Abstract
Background
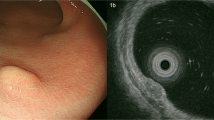
Endoscopic submucosal dissection (ESD) has been widely adopted in treating rectal neuroendocrine tumors (NETs). However, clinical outcomes in rectal NETs after ESD with different resection margin status remain scanty, particularly in patients with positive resection margins. This study aimed to evaluate the long-term clinical outcomes of ESD in rectal NET based on the resection margin status.
Methods
This retrospective study included 436 patients diagnosed with rectal NET who had undergone ESD. Clinical data, including age, sex, tumor size, stage, invasion, and the resection margin status, were collected. Further, the patients were assessed for complications, recurrence, distant metastasis, and long-term outcomes.
Results
Among all 436 patients, 395 patients had their primary ESD in our hospital. Complete resection was achieved in 319 patients. Patients who did not achieve complete resection opted for follow-up (n = 73), salvage surgery (n = 1) and salvage ESD (n = 2). Another 41 had their primary ESD in other hospital with incomplete resection and had salvage ESD in our hospital. All 436 patients had a median follow-up period of 61.4 months (range 33.4–125.3 months). During the follow-up period, two patients developed recurrences, while three patients developed metastasis. There were no significant differences in the 5-year progression-free survival and overall survival between patients with incomplete resection opting for follow-up compared to the other two groups (P = 0.5/0.8). However, the complication rates were significantly higher in patients who received salvage ESD.
Conclusion
This study demonstrated that positive resection margins have no influence on survival in patients with rectal NET treated using ESD.



Similar content being viewed by others
References
Cives M, Strosberg JR (2018) Gastroenteropancreatic neuroendocrine tumors. CA Cancer J Clin 68(6):471–487
Dasari A, Shen C, Halperin D et al (2017) Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol 3(10):1335–1342
Huguet I, Grossman AB, O’Toole D (2016) Changes in the epidemiology of neuroendocrine tumours. Neuroendocrinology 104(2):105–111
Basuroy R, O’Donnell CM, Srirajaskanthan R, Ramage JK (2018) Ileocolonic neuroendocrine tumours identified in the English bowel cancer screening programme. Color Dis 20(4):O85–O91
Boyar Cetinkaya R, Aagnes B, Myklebust TÅ, Thiis-Evensen E (2018) Survival in neuroendocrine neoplasms; a report from a large Norwegian population-based study. Int J Cancer 142(6):1139–1147
de Mestier L, Lorenzo D, Fine C et al (2019) Endoscopic, transanal, laparoscopic, and transabdominal management of rectal neuroendocrine tumors. Best Pract Res Clin Endocrinol Metab 33(5):101293
Chen L, Guo Y, Zhang Y et al (2021) Development of a novel scoring system based on endoscopic appearance for management of rectal neuroendocrine tumors. Endoscopy 53(07):702–709
Ramage JK, Valle JW, Nieveen van Dijkum EJM et al (2019) Colorectal neuroendocrine neoplasms: areas of unmet need. Neuroendocrinology 108(1):45–53
Basuroy R, Haji A, Ramage JK, Quaglia A, Srirajaskanthan R (2016) Review article: the investigation and management of rectal neuroendocrine tumours. Aliment Pharmacol Ther 44(4):332–345
Ramage JK, De Herder WW, Delle Fave G et al (2016) ENETS consensus guidelines update for colorectal neuroendocrine neoplasms. Neuroendocrinology 103(2):139–143
Qi ZP, Shi Q, Liu JZ et al (2018) Efficacy and safety of endoscopic submucosal dissection for submucosal tumors of the colon and rectum. Gastrointest Endosc 87(2):540-548.e1
Bosman FT, Carneiro F, Hruban RH et al (2010) WHO classification of tumours of the digestive system. IARC, Lyon
Amin MB, Greene FL, Edge SB et al (2017) The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin 67(2):93–99
Kumar AS, Sidani SM, Kolli K et al (2012) Transanal endoscopic microsurgery for rectal carcinoids: the largest reported United States experience. Color Dis 14(5):562–566
Fields AC, Saadat LV, Scully RE et al (2019) Local excision versus radical resection for 1-To 2-cm neuroendocrine tumors of the rectum: a national cancer database analysis. Dis Colon Rectum 62(4):417–421
Modlin IM, Lye KD, Kidd M (2003) A 5-decade analysis of 13,715 carcinoid tumors. Cancer 97(4):934–959
McConnell YJ (2016) Surgical management of rectal carcinoids: Trends and outcomes from the Surveillance, epidemiology, and end results database (1988 to 2012). Am J Surg 211(5):877–885
