Abstract
Background
Achalasia is a rare disorder of esophageal motility that induces progressive intolerance to oral intake. Other esophageal dysmotility disorders include esophagogastric junction outflow obstruction (EGJOO), distal esophageal spasm (DES), hypercontractile esophagus (HE), and other minor disorders of peristalsis (MDP) and can present similarly to achalasia despite different pathophysiologies. Prior studies have demonstrated the safety and efficacy of POEM in the treatment of achalasia, but little is reported regarding POEM’s role in treating non-achalasia esophageal dysmotility disorders (NAEDD). This study aims to assess the safety and efficacy of POEM in the treatment of NAEDD.
Study design
This is a retrospective review of consecutive POEM cases from June 1, 2011, to February 1, 2021. NAEDD were characterized according to the Chicago classification. Primary outcome measure was the resolution of preoperative symptoms. Secondary outcomes include preoperative diagnosis, myotomy length, conversion to laparoscopic or open procedure, operative time, and length of stay (LOS). Technical success was defined as the completion of an 8 cm myotomy including the esophagogastric junction (EGJ) and extending 2 cm distal to the EGJ. Clinical success was defined as a postoperative Eckardt score ≤ 3.
Results
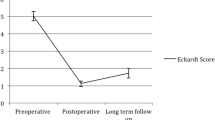
Of 124 cases of POEM performed during the study period, 17 were performed for NAEDD. Technical success was achieved in all 17 patients (100%). Of the fifteen patients that had documented postoperative Eckardt scores, 13 were ≤ 3, achieving a clinical success rate of 87%. Subgroup analysis (HE/MDP/DES vs. EGJOO) showed no significant differences in the preoperative or postoperative Eckardt scores between groups, and both groups demonstrated a significant decrease in Eckardt scores after POEM. No cases were aborted for technical or clinical reasons, and there were no adverse outcomes.
Conclusion
POEM is a safe and efficacious treatment modality for NAEDD. Further work is needed to develop optimal treatment strategies for this complex group of diseases.
Graphical abstract


Similar content being viewed by others
References
Sadowski DC, Ackah F, Jiang B, Svenson LW (2010) Achalasia: Incidence, prevalence, and survival. A population-based study. Neurogastroenterol Motil 22:256–261
Eckardt AJ, Eckardt VF (2011) Treatment and surveillance strat- egies in achalasia: an update. Nat Rev Gastroenterol Hepatol 8:311–319
Ehlers AP, Oelschlager BK, Pellegrini CA, Wright AS, Saunders MD, Flum DR, He H, Farjah F (2017) Achalasia treatment, outcomes, utilization, and costs: a population-based study from the United States. J Am Coll Surg 225:380–386
Cheng JW, Li Y, Xing WQ, Ly HW, Wang HR (2017) Laparoscopic Heller myotomy is not superior to pneumatic dilation in the management of primary achalasia: conclusions of a systematic review and meta-analysis of randomized controlled trials. Medicine 96:e5525
Schlottmann F, Patti MG (2018) Esophageal achalasia: current diagnosis and treatment. Expert Rev Gastroenterol Hepatol 12(7):711–721
Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, Satodate H, Odaka N, Itoh H, Kudo S (2010) Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 42:265–271
Inoue H, Sato H, Ikeda H, Onimaru M, Sato C, Minami H, Yokomichi H, Kobayashi Y, Grimes KL, Kudo SE (2015) Per-oral endoscopic myotomy: a series of 500 patients. J Am Coll Surg 221:256–264
Park CH, Jung DH, Kim DH, Lim CH, Moon HS, Park JH, Jung HK, Hong SJ, Choi SC, Lee OY (2019) Comparative efficacy of per-oral endoscopic myotomy and Heller myotomy in patients with achalasia: a meta-analysis. Gastrointest endosc 90(4):546–558
Sanaka MR, Hayat U, Thota PN, Jegadeesan R, Ray M, Gabbard SL, Wadhwa N, Lopez R, Baker ME, Murthy S, Raja S (2016) Efficacy of peroral endoscopic myotomy vs other achalasia treatments in improving esophageal function observational study. World J Gastroenterol 22:4918–4925
Chandrasekhara V, Desilets D, Falk GW, Inoue H, Romanelli JR, Savides TJ, Stavropoulos SN, Swanstrom LL, (ASGE PIVI Committee) (2015) The American Society for Gastrointestinal Endoscopy PIVI (Preservation and Incorporation of Valuable Endoscopic Innovations) on peroral endoscopic myotomy. Gastrointest Endosc 81:1087–1099
Patel K, Abbassi-Ghadi N, Markar S, Kumar S, Jethwa P, Zaninotto G (2016) Peroral endoscopic myotomy for the treatment of esophageal achalasia: systematic review and pooled analysis. Dis Esoph 29:807–819
