Abstract
Background
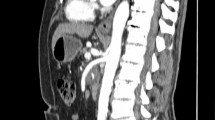
Performing a single-port laparoscopic pancreatectomy is technically challenging. Single-port laparoscopic pancreaticoduodenectomy (SPLPD) is rarely reported in English literature.
Methods
Eighty-seven cases of laparoscopic pancreaticoduodenectomy (LPD) were performed by a single surgical team in the Department of Pancreatic Surgery, West China Hospital, Sichuan University between February 2020 and December 2020. Among these, 13 cases of LPD (group 1) were performed using a single-port device. Basing on the same inclusion and exclusion criteria, 68 cases of LPD performed using traditional 5-trocar were included as a control group (group 2). The patient’s demographic characteristics, intraoperative, and postoperative variables were prospectively collected and retrospectively analyzed.
Results
Five men and eight women were included in the SPLPD group. The median age of these patients was 57 years. The patients who underwent SPLPD required a longer operative time (332.7 ± 38.1 min vs. 305.8 ± 64.7 min; p = 0.03) than those in the LPD group. The estimated blood loss, conversion rate, blood transfusion rate, time to oral intake, postoperative hospital stays, and perioperative complications were comparable between the two groups. The short-term oncological outcomes, such as R0 rate and lymph node harvested, were comparable between the two groups. The 90-day mortality of all patients was zero.
Conclusions
SPLPD is a safe and feasible procedure for well-selected patients in an experienced minimally invasive pancreatic surgery team. SPLPD may provide several potential advantages, such as the requirement of fewer trocars, fewer abdominal complications, and reduced participation of assistants than conventional LPD.


Similar content being viewed by others
References
Gagner M, Pomp A (1994) Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc 8(5):408–410
Chen K, Zhou Y, Jin W, Zhu Q, Lu C, Niu N, Wang Y, Mou Y, Chen Z (2019) Laparoscopic pancreaticoduodenectomy versus open pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: oncologic outcomes and long-term survival. Surg Endosc 34:1948
Zhang H, Lan X, Peng B, Li B (2019) Is total laparoscopic pancreaticoduodenectomy superior to open procedure? A meta-analysis. World J Gastroenterol 25(37):5711–5731
Benzing C, Krenzien F, Atanasov G, Seehofer D, Sucher R, Zorron R, Pratschke J, Schmelzle M (2015) Single incision laparoscopic liver resection (SILL) - a systematic review. GMS Interdiscip Plast Reconstr Surg DGPW 4:17
Arezzo A, Passera R, Bullano A, Mintz Y, Kedar A, Boni L, Cassinotti E, Rosati R, Fumagalli Romario U, Sorrentino M et al (2017) Multi-port versus single-port cholecystectomy: results of a multi-centre, randomised controlled trial (MUSIC trial). Surg Endosc 31(7):2872–2880
Cai Y, Luo H, Li Y, Gao P, Peng B (2019) A novel technique of pancreaticojejunostomy for laparoscopic pancreaticoduodenectomy. Surg Endosc 33(5):1572–1577
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M, Allen P, Andersson R, Asbun HJ, Besselink MG et al (2017) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery 161(3):584–591
Wente MN, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Traverso LW et al (2007) Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 142(5):761–768
Choi YS, Shin KS, Choi J, Park JN, Oh YS, Rhee TE (2012) Single-port access laparoscopy-assisted vaginal hysterectomy: our initial experiences with 100 cases. Minim Invasive Surg 2012:543627
Marescaux J, Dallemagne B, Perretta S, Wattiez A, Mutter D, Coumaros D (2007) Surgery without scars: report of transluminal cholecystectomy in a human being. Arch Surg 142(9):823–826
Subirana H, Rey FJ, Barri J, Robres J, Parra L, Martin M, Memba R, Mullerat JM, Jorba R (2020) Single-incision versus four-port laparoscopic cholecystectomy in an ambulatory surgery setting: a prospective randomised double-blind controlled trial. J Min Access Surg 17:311
Lee Y, Kim HH (2017) Single-incision laparoscopic gastrectomy for gastric cancer. J Gastr Cancer 17(3):193–203
Hebbar M, Riaz W, Sains P, Baig MK, Sajid MS (2018) Meta-analysis of randomized controlled trials only exploring the role of single incision laparoscopic surgery versus conventional multiport laparoscopic surgery for colorectal resections. Transl Gastroenterol Hepatol 3:30
Wang YB, Xia J, Zhang JY, Gong JP, Wang XM (2017) Effectiveness and safety of single-port versus multi-port laparoscopic surgery for treating liver diseases: a meta-analysis. Surg Endosc 31(4):1524–1537
Park P, Han HJ, Song TJ, Choi SB, Kim WB, Yoo YD, Kim DS, Cha JH (2019) Single-port versus conventional laparoscopic distal pancreatectomy: a propensity score matched analysis and a learning curve of single-port approach. J Hepatobiliary Pancreat Sci 26(9):401–409
Park G, Choi SH, Lee JH, Lim JH, Lee H, Lee JH, Kang CM (2020) Safety and feasibility of robotic reduced-port distal pancreatectomy: a multicenter experience of a novel technique. J Gastrointest Surg 24(9):2015–2020
Funding
This study was funded by National Institutes of Health of China (W2017ZWS07).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Pan Gao, He Cai, Bing Peng, and Yunqiang Cai have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gao, P., Cai, H., Peng, B. et al. Single-port laparoscopic pancreaticoduodenectomy. Surg Endosc 37, 1166–1172 (2023). https://doi.org/10.1007/s00464-022-09618-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09618-8