Abstract
Introduction
The recurrence rate of hiatal hernia (HH) after laparoscopic surgery with crural repair and Nissen or Toupet fundoplication is high (< 25–42%). HH repair can be reinforced with additional anterior sutures, vertical mesh strips (VMS) or mesh placement but the effect in the long-term (> 1 year) is still unclear. We determined the recurrence rate of HH after surgery and established whether the use of reinforcement techniques could reduce long-term recurrence rates.
Methods
In this retrospective cohort study patients were included if they underwent a laparoscopic fundoplication in this hospital between 2012 and 2019. HH was measured with computed tomography and baseline patient characteristics and surgical details were collected. Primary outcomes were recurrence of symptoms and re-intervention, secondary outcome was effect of surgical reinforcement techniques. Statistical analyses comprised chi-square tests, Mann–Whitney U tests and uni- and multivariable logistic regression analyses.
Results
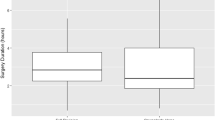
In total, 307 patients were included, 206 women and 101 men. During primary surgery, 208 patients underwent a Toupet fundoplication and 97 patients underwent a Nissen fundoplication. Reinforcements consisted of anterior sutures in 132 patients, VMS in 89 patients and mesh in 17 patients. After primary surgery, recurrence of HH was diagnostically confirmed in 64 patients (20.8%). Use of VMS during primary surgery was significantly associated with fewer recurrences (OR = 0.34, p = 0.048), corrected for confounding factors. Secondary surgery was performed in 54 patients (17.6%) and tertiary surgery in five patients (1.6%). Mesh and VMS were used more during secondary and tertiary surgery.
Conclusion
The recurrence rate among HH patients in this cohort study was 20.8% with a mean follow-up time of 6 years. Secondary surgery was performed in 17.6% of the patients. In future, the use of VMS might lead to fewer recurrences after primary laparoscopic repair of HH.
Graphical abstract






Similar content being viewed by others
References
Westcott LZ, Ward M (2020) Techniques for closing the hiatus: mesh, pledgets and suture techniques. Ann Laparosc Endosc Surg 5:16
Kohn GP, Price RR, DeMeester SR, Zehetner J, Muensterer OJ, Awad Z et al (2013) Guidelines for the management of hiatal hernia. Surg Endosc 27(12):4409–4428
Saad AR, Velanovich V (2020) Anatomic observation of recurrent hiatal hernia: recurrence or disease progression? J Am Coll Surg 230(6):999–1007
Zaman JA, Lidor AO (2016) The optimal approach to symptomatic paraesophageal hernia repair: important technical considerations. Curr Gastroenterol Rep 18(10):53
Lidor AO, Steele KE, Stem M, Fleming RM, Schweitzer MA, Marohn MR (2015) Long-term quality of life and risk factors for recurrence after laparoscopic repair of paraesophageal hernia. JAMA Surg 150(5):424–431
Acosta MA, Cuesta MA, Bruna M (2021) Atlas of minimally invasive techniques in upper gastrointestinal surgery. Springer, Cham
Sathasivam R, Bussa G, Viswanath Y, Obuobi R-B, Gill T, Reddy A et al (2019) ‘Mesh hiatal hernioplasty’ versus ‘suture cruroplasty’ in laparoscopic para-oesophageal hernia surgery; a systematic review and meta-analysis. Asian J Surg 42(1):53–60
Van Den Dop LM, De Smet GHJ, Mamound A, Lange J, Wijnhoven BPL, Hueting W (2021) Use of polypropylene strips for reinforcement of the cruroplasty in laparoscopic paraesophageal hernia repair: a retrospective cohort study. Dig Surg 38(4):290–299
Granderath FA, Schweiger UM, Pointner R (2007) Laparoscopic antireflux surgery: tailoring the hiatal closure to the size of hiatal surface area. Surg Endosc 21(4):542–548
Granderath FA, Schweiger UM, Kamolz T, Asche KU, Pointner R (2005) Laparoscopic Nissen fundoplication with prosthetic hiatal closure reduces postoperative intrathoracic wrap herniation: preliminary results of a prospective randomized functional and clinical study. Arch Surg 140(1):40–48
