Abstract
Background
The use of duckbill-type anti-reflux metal stents (DMS) in reinterventions after covered metal stent (CMS) dysfunction has been reported in patients with distal malignant biliary obstruction (MBO). However, the superiority of DMS over conventional CMS (c-CMS) has not been established. Therefore, we conducted this retrospective study to evaluate the long-term efficacy and safety of DMS as a second stent in comparison with c-CMS.
Methods
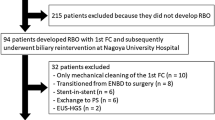
We investigated consecutive patients with distal MBO due to unresectable pancreatic cancer who underwent reintervention after dysfunction of initial biliary CMS at our institution. We compared causes of recurrent biliary obstruction (RBO), time to RBO (TRBO), adverse events (AEs), and reintervention rates of DMS and c-CMS in this stenting.
Results
A total of 76 patients were included (DMS 41 and c-CMS 35). While overall RBO rates were similar between the two groups (46% vs. 63%, p = 0.172), RBO due to non-occlusion cholangitis tended to be less frequent in the DMS group than in the c-CMS group (2% vs. 14%, p = 0.089). Median TRBO was significantly longer in the DMS group (286 days vs. 112 days, p = 0.029). DMS was identified as the only significant risk factor for TRBO (hazard ratio, 0.52; p = 0.044). Overall AE rates were significantly lower in the DMS group (2% vs. 23%, p = 0.010), with non-occlusion cholangitis being the most common AE in the c-CMS group. Endoscopic reintervention was successfully performed in all patients in both groups, despite failed stent removal in 15% of patients in DMS group.
Conclusions
DMS was associated with a significantly longer TRBO and lower rate of AEs compared with c-CMS in reinterventions after initial CMS dysfunction. DMS may be preferable to c-CMS as a second stent after biliary CMS dysfunction.



Similar content being viewed by others
Abbreviations
- MBO:
-
Malignant biliary obstruction
- PC:
-
Pancreatic cancer
- SEMS:
-
Self-expandable metal stent
- CMS:
-
Covered metal stent
- RBO:
-
Recurrent biliary obstruction
- c-CMS:
-
Conventional covered metal stent
- ARMS:
-
Anti-reflux metal stent
- ARV:
-
Anti-reflux valve
- DMS:
-
Duckbill-type anti-reflux metal stent
- ENBD:
-
Endoscopic nasobiliary drainage
- NSAIDs:
-
Nonsteroidal anti-inflammatory drugs
- TRBO:
-
Time to recurrent biliary obstruction
- AE:
-
Adverse event
- OS:
-
Overall survival
- ECOG:
-
Eastern Cooperative Oncology Group
- PS:
-
Performance status
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
References
Almadi MA, Barkun A, Martel M (2017) Plastic vs. self-expandable metal stents for palliation in malignant biliary obstruction: a series of meta-analyses. Am J Gastroenterol 112:260–273
Isayama H, Yasuda I, Ryozawa S, Maguchi H, Igarashi Y, Matsuyama Y, Katanuma A, Hasebe O, Irisawa A, Itoi T, Mukai H, Arisaka Y, Okushima K, Uno K, Kida M, Tamada K (2011) Results of a Japanese multicenter, randomized trial of endoscopic stenting for non-resectable pancreatic head cancer (JM-test): covered wallstent versus doublelayer stent. Dig Endosc 23:310–315
Nakai Y, Isayama H, Wang HP, Rerknimitr R, Khor C, Yasuda I, Kogure H, Moon JH, Lau J, Lakhtakia S, Ratanachu-Ek T, Seo DW, Lee DK, Makmun D, Dy F, Liao WC, Draganov PV, Almadi M, Irisawa A, Katanuma A, Kitano M, Ryozawa S, Fujisawa T, Wallace MB, Itoi T, Devereaux B (2020) International consensus statements for endoscopic management of distal biliary stricture. J Gastroenterol Hepatol 35:967–979
