Abstract
Purpose
To compare clinical outcomes for open, laparoscopic, and robotic hernia repairs for direct, unilateral inguinal hernia repairs, with particular focus on 30-day morbidity surgical site infection (SSI); surgical site occurrence (SSO); SSI/SSO requiring procedural interventions (SSOPI), reoperation, and recurrence.
Methods
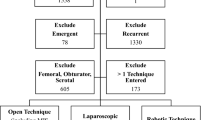
The Abdominal Core Health Quality Collaborative database was queried for patients undergoing elective, primary, > 3 cm medial, unilateral inguinal hernia repairs with an open (Lichtenstein), laparoscopic, or robotic operative approach. Preoperative demographics and patient characteristics, operative techniques, and outcomes were studied. A 1-to-1 propensity score matching algorithm was used for each operative approach pair to reduce selection bias.
Results
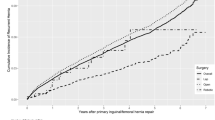
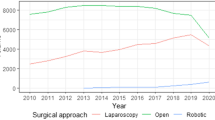
There were 848 operations included: 297 were open, 285 laparoscopic, and 266 robotic hernia repairs. There was no evidence of a difference in primary endpoints at 30 days including SSI, SSO, SSI/SSO requiring procedural interventions (SSOPI), reoperation, readmission, or recurrence for any of the operative approach pairs (open vs. robotic, open vs. laparoscopic, robotic vs. laparoscopic). For the open vs. laparoscopic groups, QoL score at 30 day was lower (better) for laparoscopic surgery compared to open surgery (OR 0.53 [0.31, 0.92], p = 0.03), but this difference did not hold at the 1-year survey (OR 1.37 [0.48, 3.92], p = 0.55). Similarly, patients who underwent robotic repair were more likely to have a higher (worse) 30-day QoL score (OR 2.01 [1.18, 3.42], p = 0.01), but no evidence of a difference at 1 year (OR 0.83 [0.3, 2.26] p = 0.71).
Conclusions
Our study did not reveal significant post-operative outcomes between open, laparoscopic, and robotic approaches for large medial inguinal hernias. Surgeons should continue to tailor operative approach based on patient needs and their own surgical expertise.



Similar content being viewed by others
References
Tran H (2018) Endorsement of the herniasurge guidelines by the Australasian hernia society. Hernia 22(1):177. https://doi.org/10.1007/s10029-017-1673-0
AlMarzooqi R, Tish S, Huang LC et al (2019) Review of inguinal hernia repair techniques within the Americas hernia society quality collaborative. Hernia 23(3):429–438. https://doi.org/10.1007/s10029-019-01968-y
Luijendijk RW, Hop WC, van den Tol MP et al (2000) A comparison of suture repair with mesh repair for incisional hernia. N Engl J Med 343(6):392–398. https://doi.org/10.1056/NEJM200008103430603
Heniford T, Park A, Ramshaw BJ et al (2000) Laparoscopic ventral and incisional hernia repair in 407 patients. J Am Coll Surg 190(6):645–650. https://doi.org/10.1016/s1072-7515(00)00280-5
Heniford BT, Park A, Ramshaw BJ et al (2003) Laparoscopic repair of ventral hernias: nine years’ experience with 850 consecutive hernias. Ann Surg 238(3):391–399. https://doi.org/10.1097/01.sla.0000086662.49499.ab
Holleran TJ, Napolitano MA, Sparks AD et al (2022) Trends and outcomes of open, laparoscopic, and robotic inguinal hernia repair in the veterans affairs system. Hernia 26(3):889–899. https://doi.org/10.1007/s10029-021-02419-3
Sheetz KH, Claflin J, Dimick JB (2020) Trends in the adoption of robotic surgery for common surgical procedures. JAMA Netw Open 3(1):e1918911. https://doi.org/10.1001/jamanetworkopen.2019.18911
Awad MA, Buzalewski J, Anderson C et al (2020) Robotic inguinal hernia repair outcomes: operative time and cost analysis. JSLS. https://doi.org/10.4293/JSLS.2020.00058
