Abstract
Background
Colorectal liver metastases (CRLM) occur in roughly half of patients with colorectal cancer. Minimally invasive surgery (MIS) has become an increasingly acceptable and utilized technique for resection in these patients, but there is a lack of specific guidelines on the use of MIS hepatectomy in this setting. A multidisciplinary expert panel was convened to develop evidence-based recommendations regarding the decision between MIS and open techniques for the resection of CRLM.
Methods
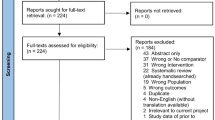
Systematic review was conducted for two key questions (KQ) regarding the use of MIS versus open surgery for the resection of isolated liver metastases from colon and rectal cancer. Evidence-based recommendations were formulated using the GRADE methodology by subject experts. Additionally, the panel developed recommendations for future research.
Results
The panel addressed two KQs, which pertained to staged or simultaneous resection of resectable colon or rectal metastases. The panel made conditional recommendations for the use of MIS hepatectomy for both staged and simultaneous resection when deemed safe, feasible, and oncologically effective by the surgeon based on the individual patient characteristics. These recommendations were based on low and very low certainty of evidence.
Conclusions
These evidence-based recommendations should provide guidance regarding surgical decision-making in the treatment of CRLM and highlight the importance of individual considerations of each case. Pursuing the identified research needs may help further refine the evidence and improve future versions of guidelines for the use of MIS techniques in the treatment of CRLM.
Similar content being viewed by others
References
Siegel RL, Miller KD, Goding Sauer A, Fedewa SA, Butterly LF, Anderson JC et al (2020) Colorectal cancer statistics, 2020. CA: Cancer J Clin. https://doi.org/10.3322/caac.21601
Stiles ZE, Behrman SW, Glazer ES, Deneve JL, Dong L, Wan JY et al (2017) Predictors and implications of unplanned conversion during minimally invasive hepatectomy: an analysis of the ACS-NSQIP database. HPB (Oxford) 19(11):957–965
Carpenter EAA, Valdera F et al (2022) Modern trends in minimally invasive versus open hepatectomy for colorectal liver metastasis: an analysis of ACS-NSQIP. Surg Endosc. https://doi.org/10.1007/s00464-022-09749-y
Famularo S, Donadon M, Cipriani F, Ardito F, Carissimi F, Perri P et al (2020) Hepatocellular carcinoma surgical and oncological trends in a national multicentric population: the HERCOLES experience. Updates Surg. https://doi.org/10.1007/s13304-020-00733-6
Pan L, Tong C, Fu S, Fang J, Gu Q, Wang S et al (2020) Laparoscopic procedure is associated with lower morbidity for simultaneous resection of colorectal cancer and liver metastases: an updated meta-analysis. World J Surg Oncol 18(1):251
Takasu C, Shimada M, Sato H, Miyatani T, Imura S, Morine Y et al (2014) Benefits of simultaneous laparoscopic resection of primary colorectal cancer and liver metastases. Asian J Endosc Surg 7(1):31–37
Ivanecz A, Krebs B, Stozer A, Jagric T, Plahuta I, Potrc S (2018) Simultaneous pure laparoscopic resection of primary colorectal cancer and synchronous liver metastases: a single institution experience with propensity score matching analysis. Radiol Oncol 52(1):42–53
Kawakatsu S, Ishizawa T, Fujimoto Y, Oba A, Mise Y, Inoue Y et al (2021) Impact on operative outcomes of laparoscopic simultaneous resection of colorectal cancer and synchronous liver metastases. Asian J Endosc Surg 14(1):34–43
Okuno M, Goumard C, Mizuno T, Omichi K, Tzeng CD, Chun YS et al (2018) Operative and short-term oncologic outcomes of laparoscopic versus open liver resection for colorectal liver metastases located in the posterosuperior liver: a propensity score matching analysis. Surg Endosc 32(4):1776–1786