Tringali A, Hassan C, Rota M, Rossi M, Mutignani M, Aabakken L (2018) Covered vs. uncovered self-expandable metal stents for malignant distal biliary strictures: a systematic review and meta-analysis. Endoscopy 50:631–641
Hamada T, Isayama H, Nakai Y, Togawa O, Kogure H, Kawakubo K, Tsujino T, Sasahira N, Hirano K, Yamamoto N, Arizumi T, Ito Y, Matsubara S, Sasaki T, Yagioka H, Yashima Y, Mohri D, Miyabayashi K, Mizuno S, Nagano R, Takahara N, Toda N, Tada M, Omata M, Koike K (2011) Duodenal invasion is a risk factor for the early dysfunction of biliary metal stents in unresectable pancreatic cancer. Gastrointest Endosc 74:548–555
Hamada T, Nakai Y, Isayama H, Sasaki T, Kogure H, Kawakubo K, Sasahira N, Yamamoto N, Togawa O, Mizuno S, Ito Y, Hirano K, Toda N, Tada M, Koike K (2013) Duodenal metal stent placement is a risk factor for biliary metal stent dysfunction: an analysis using a time-dependent covariate. Surg Endosc 27:1243–1248
Togawa O, Isayama H, Tsujino T, Nakai Y, Kogure H, Hamada T, Sasaki T, Yashima Y, Yagioka H, Arizumi T, Ito Y, Matsubara S, Yamamoto N, Sasahira N, Hirano K, Toda N, Tada M, Koike K (2013) Management of dysfunctional covered self-expandable metallic stents in patients with malignant distal biliary obstruction. J Gastroenterol 48:1300–1307
Ornellas LC, Stefanidis G, Chuttani R, Gelrud A, Kelleher TB, Pleskow DK (2009) Covered Wallstents for palliation of malignant biliary obstruction: primary stent placement versus reintervention. Gastrointest Endosc 70:676–683
Misra SP, Dwivedi M (2009) Reflux of duodenal contents and cholangitis in patients undergoing self-expanding metal stent placement. Gastrointest Endosc 70:317–321
Hu B, Wang TT, Shi ZM, Wang SZ, Lu R, Pan YM, Huang H, Wang SP (2011) A novel antireflux metal stent for the palliation of biliary malignancies: a pilot feasibility study (with video). Gastrointest Endosc 73:143–148
Lee KJ, Chung MJ, Park JY, Lee DH, Jung S, Bang BW, Park SW, Chung JB, Song SY, Bang S (2013) Clinical advantages of a metal stent with an S-shaped anti-reflux valve in malignant biliary obstruction. Dig Endosc 25:308–312
Kim DU, Kwon CI, Kang DH, Ko KH, Hong SP (2013) New antireflux self-expandable metal stent for malignant lower biliary obstruction: in vitro and in vivo preliminary study. Dig Endosc 25:60–66
Hu B, Wang TT, Wu J, Shi ZM, Gao DJ, Pan YM (2014) Antireflux stents to reduce the risk of cholangitis in patients with malignant biliary strictures: a randomized trial. Endoscopy 46:120–126
Lee YN, Moon JH, Choi HJ, Choi MH, Lee TH, Cha SW, Cho YD, Choi SY, Lee HK, Park SH (2016) Effectiveness of a newly designed antireflux valve metal stent to reduce duodenobiliary reflux in patients with unresectable distal malignant biliary obstruction: a randomized, controlled pilot study (with videos). Gastrointest Endosc 83:404–412
Hamada T, Isayama H, Nakai Y, Iwashita T, Ito Y, Mukai T, Yagioka H, Saito T, Togawa O, Ryozawa S, Hirano K, Mizuno S, Yamamoto N, Kogure H, Yasuda I, Koike K (2019) Antireflux covered metal stent for nonresectable distal malignant biliary obstruction: multicenter randomized controlled trial. Dig Endosc 31:566–574
Kin T, Ishii K, Okabe Y, Itoi T, Katanuma A (2020) Feasibility of biliary stenting to distal malignant biliary obstruction using a novel designed metal stent with duckbill-shaped anti-reflux valve. Dig Endosc. https://doi.org/10.1111/den.13827
