Abstract
Background
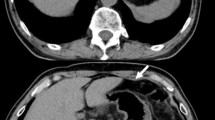
Patients requiring percutaneous endoscopic gastrostomy (PEG) for amyotrophic lateral sclerosis (ALS) related dysphagia represent a clinical challenge. Diminished pulmonary function and aspiration risks can lead to anesthesia-related complications, and gastric displacement from hemidiaphragm elevation may preclude safe gastric access. This study reports the efficacy and outcomes of a dedicated anesthesia/surgery management protocol for ALS patients undergoing PEG.
Methods
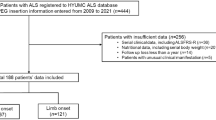
In 2013, a PEG placement protocol for ALS patients was developed emphasizing efficient pre-operative evaluation, rapidly metabolized anesthetic agents, and minimization of opioid use. Outcomes were analyzed retrospectively. Preoperative weight loss, pulmonary function tests, total analgesia, procedural time, and 90-day morbidity and mortality were recorded.
Results
From 2013–2019, 67 ALS patients (mean age 65.3 years, 52.2% female) received a PEG under the protocol. Mean percentage weight loss 6 months before PEG was 9.3 ± 5.1% with 38.8% of patients meeting criteria for severe malnutrition. Mean anesthesia time (propofol induction to anesthesia emergence) was 34.5 ± 10.8 min and mean operative time (endoscope insertion to dressing placement) was 16.4 ± 8.2 min. Regional anesthesia with liposomal bupivacaine was performed in 76.1%. All attempts at PEG placement were successful. With a mean follow-up of 6.1 ± 6.8 months, all PEGs were functional and there were no surgical site complications. Thirty-day readmission rate was 7.0% and 90-day mortality was 22.4% (46.7% occurring within 30 days). Mean time from surgery to death was 8.8 ± 7.8 months.
Conclusions
Protocols for optimizing PEG may help overcome challenges present in the ALS patient population. Despite patient comorbidities, protocol implementation and dedicated team members resulted in a high procedural success rate and low complication rate. Further study is warranted to optimize the timing of PEG placement in relation to ALS disease progression and determine the utility of regional anesthesia during PEG placement.

Similar content being viewed by others
References
Miller RG et al (2009) Practice parameter update: the care of the patient with amyotrophic lateral sclerosis: drug, nutritional, and respiratory therapies (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 73(15):1218–1226
Cui F et al (2018) Therapeutic effects of percutaneous endoscopic gastrostomy on survival in patients with amyotrophic lateral sclerosis: a meta-analysis. PLoS ONE 13(2):e0192243
Bond L et al (2019) A comprehensive examination of percutaneous endoscopic gastrostomy and its association with amyotrophic lateral sclerosis patient outcomes. Brain Sci 9(9):223
Czell D et al (2013) Outcomes of percutaneous endoscopic gastrostomy tube insertion in respiratory impaired amyotrophic lateral sclerosis patients under noninvasive ventilation. Respir Care 58(5):838–844
Sato Y et al (2017) Safety of unsedated PEG placement using transoral ultrathin endoscopy in patients with amyotrophic lateral sclerosis. Nutr Neurosci 20(1):71–75
Thompson AG et al (2017) A risk stratifying tool to facilitate safe late-stage percutaneous endoscopic gastrostomy in ALS. Amyotroph Lateral Scler Frontotemporal Degener 18(3–4):243–248
Yang B, Shi X (2017) Percutaneous endoscopic gastrostomy versus fluoroscopic gastrostomy in amyotrophic lateral sclerosis (ALS) sufferers with nutritional impairment: A meta-analysis of current studies. Oncotarget 8(60):102244–102253
White JV et al (2012) Consensus statement: Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition (undernutrition). JPEN J Parenter Enteral Nutr 36(3):275–283
Carbó Perseguer J, Madejón Seiz A, Romero Portales M, et al (2019) Percutaneous endoscopic gastrostomy in patients with amyotrophic lateral sclerosis: Mortality and complications. Neurologia (Engl Ed) 34(9):582–588
Blondet A et al (2010) Radiologic versus endoscopic placement of percutaneous gastrostomy in amyotrophic lateral sclerosis: multivariate analysis of tolerance, efficacy, and survival. J Vasc Interv Radiol 21(4):527–533
Bokuda K et al (2016) Predictive factors for prognosis following unsedated percutaneous endoscopic gastrostomy in ALS patients. Muscle Nerve 54(2):277–283
de Carvalho M, Gooch CL (2017) The yin and yang of gastrostomy in the management of ALS: friend or foe? Neurology 89:1435–1436
Wolf J et al (2014) Factors predicting one-year mortality in amyotrophic lateral sclerosis patients–data from a population-based registry. BMC Neurol 14:197
Su WM et al (2021) Predictors of survival in patients with amyotrophic lateral sclerosis: a large meta-analysis. EBioMedicine 74:103732
Hasan MS et al (2011) Open gastrostomy under ultrasound-guided bilateral oblique subcostal transversus abdominis plane block: a case series. Eur J Anaesthesiol 28(12):888–889
Lee AR, Choe YS (2015) Anesthesia experience for open gastrostomy with ultrasound-guided unilateral subcostal transversus abdominis plane block in a high risk elderly patient: a case report. Anesth Pain Med 5(4):e24890
Kalava A et al (2016) Bilateral thoracic paravertebral nerve blocks for placement of percutaneous radiologic gastrostomy in patients with amyotrophic lateral sclerosis: a case series. Rom J Anaesth Intensive Care. 23:149–153
Acknowledgements
The authors have no acknowledgements to make.
Funding
No internal or external financial support was used for this report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Eric Pauli reports speaking and teaching honoraria Beckton, Dickinson and Company (BD), Medtronic, PLC, Ovesco Endoscopy AG and Boston Scientific Corp.; consultant fees from Boston Scientific Corp., Actuated Medical, Inc., Baxter International, Inc., Wells Fargo & Company, Cook Biotech, Inc., CMR Surgical, Neptune Medical, Surgimatix, Inc., Boehringer Laboratories, Inc., Allergan, PLC and Noah Medical; royalties from Springer and UpToDate, Inc.; financial interests in International Hernia Collaboration, Inc., Contamination Source Identification and Cranial Devices, Inc. Joshua Winder receives consultant fees from Boston Scientific Corp unrelated to this report. Vamsi Alli receives research support from Actuated Medical unrelated to this report. David Morrell, Marvin Chau, Edward Stredny, Elizabeth Sinz, Sprague Hazard and Zachary Simmons have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Morrell, D.J., Chau, M.H., Winder, J.S. et al. Percutaneous endoscopic gastrostomy in amyotrophic lateral sclerosis: outcomes of a dedicated anesthesia and surgery protocol. Surg Endosc 37, 4338–4344 (2023). https://doi.org/10.1007/s00464-023-09896-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-09896-w