Abstract
Background
Regional variations in healthcare outcomes in England have been historically reported. This study analyses the variations in long term colorectal cancer survival across different regions in England.
Methods
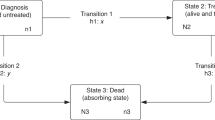
Relative survival analysis of population data obtained from all cancer registries in England between 2010 and 2014.
Results
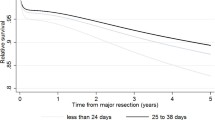
Totally, 167,501 patients were studied. Regions in the southern England had better outcomes with Southwest and Oxford registries having 63.5 and 62.7% 5 year relative survival. In contrast, Trent and Northwest cancer registries had 58.1% relative survival (p < 0.01). The regions in the north fared below the national average. The survival outcomes reflected socio-economic deprivation status, the best performing regions in the south having low levels of deprivation (5.3 and 6.5% having maximum deprivation in Southwest and Oxford, respectively). The regions with worst long term cancer outcomes had high levels of deprivation with 25% and 17% having high levels of deprivation in Northwest and Trent regions.
Conclusion
There are significant variations in long term colorectal cancer survival between different regions in England, southern England had better relative survival when compared with the northern regions. Disparities in socio-economic depravation status in different regions may be associated with worse colorectal cancer outcomes.
Graphical abstract