Renno A, Abdel-Aziz Y, Ahmed T, Alastal Y, Toseef J, Al-Abboodi Y, Nawras A (2019) Antireflux valve metal stent versus conventional self-expandable metal stent in distal malignant biliary obstruction: a systematic review and meta-analysis. Ann Gastroenterol 32:605–613
Yamada Y, Sasaki T, Takeda T, Mie T, Furukawa T, Kasuga A, Matsuyama M, Ozaka M, Igarashi Y, Sasahira N (2021) A novel laser-cut fully covered metal stent with anti-reflux valve in patients with malignant distal biliary obstruction refractory to conventional covered metal stent. J Hepatobiliary Pancreat Sci 28:563–571
Isayama H, Hamada T, Yasuda I, Itoi T, Ryozawa S, Nakai Y, Kogure H, Koike K (2015) TOKYO criteria 2014 for transpapillary biliary stenting. Dig Endosc 27:259–264
Cotton PB, Eisen GM, Aabakken L, Baron TH, Hutter MM, Jacobson BC, Mergener K, Nemcek A Jr, Petersen BT, Petrini JL, Pike IM, Rabeneck L, Romagnuolo J, Vargo JJ (2010) A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc 71:446–454
Japanese Gastric Cancer Association (1998) Japanese Classification of Gastric Carcinoma - 2nd English Edition. Gastric Cancer: Official Journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association 1:10–24
Dutz A, Löck S (2019) Competing risks in survival data analysis. Radiother Oncol 130:185–189
Gray RJ (1988) A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 16(1141–1154):1114
Kanda Y (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transpl 48:452–458
Kida M, Miyazawa S, Iwai T, Ikeda H, Takezawa M, Kikuchi H, Watanabe M, Imaizumi H, Koizumi W (2011) Endoscopic management of malignant biliary obstruction by means of covered metallic stents: primary stent placement vs. re-intervention. Endoscopy 43:1039–1044
Nakai Y, Isayama H, Kogure H, Hamada T, Togawa O, Ito Y, Matsubara S, Arizumi T, Yagioka H, Mizuno S, Sasaki T, Yamamoto N, Hirano K, Tada M, Koike K (2014) Risk factors for covered metallic stent migration in patients with distal malignant biliary obstruction due to pancreatic cancer. J Gastroenterol Hepatol 29:1744–1749
Kwon CI, Moon JP, Yun H, Jeong S, Koh DH, Lee WJ, Ko KH, Kang DH (2018) Evaluation of valve function in antireflux biliary metal stents. BMC Gastroenterol 18:150
Mandai K, Nakamura S, Uno K, Yasuda K (2021) Successful re-intervention through stent mesh after novel antireflux covered metal biliary stent placement. Endoscopy 53:E94-e95
Funding
The authors received no specific funding for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Dr. Takashi Sasaki received honoraria from Kawasumi Laboratories, Boston Scientific Japan, Century Medical, Cook Japan. Dr. Naoki Sasahira received honoraria from Boston Scientific, Gadelius Medical, Kawasumi Laboratories. Drs. Tsuyoshi Takeda, Yuto Yamada, Takeshi Okamoto, Takafumi Mie, Takaaki Furukawa, Akiyoshi Kasuga, Masato Matsuyama, Masato Ozaka have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Takeda, T., Sasaki, T., Yamada, Y. et al. Long-term outcomes of duckbill-type anti-reflux metal stents versus conventional covered metal stents in reinterventions after covered biliary metal stent dysfunction in unresectable pancreatic cancer. Surg Endosc 37, 3498–3506 (2023). https://doi.org/10.1007/s00464-022-09836-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09836-0