Abstract
Background and aims
Benign duodenal stenosis (BDS) is most commonly caused by peptic ulcer disease (PUD). Endoscopic balloon dilation (EBD) is the recommended initial management despite limited supporting literature. Our study investigated the etiologic spectrum of BDS and its response to endoscopic dilation.
Methods
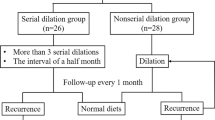
We performed a cohort study of a prospectively maintained database of BDS at our large tertiary academic center between 2002 and 2018. All patients who underwent EBD were analyzed. Dilation was performed using through-the-scope balloons. Technical and clinical successes of initial and repeat EBD were compared. Descriptive statistics, univariate, and multivariate analysis were performed.
Results
The study included 86 patients with 54.7% female gender. Etiologies included 39 patients with PUD (45.3%), 19 patients with Crohn’s disease (22.1%), 23 patients had idiopathic etiologies (26.7%), and 5 patients were listed as other etiologies (5.8%). Proximal stricture location (1st part of duodenum) occurred in 66% of females, whereas distal duodenal involvement was seen in 63.6% of males (p value 0.007). Usage of PPI was associated with 3.6 times higher clinical success rate (p value 0.04). Technical (97.4%) and clinical (77.8%) successes for index dilations in PUD were not significantly better than those of non-PUD patients (p values 0.99, 0.52).
Conclusion
EBD has both a high technical and clinical success for BDS regardless of etiology and should be considered over initial surgical intervention due to low risk profile. Males tend to have more distal duodenal involvement, and PPI usage is an independent predictor for clinical success.
Similar content being viewed by others
References
Sigmon DF, Eovaldi BJ, Cohen HL (2022) Duodenal atresia and stenosis. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470548/. Accessed 29 Aug 2022
Kochhar R, Kochhar S (2010) Endoscopic balloon dilation for benign gastric outlet obstruction in adults. World J Gastrointest Endosc 2(1):29–35
Bruno MJ, Maluf-Filho F (2019) Palliation of malignant pancreaticobiliary obstruction. In: Chandrasekhar V et al (eds) Clinical gastrointestinal endoscopy, 3rd edn. Elsevier, Philadelphia, PA, pp 734–747
Mangiavillano B, Khashab MA, Tarantino I et al (2019) Success and safety of endoscopic treatments for concomitant biliary and duodenal malignant stenosis: A review of the literature. World J Gastrointest Surg 11(2):53–61
Shone DN, Nikoomanesh P, Smith-Meek MM, Bender JS (1995) Malignancy is the most common cause of gastric outlet obstruction in the era of H2 blockers. Am J Gastroenterol 90(10):1769–1770
Kozoll DD, Meyer KA (1964) Obsturcting Gastroduodenal Ulcer. Symptoms and Signs Arch Surg 89:491–498
Jaffin BW, Kaye MD (1985) The prognosis of gastric outlet obstruction. Ann Surg 201(2):176–179
Weiland D, Dunn DH, Humphrey EW, Schwartz ML (1982) Gastric outlet obstruction in peptic ulcer disease: an indication for surgery. Am J Surg 143:90–93
Chaudhary A, Puri AS, Dhar P, Reddy P, Sachdev A, Lahoti D, Kumar N, Broor SL (1996) Elective surgery for corrosive induced gastric injury. World J Surg 20:703–706; discussion 706
Yusuf TE, Brugge WR (2006) Endoscopic therapy of benign pyloric stenosis and gastric outlet obstruction. Curr Opin Gastroenterol 22:570–573
Cherian PT, Cherian S, Singh P (2007) Long-term follow-up of patients with gastric outlet obstruction related to peptic ulcer disease treated with endoscopic balloon dilatation and drug therapy. Gastrointest Endosc 66(3):491–497
Kochhar R, Sethy PK, Nagi B et al (2004) Endoscopic balloon dilatation of benign gastric outlet obstruction. J Gastroenterol Hepatol 19:418–422
Hamzaoui L, Bouassida M, Ben Mansour I et al (2015) Balloon dilatation in patients with gastric outlet obstruction related to peptic ulcer disease. Arab J Gastroenterol 16(3–4):121–124
Kochhar R, Malik S, Gupta P et al (2018) Etiological spectrum and response to endoscopic balloon dilation in patients with benign gastric outlet obstruction. Gastrointest Endosc 88(6):899–908
Rana SS, Bhasin DK, Chandail VS et al (2011) Endoscopic balloon dilatation without fluoroscopy for treating gastric outlet obstruction because of benign etiologies. Surg Endosc 25:1579–1584
Maharshi S, Puri AS, Sachdeva S et al (2016) Aetiological spectrum of benign gastric outlet obstruction in India: new trends. Trop Doct 46:186–191
Fallone CA, Chiba N, van Zanten SV et al (2016) The Toronto Consensus for the Treatment of Helicobacter pylori Infection in Adults. Gastroenterology 151(1):51–69
Boylan JJ, Gradzka MI (1999) Long-term results of endoscopic balloon dilatation for gastric outlet obstruction. Dig Dis Sci 44:1883–1886
Solt J, Bajor J, Szabo M et al (2003) Long-term results of balloon catheter dilation for benign gastric outlet stenosis. Endoscopy 35:490–495
Feldman M, Friedman LS, Brandt LJ (2016) Sleisenger and Fordtran’s gastrointestinal and liver disease: pathophysiology/diagnosis/management, vol 2, 10th edn. Saunders/Elsevier, Philadelphia, PA (p xxxi, 2369, 2389)
Fortun PJ, Hawkey CJ (2007) Nonsteroidal antiinflammatory drugs and the small intestine. Curr Opin Gastroenterol 23(2):134–141
Gajendran M, Loganathan P, Catinella AP, Hashash JG (2018) A comprehensive review and update on Crohn’s disease. Dis Mon 64(2):20–57
Bessissow T, Reinglas J, Aruljothy A, Lakatos PL, Van Assche G (2018) Endoscopic management of Crohn’s strictures. World J Gastroenterol 24(17):1859–1867
Williams AJ, Palmer KR (1991) Endoscopic balloon dilatation as a therapeutic option in the management of intestinal strictures resulting from Crohn’s disease. Br J Surg 78(4):453–454
Funding
None.
Author information
Authors and Affiliations
Contributions
VC participated in conception and design, analysis and interpretation of data, drafting of the article, critical revision of the article for important intellectual content; YAO participated in analysis and interpretation of the data; CRSL participated in conception and design, analysis and interpretation of the data, and final approval of the article; PC participated in conception and design and final approval of the article.
Corresponding author
Ethics declarations
Disclosures
Drs. Vibhu Chittajallu, Yazan Abu Omar, C. Roberto Simons-Linares, and Prabhleen Chahal have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chittajallu, V., Omar, Y.A., Simons-Linares, C.R. et al. Endoscopic balloon dilation management for benign duodenal stenosis. Surg Endosc 37, 3610–3618 (2023). https://doi.org/10.1007/s00464-022-09844-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09844-0