Saito Y, Sakamoto T, Nakajima T, Matsuda T (2014) Colorectal ESD: current indications and latest technical advances. Gastrointest Endosc Clin N Am 24(2):245–255
Choi HH (2013) Which endoscopic treatment is the best for small rectal carcinoid tumors? World J Gastrointest Endosc 5(10):487
Onozato Y, Kakizaki S, Iizuka H, Sohara N, Mori M, Itoh H (2010) Endoscopic treatment of rectal carcinoid tumors. Dis Colon Rectum 53(2):169–176
Moon CM, Huh KC, Jung SA et al (2016) Long-term clinical outcomes of rectal neuroendocrine tumors according to the pathologic status after initial endoscopic resection: A KASID multicenter study. Am J Gastroenterol 111(9):1276–1285
Sung HY, Kim SW, Kang WK et al (2012) Long-term prognosis of an endoscopically treated rectal neuroendocrine tumor: 10-year experience in a single institution. Eur J Gastroenterol Hepatol 24(8):978–983
Chen T, Yao LQ, Xu MD et al (2016) Efficacy and safety of endoscopic submucosal dissection for colorectal carcinoids. Clin Gastroenterol Hepatol 14(4):575–581
Gleeson FC, Levy MJ, Dozois EJ, Larson DW, Wong Kee Song LM, Boardman LA (2014) Endoscopically identified well-differentiated rectal carcinoid tumors: Impact of tumor size on the natural history and outcomes. Gastrointest Endosc 80(1):144–151
Shigeta K, Okabayashi K, Hasegawa H et al (2014) Long-term outcome of patients with locally resected high- and low-risk rectal carcinoid tumors. J Gastrointest Surg 18(4):768–773
Hane Y, Tsuchikawa T, Tanaka K et al (2020) Metachronous liver metastases after long-term follow-up of endoscopic resection for rectal neuroendocrine neoplasms: a report of three cases. Surg Case Reports 6(1):4–8
Sekiguchi M, Sekine S, Sakamoto T et al (2015) Excellent prognosis following endoscopic resection of patients with rectal neuroendocrine tumors despite the frequent presence of lymphovascular invasion. J Gastroenterol 50(12):1184–1189
Chen WJ, Wu N, Zhou JL, Le LG, Qiu HZ (2015) Full-thickness excision using transanal endoscopic microsurgery for treatment of rectal neuroendocrine tumors. World J Gastroenterol 21(30):9142–9149
Park CH, Cheon JH, Kim JO et al (2011) Criteria for decision making after endoscopic resection of well-differentiated rectal carcinoids with regard to potential lymphatic spread. Endoscopy 43(9):790–795
Yamamoto K, Shimoda R, Ogata S et al (2018) Perforation and postoperative bleeding associated with endoscopic submucosal dissection in colorectal tumors: an analysis of 398 lesions treated in saga. Japan Intern Med 57(15):2115–2122
Okamoto K, Watanabe T, Komeda Y et al (2017) Risk factors for postoperative bleeding in endoscopic submucosal dissection of colorectal tumors. Oncol 93(1):35–42
Hong SN, Byeon JS, Lee BI et al (2016) Prediction model and risk score for perforation in patients undergoing colorectal endoscopic submucosal dissection. Gastrointest Endosc 84(1):98–108
Kaosombatwattana U, Yamamura T, Limsrivilai J et al (2019) Preoperative endoscopic predictors of severe submucosal fibrosis in colorectal tumors undergoing endoscopic submucosal dissection. Endosc Int Open 07(04):E421–E430
Takamaru H, Goto R, Yamada M, Sakamoto T, Matsuda T, Saito Y (2020) Expert review of medical devices predicting and managing complications following colonoscopy : risk factors and management of advanced interventional endoscopy with a focus on colorectal ESD. Expert Rev Med Devices 00(00):1–8
Kunz PL, Reidy-Lagunes D, Anthony LB et al (2013) Consensus guidelines for the management and treatment of neuroendocrine tumors. Pancreas 42(4):557–577
Shah MH, Goldner WS, Halfdanarson TR et al (2018) NCCN guidelines insights: neuroendocrine and adrenal tumors. J Natl Compr Cancer Netw. 16(6):693–702
Funding
This work was supported by the National Key R&D Program of China (No.2019YFC1315800/2019YFC1315802), National Natural Science Foundation of China (No. 81902394, 82002515, 81502000), Shanghai Sailing Program (No.20YF1407200), China Postdoctoral Science Foundation (No. 2020M681177), and Shanghai Municipal Commission of Science and Technology (NO. 19140901902, 18DZ1930302, 22S31903800).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Disclosure
Drs. Di Sun, Zhong Ren, Enpan Xu, Shilun Cai, Zhipeng Qi, Zhanghan Chen, Jingyi Liu, Qiang Shi, Pinghong Zhou, Yunshi Zhong have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sun, D., Ren, Z., Xu, E. et al. Long-term clinical outcomes of endoscopic submucosal dissection in rectal neuroendocrine tumors based on resection margin status: a real-world study. Surg Endosc 37, 2644–2652 (2023). https://doi.org/10.1007/s00464-022-09710-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09710-z