Fretland AA, Aghayan DL, Edwin B (2019) Long-term survival after laparoscopic versus open resection of colorectal liver metastases. J Clin Oncol. https://doi.org/10.1200/JCO.2019.37.18_suppl.LBA3516
Fretland AA, Dagenborg VJ, Bjornelv GMW, Kazaryan AM, Kristiansen R, Fagerland MW et al (2018) Laparoscopic versus open resection for colorectal liver metastases: the OSLO-COMET randomized controlled trial. Ann Surg 267(2):199–207
Robles-Campos R, Lopez-Lopez V, Brusadin R, Lopez-Conesa A, Gil-Vazquez PJ, Navarro-Barrios A et al (2019) Open versus minimally invasive liver surgery for colorectal liver metastases (LapOpHuva): a prospective randomized controlled trial. Surg Endosc 33(12):3926–3936
Ozair A, Collings A, Adams A et al (2022) Minimally invasive versus open hepatectomy for the resection of colorectal liver metastases: a systemic review and meta-analysis. Surg Endosc 36(11):7915–7937
Alonso-Coello P, Oxman AD, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M et al (2016) GRADE evidence to decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 2: clinical practice guidelines. BMJ. https://doi.org/10.1136/bmj.i2089
Alonso-Coello P, Schunemann HJ, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M et al (2016) GRADE evidence to decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: introduction. BMJ. https://doi.org/10.1136/bmj.i2016
Andrews JC, Schunemann HJ, Oxman AD, Pottie K, Meerpohl JJ, Coello PA et al (2013) GRADE guidelines: 15. Going from evidence to recommendation-determinants of a recommendation’s direction and strength. J Clin Epidemiol 66(7):726–735
Chen Y, Yang K, Marusic A, Qaseem A, Meerpohl JJ, Flottorp S et al (2017) A reporting tool for practice guidelines in health care: the RIGHT statement. Ann Intern Med 166(2):128–132
Rogers AT, Dirks R, Burt HA, Haggerty S, Kohn GP, Slater BJ et al (2021) Society of American Gastrointestinal and endoscopic surgeons (SAGES) guidelines development: standard operating procedure. Surg Endosc 35(6):2417–2427
GRADEpro GDT: GRADEpro guideline development tool.: McMaster University (developed by Evidence Prime, Inc.); Available from: www.gradepro.org.
Schunemann HJ, Brozek J, Guyatt G, Oxman AD. (2013) GRADE handbook for grading quality of evidence and strength of recommendations: The GRADE Working Group; 2013 [updated Updated October 2013]. Available from: https://guidelinedevelopment.org/handbook.
Kasai M, Van Damme N, Berardi G, Geboes K, Laurent S, Troisi RI (2018) The inflammatory response to stress and angiogenesis in liver resection for colorectal liver metastases: a randomized controlled trial comparing open versus laparoscopic approach. Acta Chir Belg 118(3):172–180
Aghayan DL, Kazaryan AM, Dagenborg VJ, Rosok BI, Fagerland MW, Waaler Bjornelv GM et al (2021) Long-term oncologic outcomes after laparoscopic versus open resection for colorectal liver metastases : a randomized trial. Ann Intern Med 174(2):175–182
Huh JW, Koh YS, Kim HR, Cho CK, Kim YJ (2011) Comparison of laparoscopic and open colorectal resections for patients undergoing simultaneous R0 resection for liver metastases. Surg Endosc 25(1):193–198
Jung KU, Kim HC, Cho YB, Kwon CH, Yun SH, Heo JS et al (2014) Outcomes of simultaneous laparoscopic colorectal and hepatic resection for patients with colorectal cancers: a comparative study. J Laparoendosc Adv Surg Tech A 24(4):229–235
Shin JK, Kim HC, Lee WY, Yun SH, Cho YB, Huh JW et al (2020) Comparative study of laparoscopic versus open technique for simultaneous resection of colorectal cancer and liver metastases with propensity score analysis. Surg Endosc 34(11):4772–4780
Hu MG, Ou-yang CG, Zhao GD, Xu DB, Liu R (2012) Outcomes of open versus laparoscopic procedure for synchronous radical resection of liver metastatic colorectal cancer: a comparative study. Surg Laparosc Endosc Percutan Tech 22(4):364–369
Chen KY, Xiang GA, Wang HN, Xiao FL (2011) Simultaneous laparoscopic excision for rectal carcinoma and synchronous hepatic metastasis. Chin Med J (Engl) 124(19):2990–2992