Similar content being viewed by others
Data availability
Public Health data (PHE) were utilised to write the paper. This data are stored securely and can be made available upon reasonable request after obtaining permission from PHE.
References
Oliver A, Mossialos E (2004) Equity of access to health care: outlining the foundations for action. J Epidemiol Community Heal 58(8):655–658
Bennett JE, Pearson-Stuttard J, Kontis V, Capewell S, Wolfe I, Ezzati M (2018) Contributions of diseases and injuries to widening life expectancy inequalities in England from 2001 to 2016: a population-based analysis of vital registration data. Lancet Public Heal 3(12):e586–e597
Torabi M, Green C, Nugent Z, Mahmud SM, Demers AA, Griffith J et al (2014) Geographical variation and factors associated with colorectal cancer mortality in a universal health care system. Can J Gastroenterol Hepatol 28(4):191
NHS. Long Term Plan » Cancer. https://www.longtermplan.nhs.uk/areas-of-work/cancer/
Walters S, Quaresma M, Coleman MP, Gordon E, Forman D, Rachet B (2011) Geographical variation in cancer survival in England, 1991–2006: an analysis by Cancer Network. J Epidemiol Community Health 65(11):1044–1052
CAS Explorer (2022) C20 - Malignant neoplasms of rectum. https://www.cancerdata.nhs.uk/explorer/tumour_types/Malignant%20neoplasms%20of%20rectum. Accessed 15 Aug 2022
Henson KE, Elliss-Brookes L, Coupland VH, Payne E, Vernon S, Rous B et al (2020) Data resource profile: national cancer registration dataset in England. Int J Epidemiol 49(1):16-16H
Council UMR. Is my study research?
National Insitute for Health and Care Excellence (NICE) (2014) Colorectal cancer: diagnosis and management | Guidance. https://www.nice.org.uk/Guidance/CG131
Public Health England (2021) Bowel cancer screening: programme overview—GOV.UK. https://www.gov.uk/guidance/bowel-cancer-screening-programme-overview#target-population. Accessed 18 Jan 2023
Hirst Y, Stoffel S, Baio G, McGregor L, von Wagner C (2018) Uptake of the English bowel (colorectal) cancer screening programme: an update 5 years after the full roll-out. Eur J Cancer 1(103):267
Department for Communities and Local Government. The English index of multiple deprivation (IMD) 2015-Guidance.
AJCC Cancer Staging Handbook (2017) The AJCC cancer staging manual. Springer, USA
Dickman PW, Adami HO (2006) Interpreting trends in cancer patient survival. J Intern Med 260(2):103–117
University of Leicester, Karolinska Institutet. InterPreT cancer survival: an online interactive cancer survival prediction tool. https://interpret.le.ac.uk/. Accessed 15 Aug 2022
Wickham H (2009) ggplot2
R: The R Foundation (2022). https://www.r-project.org/foundation/. 15 Aug 2022
Sjöström O, Silander G, Syk I, Henriksson R, Melin B, Hellquist BN (2018) Disparities in colorectal cancer between Northern and Southern Sweden—a report from the new RISK North database. Acta Oncol 57(12):1622–1630
Rey G, Jougla E, Fouillet A, Hémon D (2009) Ecological association between a deprivation index and mortality in France over the period 1997–2001: variations with spatial scale, degree of urbanicity, age, gender and cause of death. BMC Public Health 9(1):1–12
Saldana-Ruiz N, Clouston SAP, Rubin MS, Colen CG, Link BG (2013) Fundamental causes of colorectal cancer mortality in the United States: Understanding the importance of socioeconomic status in creating inequality in mortality. Am J Public Health 103(1):99
Wood J (2014) New CCG funding allocations–mapped. https://commonslibrary.parliament.uk/new-ccg-funding-allocations-mapped/. Accessed 19 Jul 2022
Aarts MJ, Lemmens VEPP, Louwman MWJ, Kunst AE, Coebergh JWW (2010) Socioeconomic status and changing inequalities in colorectal cancer? A review of the associations with risk, treatment and outcome. Eur J Cancer 46(15):2681–2695
Afshar N, English DR, Milne RL (2019) Rural–urban residence and cancer survival in high-income countries: a systematic review. Cancer 125(13):2172–2184
Rogers CR, Blackburn BE, Huntington M, Curtin K, Thorpe RJ, Rowe K et al (2020) Rural-urban disparities in colorectal cancer survival and risk among men in Utah: a statewide population-based study. Cancer Causes Control 31(3):241
Campbell NC, Elliott AM, Sharp L, Ritchie LD, Cassidy J, Little J (2000) Rural factors and survival from cancer: analysis of Scottish cancer registrations. Br J Cancer 82(11):1863–1866
Franklyn J, Lomax J, Labib PLZ, Baker A, Balasubramanya S, Natale J et al (2022) Young-onset colorectal cancer: insights from an English population-based study. Colorectal Dis 24:1063
Kontopantelis E, Buchan I, Webb RT, Ashcroft DM, Mamas MA, Doran T (2018) Disparities in mortality among 25–44-year-olds in England: a longitudinal, population-based study. Lancet Public Heal 3(12):e567
Petrelli F, Cortellini A, Indini A, Tomasello G, Ghidini M, Nigro O et al (2021) Association of obesity with survival outcomes in patients with cancer: a systematic review and meta-analysis. JAMA Netw Open 4(3):e213520–e213520
Kajiwara Saito M, Quaresma M, Fowler H, Benitez Majano S, Rachet B (2021) Socioeconomic gaps over time in colorectal cancer survival in England: flexible parametric survival analysis. J Epidemiol Community Heal 75(12):1155–1164
Brown KF, Rumgay H, Dunlop C, Ryan M, Quartly F, Cox A et al (2018) The fraction of cancer attributable to modifiable risk factors in England, Wales, Scotland, Northern Ireland, and the United Kingdom in 2015. Br J Cancer 118(8):1130–1141
Dalton SO, Schüz J, Engholm G, Johansen C, Kjær SK, Steding-Jessen M et al (2008) Social inequality in incidence of and survival from cancer in a population-based study in Denmark, 1994–2003: summary of findings. Eur J Cancer 44(14):2074–2085
Charles A (2022) Integrated care systems explained. The King’s Fund. https://www.kingsfund.org.uk/publications/integrated-care-systems-explained#why-are-they-needed. Accessed 7 Jul 2022
Acknowledgements
We wish to acknowledge Public Health England (PHE) for providing the necessary data for this study.
Funding
The study was funded using a grant from the Bowel cancer West Charity (charity number 1140271).
Author information
Authors and Affiliations
Contributions
JF, JL, AB, SS were involved in conceptualising the project, applying for permission from public health England, writing the manuscript and proof reading. JL, AB, JH were involved in providing expert statistical analysis and proof reading the manuscript. MA and MC were involved in writing the manuscript and proof reading the same.
Corresponding author
Ethics declarations
Disclosures
Mark Coleman has served on the board of the funding charity; however, he declares no conflict of interest and the charity was not involved in the study design, data analysis or manuscript preparation in anyway. Dr Joshua Franklyn, Mr Joe Lomax, Dr Muhamed Abdalkoddus, Dr Joanne Hosking, Dr Amy Baker, Dr Sebastian Smolarek and Dr Mark Coleman declare no financial disclosures, conflicts of interest or relevant financial ties to disclose.
Ethical approval
Ethical review or individual patient consent was not required as anonymised, non-interventional, retrospective data was used. The online National Research Ethics Service decision tool was used to confirm the same.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.

464_2023_10003_MOESM1_ESM.jpg
Supplementary file1 (JPG 71 kb)—Variations in long term relative survival of colon cancer based on various geographical regions in England. Map of England split into the eight cancer registries, with a colour gradient displaying the relative 5 year survival percentage of colon cancer for each registry.

464_2023_10003_MOESM2_ESM.jpg
Supplementary file2 (JPG 70 kb)—Variations in long term relative survival of rectal cancer based on various geographical regions in England. Map of England split into the eight cancer registries, with a colour gradient displaying the relative 5 year survival percentage of colon cancer for each registry.

464_2023_10003_MOESM3_ESM.jpg
Supplementary file3 (JPG 67 kb)—Geographical variations of funding of health services by the Clinical commissioning group (CCG). Map of England showing the distribution of funding to different regions, there are appears to be more money distributed to the northern parts of England in an attempt to level up the country.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Franklyn, J., Lomax, J., Baker, A. et al. Geographical variations in long term colorectal cancer outcomes in England: a contemporary population analysis revealing the north–south divide in colorectal cancer survival. Surg Endosc 37, 5340–5350 (2023). https://doi.org/10.1007/s00464-023-10003-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-10003-2