Abstract
Introduction
Robotic surgery has integrated into the healthcare system despite limited evidence demonstrating its clinical benefit. Our objectives were (i) to describe secular trends and (ii) patient- and system-level determinants of the receipt of robotic as compared to open or laparoscopic surgery.
Methods
This population-based retrospective cohort study included adult patients who, between 2009 and 2018 in Ontario, Canada, underwent one of four commonly performed robotic procedures: radical prostatectomy, total hysterectomy, thoracic lobectomy, partial nephrectomy. Patients were categorized based on the surgical approach as robotic, open, or laparoscopic for each procedure. Multivariable regression models were used to estimate the temporal trend in robotic surgery use and associations of patient and system characteristics with the surgical approach.
Results
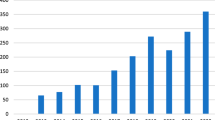
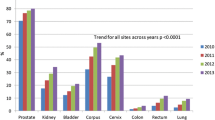
The cohort included 24,741 radical prostatectomy, 75,473 total hysterectomy, 18,252 thoracic lobectomy, and 4608 partial nephrectomy patients, of which 6.21% were robotic. After adjusting for patient and system characteristics, the rate of robotic surgery increased by 24% annually (RR 1.24, 95%CI 1.13–1.35): 13% (RR 1.13, 95%CI 1.11–1.16) for robotic radical prostatectomy, 9% (RR 1.09, 95%CI 1.05–1.13) for robotic total hysterectomy, 26% (RR 1.26, 95%CI 1.06–1.50) for thoracic lobectomy and 26% (RR 1.26, 95%CI 1.13–1.40) for partial nephrectomy. Lower comorbidity burden, earlier disease stage (among cancer cases), and early career surgeons with high case volume at a teaching hospital were consistently associated with the receipt of robotic surgery.
Conclusion
The use of robotic surgery has increased. The study of the real-world clinical outcomes and associated costs is needed before further expanding use among additional providers and hospitals.


Similar content being viewed by others
References
Muaddi H, Hafid ME, Choi WJ et al (2021) Clinical outcomes of robotic surgery compared to conventional surgical approaches (laparoscopic or open): a systematic overview of reviews. Ann Surg 273(3):467–473. https://doi.org/10.1097/SLA.0000000000003915
Marohn MR, Hanly EJ (2004) Twenty-first century surgery using twenty-first century technology: surgical robotics. Curr Surg 61(5):466–473
Sheetz KH, Claflin J, Dimick JB (2020) Trends in the adoption of robotic surgery for common surgical procedures. JAMA Netw Open 3(1):e1918911. https://doi.org/10.1001/jamanetworkopen.2019.18911
Health Quality Ontario (2017) Robotic surgical system for radical prostatectomy: a health technology assessment. ON Health Technol Assess Ser 17(11):1–172
Agence d’évaluation des technologies et des modes d’intervention en santé (AETMIS) (2010) La prostatectomie radicale assistée par robot [homepage on the Internet]. [cited April 2021]. https://www.inesss.qc.ca/fileadmin/doc/AETMIS/Rapports/Cancer/NI-2010-01_prostatectomie.pdf
Marcus HJ, Hughes-Hallett A, Payne CJ et al (2017) Trends in the diffusion of robotic surgery: a retrospective observational study. Int J Med Robotics Comput Assist Surg. 13(4):e1870
Pietrabissa A, Vinci A, Pugliese L, Peri A (2012) Robotic surgery: current controversies and future expectations. Cirugia española (English ed) 91(2):67–71. https://doi.org/10.1016/j.cireng.2012.07.002
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke J (2007) STROBE: annals of internal medicine academia and clinic the strengthening the reporting of observational studies in epidemiology (STROBE) statement : guidelines for reporting. Lancet. https://doi.org/10.1136/bmj.39335.541782.AD
Canadian Institute for Health Information. https://www.cihi.ca/en/about-cihi/contact-us.
Classification of Hospitals. Ottawa (ON). Ontario Ministry of Health and Long Term Care. www.health.gov.on.ca/english/public/contact/hosp/group_a.html. Accessed Feb 2020.
Ministry of Health and Long-Term Care (MOHLTC) in Ontario, Canada. Registered Persons Database (RPDB). https://data.ontario.ca/dataset/registered-persons-database-rpdb. Accessed Feb 2021.
