Abstract
Background
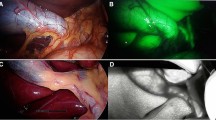
Near-infrared fluorescent cholangiography (NIRFC) with indocyanine green (ICG) as the developer yields clear visualization of the extrahepatic bile ducts and is effective in identifying key structures. Here, we analyzed and compared the surgical outcomes of fluorescent and conventional laparoscopy in cholecystectomy of various difficulties and then assessed the value of NIRFC.
Materials and methods
This retrospective study collected clinical data from partial patients who underwent laparoscopic cholecystectomy (LC) at the Department of Hepatobiliary and Pancreatic Surgery, Zhongnan Hospital of Wuhan University between 2020 and 2021. The study subjects were classified into ICG-assisted and white-light laparoscopy. Two cohorts with homogeneous baseline status were selected based on 1:1 ratio propensity score matching (PSM). Multivariate logistic regression analysis was performed to predict independent risk factors for LC difficulty. Thereafter, the matched cases were classified into difficult and easy subgroups by combining difficulty score and gallbladder disease type, and then the surgical outcomes of the two groups were compared.
Results
This study included a total of 624 patients. The patients were classified into the ICG group (n = 218) and the non-ICG group (n = 218) after a 1:1 ratio PSM. Our data showed significant differences between the groups in operative time (P = 0.020), blood loss (P = 0.016), length of stay (P = 0.036), and adverse reaction (P = 0.023). Stratified analysis demonstrated that ICG did not significantly improve the surgical outcomes in simple cases (n = 208). On the other hand, in difficult cases (n = 228), NIRFC shortened operative time (P = 0.003) and length of stay (P = 0.015), reduced blood loss (P = 0.028) and drain placement rate (P = 0.015), and had fewer adverse reactions (P = 0.023). The data showed that five cases were converted to laparotomy while two cases had minor bile leaks in the non-ICG group. There was no bile duct injury (BDI) in all the cases. Furthermore, high BMI, history of urgent admission and abdominal surgery, palpable gallbladder, thickened wall, and pericholecystic collection were risk factors for surgical difficulty.
Conclusion
ICG-assisted NIRFC provides real-time biliary visualization. In complicated conditions such as acute severe inflammation, dense adhesions, and biliary variants, the navigating ability of fluorescence can enhance the operation progress, reduce the possibility of conversion or serious complications, and improve the efficiency and safety of difficult LC.
Graphical abstract





Similar content being viewed by others
References
Coccolini F, Catena F, Pisano M et al (2015) Open versus laparoscopic cholecystectomy in acute cholecystitis. Systematic review and meta-analysis. Int J Surg. https://doi.org/10.3748/wjg.v27.i36.5989
Pesce A, Piccolo G, Lecchi F et al (2021) Fluorescent cholangiography: an up-to-date overview twelve years after the first clinical application. World J Gastroenterol 27(36):5989–6003
Booij KAC, de Reuver PR, van Dieren S et al (2018) Long-term impact of bile duct injury on morbidity, mortality, quality of life, and work related limitations. Ann Surg 268(1):143–150
Halle-Smith JM, Hodson J, Stevens LG et al (2020) A comprehensive evaluation of the long-term clinical and economic impact of minor bile duct injury. Surgery 167(6):942–949
Parmeggiani D, Cimmino G, Cerbone D et al (2010) Biliary tract injuries during laparoscopic cholecystectomy: three case reports and literature review. G Chir 31(1–2):16–19
Vidrio Duarte R, Martínez Martínez AR, Sr Ortega León LH et al (2020) Transillumination of Calot’s triangle on laparoscopic cholecystectomy: a feasible approach to achieve a critical view of safety. Cureus 12(7):e9113
van de Graaf FW, Zaïmi I, Stassen LPS et al (2018) Safe laparoscopic cholecystectomy: a systematic review of bile duct injury prevention. Int J Surg. https://doi.org/10.1016/j.ijsu.2018.11.006
Asai K, Watanabe M, Kusachi S et al (2014) Risk factors for conversion of laparoscopic cholecystectomy to open surgery associated with the severity characteristics according to the Tokyo guidelines. Surg Today 44(12):2300–2304
Shah AA, Bhatti UF, Petrosyan M et al (2019) The heavy price of conversion from laparoscopic to open procedures for emergent cholecystectomies. Am J Surg 217(4):732–738
Ishizawa T, Tamura S, Masuda K et al (2009) Intraoperative fluorescent cholangiography using indocyanine green: a biliary road map for safe surgery. J Am Coll Surg 208(1):e1-4
Gao Y, Li M, Song ZF et al (2017) Mechanism of dynamic near-infrared fluorescence cholangiography of extrahepatic bile ducts and applications in detecting bile duct injuries using indocyanine green in animal models. J Huazhong Univ Sci Technol 37(1):44–50
Benya R, Quintana J, Brundage B (1989) Adverse reactions to indocyanine green: a case report and a review of the literature. Cathet Cardiovasc Diagn 17(4):231–233
Randhawa JS, Pujahari AK (2009) Preoperative prediction of difficult lap chole: a scoring method. Indian J Surg 71(4):198–201
Törnqvist B, Waage A, Zheng Z et al (2016) Severity of acute cholecystitis and risk of iatrogenic bile duct injury during cholecystectomy, a population-based case-control study. World J Surg 40(5):1060–1067
