Abstract
Background
Pediatric endoscopic surgery has become an alternative to conventional techniques with the development of medical equipment. However, there is no formal, standardized curriculum for pediatric endoscopic surgery, and its requirement remains elusive. The purpose of this study is to determine the baseline knowledge of pediatric surgeons that is considered essential for pediatric laparoscopic and thoracoscopic surgery.
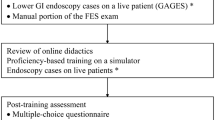
Methods
Sixteen web-based multiple-choice questions based on the fundamental cognitive knowledge of pediatric endoscopic surgery were administered. The questions were created based on the fields covered by the Fundamentals of Laparoscopic Surgery ™ (FLS) certification examination blueprints and eight specific diseases of pediatric surgery. Pediatric surgeons and pediatric surgical trainees participated in this study voluntarily.
Results
A total of 122 surgeons participated through the Japanese Society of Pediatric Surgeons. The response rate was 95% (122/128). The total mean examination score of all participants was 79.4% (77.3–81.4%). There were no significant differences in total scores between the board-certified pediatric surgeons without an endoscopic surgical skill qualification and the non-board-certified pediatric surgeons (80.4% vs. 77.1%, p = 0.12). The endoscopic surgical skill-qualified surgeons had significantly higher percentages of correct responses in specific subjects than board-certified pediatric surgeons and surgeons without pediatric board certification (94.3% vs. 82.9%, p = 0.02; 94.3% vs. 77.5%, p = 0.0002). The FLS original subjects’ scores were not significantly different among them. The mean score of surgeons who had experienced more than 200 cases of endoscopic surgery, including adult cases, was 83.2% (80.4–85.9%).
Conclusions
A knowledge gap exists between surgeons, board-certified pediatric surgeons, and endoscopic surgical skill-qualified surgeons in Japan. In the field of pediatric surgery, an effective formal curriculum, such as FLS, is required to help address this vast knowledge gap for the safe conduct of endoscopic surgeries.

Similar content being viewed by others
References
Fox D, Morrato E, Campagna EJ, Rees DI, Dickinson LM, Partrick DA, Kempe A (2011) Outcomes of laparoscopic versus open fundoplication in children’s hospitals: 2005–2008. Pediatrics 127:872–880. https://doi.org/10.1542/peds.2010-1198
Kalfa N, Allal H, Raux O, Lardy H, Varlet F, Reinberg O, Podevin G, Héloury Y, Becmeur F, Talon I, Harper L, Vergnes P, Forgues D, Lopez M, Guibal M-P, Galifer R-B (2007) Multicentric assessment of the safety of neonatal videosurgery. Surg Endosc 21:303–308. https://doi.org/10.1007/s00464-006-0044-1
Bishay M, Giacomello L, Retrosi G, Thyoka M, Garriboli M, Brierley J, Harding L, Scuplak S, Cross KM, Curry JI, Kiely EM, Coppi PD, Eaton S, Pierro A (2013) Hypercapnia and acidosis during open and thoracoscopic repair of congenital diaphragmatic hernia and esophageal atresia: results of a pilot randomized controlled trial. Ann Surg 258:895–900. https://doi.org/10.1097/SLA.0b013e31828fab55
Yokoyama S, Mizunuma K, Kurashima Y, Watanabe Y, Mizota T, Poudel S, Kikuchi T, Kawai F, Shichinohe T, Hirano S (2019) Evaluation methods and impact of simulation-based training in pediatric surgery: a systematic review. Pediatr Surg Int 35:1085–1094. https://doi.org/10.1007/s00383-019-04539-5
Patel EA, Aydın A, Desai A, Dasgupta P, Ahmed K (2019) Current status of simulation-based training in pediatric surgery: A systematic review. J Pediatr Sur 54:1884–1893. https://doi.org/10.1016/j.jpedsurg.2018.11.019
Brunt LM (2014) FLS: celebrating a decade of innovation in surgical education. Bulletin of the American College of Surgeons. http://bulletin.facs.org/2014/11/fls-celebrating-a-decade-of-innovation-in-surgical-education/#.Wr7zVWbAOnc. Accessed 19 May 2022.
Bilgic E, Kaneva P, Okarinec A, Ritter EM, Schwaitzberg SD, Vassiliou MC (2018) Trends in the Fundamentals of Laparoscopic Surgery® (FLS) certification exam over the past 9 years. Surg Endosc 32:2101–2105. https://doi.org/10.1007/s00464-017-5907-0
Derevianko AY, Schwaitzberg SD, Tsuda S, Barrios L, Brooks DC, Callery MP, Fobert D, Irias N, Rattner DW, Jones DB (2010) Malpractice carrier underwrites fundamentals of laparoscopic surgery training and testing: a benchmark for patient safety. Surg Endosc 24:616–623. https://doi.org/10.1007/s00464-009-0617-x
Hafford ML, Van Sickle KR, Willis RE, Wilson TD, Gugliuzza K, Brown KM, Scott DJ (2013) Ensuring competency: are fundamentals of laparoscopic surgery training and certification necessary for practicing surgeons and operating room personnel? Surg Endosc 27:118–126. https://doi.org/10.1007/s00464-012-2437-7
Watkins R, West-Meiers M, Visser Y (2012) A guide to assessing needs: Tools for collecting information, making decisions, and achieving development results. World Bank, Washington, DC
Mori T, Kimura T, Kitajima M (2010) Skill accreditation system for laparoscopic gastroenterologic surgeons in Japan. Minim Invasive Ther Allied Technol 19:18–23
Japanese congenital diaphragmatic hernias guidelines. https://www.med-amc.com/jcs_society/images/guideline/shouni2019.pdf Accessed 14 May 2022.