Tu K, Campbell NR, Chen Z, Cauch-Dudek KJ, McAlister FA (2007) Accuracy of administrative databases in identifying patients with hypertension. Open Med 1(1):e18–e26
Kralj B (2000) Measuring ‘rurality’ for purposes of health-care planning: an empirical measure for Ontario. Ontario Medical Review
McLaughlin JR, Kreiger N, Marrett LD, Holowaty EJ (1991) Cancer incidence registration and trends in Ontario. Eur J Cancer 27(11):1520–1524. https://doi.org/10.1016/0277-5379(91)90041-b
Juurlink D, Preyra C, Croxford R, et al (2006) Canadian Institute for Health Information discharge abstract database: a validation study. Institute of Clinical Evaluative Sciences
Tu K, Chen Z, Lipscombe LL (2008) Canadian hypertension education program outcomes research taskforce: mortality among patients with hypertension from 1995 to 2005: a population-based study. CMAJ 178(11):1436–1440. https://doi.org/10.1503/cmaj.080096
Austin PC, Daly PA, Tu JV (2002) A multicenter study of the coding accuracy of hospital discharge administrative data for patients admitted to cardiac care units in Ontario. Am Heart J 144(2):290–296
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45(6):613–619
Simpson AN, Sutradhar R, Ferguson SE, Robertson D, Cheng SY, Baxter NN (2020) Class III obesity and other factors associated with longer wait times for endometrial cancer surgery: a population-based study. J Obstet Gynaecol Can 42(9):1093-1102.e3
Edge SB (2010) American Joint Committee on Cancer, American Cancer Society. AJCC cancer staging handbook: from the AJCC cancer staging manual, 7th ed. New York: Springer.
Glazier RH, Creatore MI, Agha MM, Steele LS (2003) Inner city Toronto time trends working group: socioeconomic misclassification in Ontario’s health care registry. Can J Public Health 94(2):140–143
Wilkins R (1993) Use of postal codes and addresses in the analysis of health data. Health Rep 5(2):157–177
Bollman RD, Clemenson HA (2008) Structure and change in Canada’s rural demography: an update to 2006. Rural and Small Town Canada Anal Bull. 7 (7 Ottawa: Statistics Canada, Cat. No. 21–006-XIE).
Canadian Journal of Health Technology. Robotic surgical systems for use in gynecologic oncology or urologic surgery: clinical effectiveness, cost-effectiveness, and guidelines. https://www.cadth.ca/sites/default/files/pdf/htis/2020/RB1430%20Robotic%20Surgical%20Systems%20Final.pdf. Accessed April 2021.
Papalekas E, Fisher J (2018) Trends in route of hysterectomy after the implementation of a comprehensive robotic training program. Minim Invasive Surg 2018:7362489. https://doi.org/10.1155/2018/7362489
Stitzenberg KB, Wong YN, Nielsen ME, Egleston BL, Uzzo RG (2012) Trends in radical prostatectomy: centralization, robotics, and access to urologic cancer care. Cancer 118(1):54–62. https://doi.org/10.1002/cncr.26274
Cusimano MC, Simpson AN, Dossa F et al (2019) Laparoscopic and robotic hysterectomy in endometrial cancer patients with obesity: a systematic review and meta-analysis of conversions and complications. Am J Obstet Gynecol 221(5):410-428.e19
Kneuertz PJ, D’Souza DM, Moffatt-Bruce SD, Merritt RE (2018) Robotic lobectomy has the greatest benefit in patients with marginal pulmonary function. J Cardiothorac Surg 13(1):56-z. https://doi.org/10.1186/s13019-018-0748-z
Sheetz KH, Dimick JB (2019) Is it time for safeguards in the adoption of robotic surgery? JAMA 321(20):1971–1972. https://doi.org/10.1001/jama.2019.3736
Levin L, Goeree R, Levine M et al (2011) Coverage with evidence development: the Ontario experience. Int J Technol Assess Health Care 27(2):159–168. https://doi.org/10.1017/S0266462311000018
Elrod JK, Fortenberry JL (2017) Centers of excellence in healthcare institutions: what they are and how to assemble them. BMC Health Serv Res 17(Suppl 1):425-y. https://doi.org/10.1186/s12913-017-2340-y
Funding
This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The parts of this material are based on the data and information compiled and provided by: MOHLTC, CCO and CIHI. The analyses, conclusions, opinions and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred. This study was supported by the Surgical Innovation Program at the Ontario Ministry of Health and Long-Term Care. H.M is support by CIHR Vanier award and the Physician Services Incorporated award.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Stephen E. Pautler is a mentor for Minogue Medical Inc and received no remuneration for this work. Waël C. Hanna is a speaker and consultant for Minogue medical and AstraZeneca, is a DMSB for Roche Genetech and has securities and stock with intuitive Surgical.
Authors Hala Muaddi, Therese A Stukel, Charles de Mestral, Avery Nathens, Bobby Shayegan, Christopher M Schlachta, Rodney H. Breau, Laura Hopkins, Timothy D. Jackson, Paul J Karanicolas have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Muaddi, H., Stukel, T.A., de Mestral, C. et al. The evolving use of robotic surgery: a population-based analysis. Surg Endosc 37, 1870–1877 (2023). https://doi.org/10.1007/s00464-022-09643-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09643-7