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, Pandolfino JE, International High Resolution Manometry Working Group (2015) The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 27(2):160–174
Yadlapati R, Kahrilas PJ, Fox MR, Bredenoord AJ, Prakash Gyawali C, Roman S, Babaei A, Mittal RK, Rommel N, Savarino E, Sifrim D, Smout A, Vaezi MF, Zerbib F, Akiyama J, Bhatia S, Bor S, Carlson DA, Chen JW, Cisternas D, Cock C, Coss-Adame E, de Bortoli N, Defilippi C, Fass R, Ghoshal UC, Gonlachanvit S, Hani A, Hebbard GS, Wook Jung K, Katz P, Katzka DA, Khan A, Kohn GP, Lazarescu A, Lengliner J, Mittal SK, Omari T, Park MI, Penagini R, Pohl D, Richter JE, Serra J, Sweis R, Tack J, Tatum RP, Tutuian R, Vela MF, Wong RK, Wu JC, Xiao Y, Pandolfino JE (2021) Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0©. Neurogastroenterol Motil 33(1):e14058
Bredenoord AJ, Fox M, Kahrilas PJ, Pandolfino JE, Schwizer W, Smout AJ, International High Resolution Manometry Working Group (2012) Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil 24(Suppl 1):57–65
Zerbib F, Roman S (2015) Current therapeutic options for esophageal motor disorders as defined by the Chicago classification. J Clin Gastroenterol 49:451–460
Drenth JP, Bos LP, Engels LG (1990) Efficacy of diltiazem in the treatment of diffuse oesophageal spasm. Aliment Pharmacol Ther 4:411–416
Vanuytsel T, Bisschops R, Farre R, Pauwels A, Holvoet L, Arts J, Caenepeel P, De Wulf D, Mimidis K, Rommel N, Tack J (2013) Botulinum toxin reduces dysphagia in patients with nonachalasia primary esophageal motility disorders. Clin Gastroenterol Hepatol 11:1115–1121
Eckardt VF, Aignherr C, Bernhard G (1992) Predictors of outcome in patients with achalasia treated by pneumatic dilation. Gastroenterology 103(6):1732–1738
R Core Team (2019) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria
Yang S, Zeng MS, Zhang ZY, Zhang HL, Liang L, Zhang XW (2015) Pneumomediastinum and pneumoperitoneum on computed tomography after peroral endoscopic myotomy (POEM): postoperative changes or complications? Acta Radiol 56(10):1216–1221
Ren Z, Zhong Y, Zhou P, Xu M, Cai M, Li L, Shi Q, Yao L (2012) Perioperative management and treatment for complications during and after peroral endoscopic myotomy (POEM) for esophageal achalasia (EA) (data from 119 cases). Surg Endosc 26(11):3267–3272
Bernardot L, Roman S, Barret M, Vitton V, Wallenhorst T, Pioche M, Chaussade S, Gonzalez JM, Ponchon T, Prat F, Barthet M, Vergniol J, Chabrun E, Zerbib F (2020) Efficacy of per-oral endoscopic myotomy for the treatment of non-achalasia esophageal motor disorders. Surg Endosc 34:5508–5515
Khashab MA, Familiari P, Draganov PV, Aridi HD, Cho JY, Ujiki M, Tinto RR, Louis H, Desai PN, Velanovich V, Albéniz E, Haji A, Marks J, Costamagna G, Devière J, Perbtani Y, Hedberg M, Estremera F, Del Campo LAM, Yang D, Bukhari M, Brewer O, Sanaei O, Fayad L, Agarwal A, Kumbhari V, Chen YI (2018) Peroral endoscopic myotomy is effective and safe in non-achalasia esophageal motility disorders: an international multicenter study. Endosc Int Open 6(8):E1031–E1036
Jacobs CC, Perbtani Y, Yang D, Al-Haddad MA, Obaitan I, Othman M, Groth S, Sethi A, Agarunov E, Repici A, Maselli R, Galtieri A, Moremen J, Jenkins HN, Samarasena JB, Chang KJ, Draganov PV (2021) Per-oral endoscopic myotomy for esophagogastric junction outflow obstruction: a multicenter pilot study. Clin Gastroenterol Hepatol 19(8):1717–1719
Li QL, Chen WF, Zhou PH, Yao LQ, Xu MD, Hu JW, Cai MY, Zhang YQ, Qin WZ, Ren Z (2013) Peroral endoscopic myotomy for the treatment of achalasia: a clinical comparative study of endoscopic full-thickness and circular muscle myotomy. J Am Coll Surg 217(3):442–451
Ahmed Y, Othman MO (2019) Peroral endoscopic myotomy (POEM) for achalasia. J Thorac Dis 11(Suppl 12):S1618–S1628
Samo S, Qayed E (2019) Esophagogastric junction outflow obstruction: where are we now in diagnosis and management? World J Gastroenterol 25(4):411–417
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
John R. Romanelli receives research funding from Davol, and consulting fees from New View Surgical. Timothy J. Morley, Matthew F. Mikulski, Matthew Rade, Jean Chalhoub, and David J. Desilets have no conflicts of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Morley, T.J., Mikulski, M.F., Rade, M. et al. Per-oral endoscopic myotomy for the treatment of non-achalasia esophageal dysmotility disorders: experience from a single high-volume center. Surg Endosc 37, 1013–1020 (2023). https://doi.org/10.1007/s00464-022-09596-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09596-x