Gené Škrabec C, Pardo Aranda F, Espín F et al (2020) Fluorescent cholangiography with direct injection of indocyanine green (ICG) into the gallbladder: a safety method to outline biliary anatomy. Langenbecks Arch Surg 405(6):827–832
Jao ML, Wang YY, Wong HP et al (2020) Intracholecystic administration of indocyanine green for fluorescent cholangiography during laparoscopic cholecystectomy-a two-case report. Int J Surg Case Rep. https://doi.org/10.1016/j.ijscr.2020.02.054
Boogerd LSF, Handgraaf HJM, Huurman VAL et al (2017) The best approach for laparoscopic fluorescence cholangiography: overview of the literature and optimization of dose and dosing time. Surg Innov 24(4):386–396
Chen Q, Zhou R, Weng J et al (2021) Extrahepatic biliary tract visualization using near-infrared fluorescence imaging with indocyanine green: optimization of dose and dosing time. Surg Endosc 35(10):5573–5582
Zarrinpar A, Dutson EP, Mobley C et al (2016) Intraoperative laparoscopic near-infrared fluorescence cholangiography to facilitate anatomical identification: when to give indocyanine green and how much. Surg Innov 23(4):360–365
Li X, Li J, Wang H et al (2020) Application of indocyanine green fluorescence imaging in laparoscopic cholecystectomy[J]. Abdom Surg 33(03):194–199
Dip FD, Asbun D, Rosales-Velderrain A et al (2014) Cost analysis and effectiveness comparing the routine use of intraoperative fluorescent cholangiography with fluoroscopic cholangiogram in patients undergoing laparoscopic cholecystectomy. Surg Endosc 28(6):1838–1843
Lehrskov LL, Westen M, Larsen SS et al (2020) Fluorescence or X-ray cholangiography in elective laparoscopic cholecystectomy: a randomized clinical trial. Br J Surg 107(6):655–661
Rungsakulkij N, Thewmorakot S, Suragul W et al (2020) Fluorescence cholangiography enhances surgical residents’ biliary delineation skill for laparoscopic cholecystectomies. World J Gastrointest Surg 12(3):93–103
Berci G, Morgenstern L (1995) An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 180(5):638–639
Avgerinos C, Kelgiorgi D, Touloumis Z et al (2009) One thousand laparoscopic cholecystectomies in a single surgical unit using the “critical view of safety” technique. J Gastroint Surg 13(3):498–503
Sgaramella LI, Gurrado A, Pasculli A et al (2021) The critical view of safety during laparoscopic cholecystectomy: strasberg yes or no? An Italian multicentre study. Surg Endosc 35(7):3698–3708
Strasberg SM, Brunt LM (2010) Rationale and use of the critical view of safety in laparoscopic cholecystectomy. J Am Coll Surg 211(1):132–138
Wakabayashi G, Iwashita Y, Hibi T et al (2018) Tokyo Guidelines 2018: surgical management of acute cholecystitis: safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci 25(1):73–86
Dip F, LoMenzo E, Sarotto L et al (2019) Randomized trial of near-infrared incisionless fluorescent cholangiography. Ann Surg 270(6):992–999
Ankersmit M, van Dam DA, van Rijswijk AS et al (2017) Fluorescent imaging with indocyanine green during laparoscopic cholecystectomy in patients at increased risk of bile duct injury. Surg Innov 24(3):245–252
Jin H, Yang J, Lu L et al (2021) Propensity score matching between conventional laparoscopic cholecystectomy and indocyanine green cholangiography-guided laparoscopic cholecystectomy: observational study. Lasers Med Sci. https://doi.org/10.1007/s10103-021-03401-2
Broderick RC, Lee AM, Cheverie JN et al (2021) Fluorescent cholangiography significantly improves patient outcomes for laparoscopic cholecystectomy. Surg Endosc 35(10):5729–5739
Beksac K, Turhan N, Karaagaoglu E et al (2016) Risk factors for conversion of laparoscopic cholecystectomy to open surgery: a new predictive statistical model. J Laparoendosc Adv Surg Tech A 26(9):693–696
Goonawardena J, Gunnarsson R, de Costa A (2015) Predicting conversion from laparoscopic to open cholecystectomy presented as a probability nomogram based on preoperative patient risk factors. Am J Surg 210(3):492–500
Diana M, Soler L, Agnus V et al (2017) Prospective evaluation of precision multimodal gallbladder surgery navigation: virtual reality, near-infrared fluorescence, and x-ray-based intraoperative cholangiography. Ann Surg 266(5):890–897
Funding
This work was supported by the National Natural Science Foundation of China (32170717) and the Grant from the National Key Research and Development Program of China (SQ2019YFC200078/02).
Author information
Authors and Affiliations
Contributions
This manuscript was written by all the authors, who gave approval of the final version of the manuscript. Chengfan Xu and Maohui Yin contributed equally to the manuscript.
Corresponding authors
Ethics declarations
Disclosures
Chengfan Xu, Maohui Yin, Haitao Wang, Ping Jiang, Zhiyong Yang, Yueming He, Zhonglin Zhang, Zhisu Liu, Bo Liao, and Yufeng Yuan have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, C., Yin, M., Wang, H. et al. Indocyanine green fluorescent cholangiography improves the clinical effects of difficult laparoscopic cholecystectomy. Surg Endosc 37, 5836–5846 (2023). https://doi.org/10.1007/s00464-023-10035-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10035-8