Japan Society for Endoscopic Surgery. https://www.jses.or.jp/uploads/files/gijutsunintei/kisoku20211202.pdf. Accessed 14 May 2022.
Shiroshita H, Inomata M, Akira S, Kanayama H, Yamaguchi S, Eguchi S, Wada N, Kurokawa Y, Uchida H, Seki Y, Ieiri S, Iwazaki M, Sato Y, Kitamura K, Tabata M, Mimata H, Takahashi H, Uemura T, Akagi T, Taniguchi F, Miyajima A, Hashizume M, Matsumoto S, Kitano S, Watanabe M, Sakai Y (2021) Current Status of endoscopic surgery in Japan: the 15th national survey of endoscopic surgery by the japan society for endoscopic surgery. Asian J Endosc Surg 2021:1–12. https://doi.org/10.1111/ases.13012
Yeo H, Viola K, Berg D, Lin Z, Smith MN, Cammann C, Bell RH Jr, Sosa JA, Krumholz HM, Curry LA (2009) Attitudes, training experiences, and professional expectations of US general surgery residents: a national survey. JAMA 302:1301–1308. https://doi.org/10.1001/jama.2009.1386
Dawe SR, Pena GN, Windsor JA, Broeders JAJL, Cregan PC, Hewett PJ, Maddern GJ (2014) Systematic review of skills transfer after surgical simulation-based training. Br J Surg 101:1063–1076. https://doi.org/10.1002/bjs.9482
Kirkpatrick D (1996) Great ideas revisited. Techniques for evaluating training programs. Revisiting Kirkpatrick’s Four-Level Model Train Dev 50:54–59
Nakajima K, Wasa M, Takiguchi S, Taniguchi E, Soh H, Ohashi S, Okada A (2003) A modular laparoscopic training program for pediatric surgeons. JSLS 7:33–37
Ieiri S, Nakatsuji T, Higashi M, Akiyoshi J, Uemura M, Konishi K, Onimaru M, Ohuchida K, Hong J, Tomikawa M, Tanoue K, Hashizume M, Taguchi T (2010) Effectiveness of basic endoscopic surgical skill training for pediatric surgeons. Pediatr Surg Int 26:947–954. https://doi.org/10.1007/s00383-010-2665-7
Jimbo T, Ieiri S, Obata S, Uemura M, Souzaki R, Matsuoka N, Katayama T, Masumoto K, Hashizume M, Taguchi T (2015) Effectiveness of short-term endoscopic surgical skill training for young pediatric surgeons: a validation study using the laparoscopic fundoplication simulator. Pediatr Surg Int 31:963–969. https://doi.org/10.1007/s00383-015-3776-y
Breaud J, Talon I, Fourcade L, Podevin G, Rod J, Audry G, Dohin B, Lecompte JF, Bensaid R, Rampal V, Azzie G (2019) The national pediatric surgery simulation program in France: a tool to develop resident training in pediatric surgery. J Pediatr Sur 54:582–586. https://doi.org/10.1016/j.jpedsurg.2018.09.003
Barsness KA (2015) Trends in technical and team simulations: Challenging the status Quo of surgical training. Semin Pediatr Surg 24:130–133. https://doi.org/10.1053/j.sempedsurg.2015.02.011
Acknowledgements
The authors would like to thank the members of the Japanese Society of Pediatric Surgeons and the participant institutes of Kagoshima University, Nagoya University Graduate School of Medicine, Kobe University Graduate School of Medicine, Kyushu University, Saitama Children’s Medical Center, Juntendo University School of Medicine, Osaka University Graduate School of Medicine, The University of Tokyo Hospital, Kyoto prefectural university of medicine, Niigata University Graduate School of Medical and Dental Sciences, Hokkaido Medical Center for Child Health and Rehabilitation, Kitano Hospital, Hokkaido University Graduate School of Medicine, Kagawa University, Tokai University School of Medicine, Nagasaki University Graduate School, Asahikawa Medical University, Mie university hospital, Iwate Medical University School of Medicine, Ehime university hospital, Osaka women’s and children’s hospital, Nara medical university, National Hospital Organization Kokura Medical Center, University of the Ryukyus faculty of medicine and university hospital, University of Tsukuba, Kindai University Nara Hospital, and Fukuoka children’s hospital. We could not have completed the survey study without their support.
Funding
This research received no specific grant from any funding agency.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Shinichiro Yokoyama, Yo Kurashima, Satoshi Ieiri, Atsuyuki Yamataka, Hiroomi Okuyama, Hiroo Uchida, Tetsuya Ishimaru, and Satoshi Hirano have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yokoyama, S., Kurashima, Y., Ieiri, S. et al. Comprehension of fundamental knowledge about pediatric endoscopic surgery: a cross-sectional study in Japan. Surg Endosc 37, 6408–6416 (2023). https://doi.org/10.1007/s00464-023-09975-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-09975-y