Goumard C, Nancy You Y, Okuno M, Kutlu O, Chen HC, Simoneau E et al (2018) Minimally invasive management of the entire treatment sequence in patients with stage IV colorectal cancer: a propensity-score weighting analysis. HPB (Oxford) 20(12):1150–1156
Xu X, Guo Y, Chen G, Li C, Wang H, Dong G (2018) Laparoscopic resections of colorectal cancer and synchronous liver metastases: a case controlled study. Minim Invasive Ther Allied Technol 27(4):209–216
Ratti F, Catena M, Di Palo S, Staudacher C, Aldrighetti L (2016) Impact of totally laparoscopic combined management of colorectal cancer with synchronous hepatic metastases on severity of complications: a propensity-score-based analysis. Surg Endosc 30(11):4934–4945
Kawaguchi Y, Fuks D, Kokudo N, Gayet B (2018) Difficulty of laparoscopic liver resection: proposal for a new classification. Ann Surg 267(1):13–17
Tanaka S, Kawaguchi Y, Kubo S, Kanazawa A, Takeda Y, Hirokawa F et al (2019) Validation of index-based IWATE criteria as an improved difficulty scoring system for laparoscopic liver resection. Surgery 165(4):731–740
Acknowledgements
We would like to thank Sarah Colon, the SAGES senior program coordinator, Holly Burt, the SAGES librarian, and the SAGES guideline committee members for their help with the creation of this guideline.
Disclaimer
Clinical practice guidelines are intended to indicate the best available approach to medical conditions as established by a systematic review of available data and expert opinion. The approach suggested may not necessarily be the only acceptable approach given the complexity of the healthcare environment. These guidelines are intended to be flexible, as the surgeon must always choose the approach best suited to the patient and to the variables at the moment of decision. These guidelines are applicable to all physicians who are appropriately credentialed regardless of specialty and address the clinical situation in question. These guidelines are developed under the auspices of SAGES and AHPBA, the guidelines committee, and approved by the Board of Governors of both societies. The recommendations of each guideline undergo multidisciplinary review and are considered valid at the time of production based on the data available. New developments in medical research and practice pertinent to each guideline are reviewed, and guidelines are periodically updated.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Vreeland receives financial support for travel expenses and registration fees for meetings from the Metis Foundation and consulting fees from Bantam Pharmaceuticals for clinical trial design. Dr. Collings was employed by SAGES as the guideline’s fellow. Dr. Adams receives financial support for travel expenses and registration fees for annual meetings for SAGES and AHPBA from the Metis Foundation. Dr. Dirks has privately purchased stock in Johnson & Johnson. Dr. Ansari is a consultant guideline methodologist and remunerated by SAGES for contribution to this work. Dr. Cleary receives consulting fees from Ethicon, Erbe, and Olympus. Dr. Buell receives speaker and consulting fees from Ethicon and Covidien. Dr. Slater receives consulting fees from Bolder Surgical and Cook Medical. Dr. Pryor receives speaker fees from Gore, Ethicon, and Stryker. Dr. Jeyarajah is a consultant for Ethicon, Angiodynamics, and Sirtex. Drs. Ozair, Kushner, Sucandy, Morrell, Cloyd, Ceppa, Abou-Setta, Alseidi, Awad, Ayloo, Orthopoulos, Richardson, Sbayi, Wakabayashi, and Mr. Whiteside have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vreeland, T.J., Collings, A.T., Ozair, A. et al. SAGES/AHPBA guidelines for the use of minimally invasive surgery for the surgical treatment of colorectal liver metastases (CRLM). Surg Endosc 37, 2508–2516 (2023). https://doi.org/10.1007/s00464-023-09895-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-023-09895-x