Poulose BK, Roll S, Murphy JW et al (2016) Design and implementation of the Americas hernia society quality collaborative (AHSQC): improving value in hernia care. Hernia 20(2):177–189. https://doi.org/10.1007/s10029-016-1477-7
Muysoms F, Campanelli G, Champault GG et al (2012) EuraHS: the development of an international online platform for registration and outcome measurement of ventral abdominal wall hernia repair. Hernia 16(3):239–250. https://doi.org/10.1007/s10029-012-0912-7
Muysoms FE, Vanlander A, Ceulemans R et al (2016) A prospective, multicenter, observational study on quality of life after laparoscopic inguinal hernia repair with ProGrip laparoscopic, self-fixating mesh according to the European registry for abdominal wall hernias quality of life instrument. Surgery 160(5):1344–1357. https://doi.org/10.1016/j.surg.2016.04.026
Tastaldi L, Barros PHF, Krpata DM et al (2020) Hernia recurrence inventory: inguinal hernia recurrence can be accurately assessed using patient-reported outcomes. Hernia 24(1):127–135. https://doi.org/10.1007/s10029-019-02000-z
Kim HY (2017) Statistical notes for clinical researchers: chi-squared test and fisher’s exact test. Restor Dent Endod 42(2):152–155. https://doi.org/10.5395/rde.2017.42.2.15
Kim HY (2014) Statistical notes for clinical researchers: nonparametric statistical methods: 1. nonparametric methods for comparing two groups. Restor Dent Endod 39(3):235–239. https://doi.org/10.5395/rde.2014.39.3.235
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res 46(3):399–424. https://doi.org/10.1080/00273171.2011.568786
Wu JJ, Way JA, Eslick DD et al (2018) Transabdominal pre-peritoneal versus open repair for primary unilateral inguinal hernia: a meta-analysis. World J Surg 42(5):1304–1311. https://doi.org/10.1007/s00268-017-4288-9
Aiolfi A, Cavalli M, Micheletto G et al (2019) Primary inguinal hernia: systematic review and Bayesian network meta-analysis comparing open, laparoscopic transabdominal preperitoneal, totally extraperitoneal, and robotic preperitoneal repair. Hernia 23(3):473–484. https://doi.org/10.1007/s10029-019-01964-2
Tatarian T, Nie L, McPartland C et al (2021) Comparative perioperative and 5-year outcomes of robotic and laparoscopic or open inguinal hernia repair: a study of 153,727 patients in the state of New York. Surg Endosc 35(12):7209–7218. https://doi.org/10.1007/s00464-020-08211-1
Acknowledgements
None.
Author information
Authors and Affiliations
Contributions
All authors contributed significantly to the work. The study was designed by RZ, and data primarily obtained by MO and RZ. Data analysis and interpretation were done by all authors. Manuscript preparation was primarily done by DNV, MS, and RZ, with all authors contributing to the draft and revisions to ensure accuracy of the data and analysis.
Corresponding author
Ethics declarations
Disclosures
Authors Dimitrios N. Varvoglis, Manuel Sanchez-Casalongue, Molly A. Olson, Noah DeAngelo, Ian Garbarine, Jeffrey Lipman, Timothy M. Farrell, Wayne David Overby, Arielle Perez, and Randal Zhou have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Varvoglis, D.N., Sanchez-Casalongue, M., Olson, M.A. et al. Comparison of post-operative outcomes of large direct inguinal hernia repairs based on operative approach (open vs. laparoscopic vs. robotic) using the ACHQC (Abdominal Core Health Quality Collaborative) database. Surg Endosc 37, 2923–2931 (2023). https://doi.org/10.1007/s00464-022-09805-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09805-7