Oor JE, Roks DJ, Koetje JH, Broeders JA, van Westreenen HL, Nieuwenhuijs VB et al (2018) Randomized clinical trial comparing laparoscopic hiatal hernia repair using sutures versus sutures reinforced with non-absorbable mesh. Surg Endosc 32(11):4579–4589
Stadlhuber RJ, Sherif AE, Mittal SK, Fitzgibbons RJ Jr, Michael Brunt L, Hunter JG et al (2009) Mesh complications after prosthetic reinforcement of hiatal closure: a 28-case series. Surg Endosc 23(6):1219–1226
Nissen R (1956) A simple operation for control of reflux esophagitis. Schweizerische medizinische Wochenschrift 86(Suppl 20):590–592
Dallemagne B, Weerts JM, Jehaes C, Markiewicz S, Lombard R (1991) Laparoscopic Nissen fundoplication: preliminary report. Surg Laparosc Endosc 1(3):138–143
Tian Z-c, Wang B, Shan C-x, Zhang W, Jiang D-z, Qiu M (2015) A meta-analysis of randomized controlled trials to compare long-term outcomes of Nissen and Toupet fundoplication for gastroesophageal reflux Disease. PLoS ONE 10(6):e0127627
Broeders JAJL, Mauritz FA, Ahmed Ali U, Draaisma WA, Ruurda JP, Gooszen HG et al (2010) Systematic review and meta-analysis of laparoscopic Nissen (posterior total) versus Toupet (posterior partial) fundoplication for gastro-oesophageal reflux disease. Br J Surg 97(9):1318–1330
Toupet AC (1963) Technique d’oesophago-gastroplastie avec phréno-gastropexie appliquée dans la cure radicale des hernies hiatales et comme complément de l’opération de Heller dans les cardiospasmes. Mem Acad Chir 89:394–399
Watson DI, Jamieson GG, Pike GK, Davies N, Richardson M, Devitt PG (1999) Prospective randomized double-blind trial between laparoscopic Nissen fundoplication and anterior partial fundoplication. Br J Surg 86(1):123–130
Bell RC, Hanna P, Mills MR, Bowrey D (1999) Patterns of success and failure with laparoscopic Toupet fundoplication. Surg Endosc 13(12):1189–1194
Collis JL (1957) An operation for hiatus hernia with short oesophagus. Thorax 12(3):181–188
Karatay E, Gok MA, Javadov M (2021) Measurement of hiatal surface area and other hiatus oesophageal diameters at computed tomography imaging in patients with gastroesophageal reflux disease and its relationship with hiatal hernia. J Minim Access Surg 17(4):537–541
Granderath FA, Schweiger UM, Kamolz T, Pasiut M, Haas CF, Pointner R (2002) Laparoscopic antireflux surgery with routine mesh-hiatoplasty in the treatment of gastroesophageal reflux disease. J Gastrointest Surg 6(3):347–353
Kang T, Urrego H, Gridley A, Richardson WS (2014) Pledgeted repair of giant hiatal hernia provides excellent long-term results. J Laparoendosc Adv Surg Tech A 24(10):684–687
Weitzendorfer M, Pfandner R, Antoniou SA, Schwaiger-Hengstschläger C, Emmanuel K, Koch OO (2019) Short-term results after laparoscopic repair of giant hiatal hernias with pledgeted sutures: a retrospective analysis. Hernia 23(2):397–401
Watson DI, Thompson SK, Devitt PG, Smith L, Woods SD, Aly A et al (2015) Laparoscopic repair of very large hiatus hernia with sutures versus absorbable mesh versus nonabsorbable mesh: a randomized controlled trial. Ann Surg 261(2):282–289
Frantzides CT, Carlson MA, Loizides S, Papafili A, Luu M, Roberts J et al (2010) Hiatal hernia repair with mesh: a survey of SAGES members. Surg Endosc 24(5):1017–1024
Gibson SC, Wong SK, Dixon AC, Falk GL (2013) Laparoscopic repair of giant hiatus hernia: prosthesis is not required for successful outcome. Surg Endosc 27(2):618–623
Furtado RV, Vivian SJ, van der Wall H, Falk GL (2016) Medium-term durability of giant hiatus hernia repair without mesh. Ann R Coll Surg Engl 98(7):450–455
Acknowledgements
We are grateful to all surgeons who performed the laparoscopic fundoplications in this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs Berdel Akmaz, Amber Hameleers, Dr Evert-Jan G Boerma, Dr Roy FA Vliegen, Prof Dr Jan Willem M Greve, Drs Berry Meesters and Dr Jan HMB Stoot have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Akmaz, B., Hameleers, A., Boerma, E.G. et al. Hiatal hernia recurrences after laparoscopic surgery: exploring the optimal technique. Surg Endosc 37, 4431–4442 (2023). https://doi.org/10.1007/s00464-023-09907-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-09907-w