive Surgery, Hospital Clínic, Barcelona, Spain)
Funding
Dr T. P. Kingham was partially supported by the US National Cancer Institute MSKCC Core Grant number P30 CA008747 for this study.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Disclosures
Dr Goh BK has received travel grants and honorarium from Johnson & Johnson, Olympus and Transmedic, the local distributor for the Da Vinci Robot. Dr Marino MV is a consultant for CAVA Robotics LLC. Johann Pratschke reports receiving a research grant from Intuitive Surgical Deutschland GmbH and personal fees or non-financial support from Johnson & Johnson, Medtronic, AFS Medical, Astellas, CHG Meridian, Chiesi, Falk Foundation, La Fource Group, Merck, Neovii, NOGGO, Peterson, and Promedicis. Moritz Schmelzle reports receiving personal fees or other support outside of the submitted work from Merck, Bayer, ERBE, Amgen, Johnson & Johnson, Takeda, Olympus, and Medtronic. Asmund Fretland reports receiving speaker fees from Bayer. Bong Jun Kwak, Jae Hoon Lee, Ken-Min Chin, Nicholas L. Syn, Sung Hoon Choi, Tan-To Cheung, Adrian K. H. Chiow, Iswanto Sucandy, Mikel Prieto, Charing C. Chong, Gi-Hong Choi, Mikhail Efanov, T. Peter Kingham, Robert P. Sutcliffe, Roberto I. Troisi, Xiaoying Wang, Mathieu D’Hondt, Chung Ngai Tang, Kohei Mishima, Go Wakabayashi, Daniel Cherqui, Davit L. Aghayan, Bjorn Edwin, Olivier Scatton, Atsushi Sugioka, Tran Cong Duy Long, Constantino Fondevila, Mohammad Alzoubi, Mohammad Abu Hilal, Andrea Ruzzenente, Alessandro Ferrero, Paulo Herman, Boram Lee, David Fuks. Federica Cipriani, Qu Liu, Luca Aldrighetti, Rong Liu and Ho-Seong Han have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of International robotic and laparoscopic liver resection study group investigators are listed in Acknowledgements section.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kwak, B.J., Lee, J.H., Chin, K.M. et al. Robotic versus laparoscopic liver resections for hepatolithiasis: an international multicenter propensity score matched analysis. Surg Endosc 37, 5855–5864 (2023). https://doi.org/10.1007/s00464-023-10051-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10051-8



