Abstract
Background
The current study aimed to investigate the relationship between muscle mass proportion and the incidence of total complications in male gastric cancer (GC) patients after minimally invasive distal gastrectomy (MIDG).
Methods
Between March 2017 and March 2020, 152 male GC patients with clinical stage III or lower GC who underwent MIDG were enrolled in this study. The muscle mass ratio (MMR) was calculated by dividing the total muscle weight obtained from bioelectrical impedance analysis by the whole-body weight. Thereafter, the association between MMR and surgical outcomes was determined.
Results
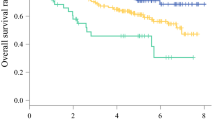
Based on the optimal MMR cutoff value of 0.712 obtained using the receiver operating characteristic (ROC) curve, patients were divided into two groups (69 and 83 patients in the MMR-L and MMR-H groups). The MMR-L group had a significantly higher total complication rate compared to the MMR-H group (MMR-L, 24.6% vs. MMR-H, 7.2%; P = 0.005). Multivariate analysis also identified MMR-L as a significant independent risk factor for total complications and intra-abdominal infectious complications after MIDG.
Conclusions
The MMR calculated using bioelectrical impedance analysis can be a useful predictor for postoperative complications after MIDG in male GC patients.


Similar content being viewed by others
References
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, Chou MY, Chen LY, Hsu PS, Krairit O, Lee JS, Lee WJ, Lee Y, Liang CK, Limpawattana P, Lin CS, Peng LN, Satake S, Suzuki T, Won CW, Wu CH, Wu SN, Zhang T, Zeng P, Akishita M, Arai H (2014) Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc 15:95–101
Pamoukdjian F, Bouillet T, Lévy V, Soussan M, Zelek L, Paillaud E (2018) Prevalence and predictive value of pre-therapeutic sarcopenia in cancer patients: a systematic review. Clin Nutr 37:1101–1113
Fukuda Y, Yamamoto K, Hirao M, Nishikawa K, Nagatsuma Y, Nakayama T, Tanikawa S, Maeda S, Uemura M, Miyake M, Hama N, Miyamoto A, Ikeda M, Nakamori S, Sekimoto M, Fujitani K, Tsujinaka T (2016) Sarcopenia is associated with severe postoperative complications in elderly gastric cancer patients undergoing gastrectomy. Gastric Cancer 19:986–993
Kawamura T, Makuuchi R, Tokunaga M, Tanizawa Y, Bando E, Yasui H, Aoyama T, Inano T, Terashima M (2018) Long-term outcomes of gastric cancer patients with preoperative sarcopenia. Ann Surg Oncol 25:1625–1632
Yamamoto K, Hirao M, Nishikawa K, Omori T, Yanagimoto Y, Shinno N, Sugimura K, Miyata H, Wada H, Takahashi H, Yasui M, Ohue M, Yano M, Fujitani K, Tsujinaka T (2019) Sarcopenia is associated with impaired overall survival after gastrectomy for elderly gastric cancer. Anticancer Res 39:4297–4303
Kanaya S, Haruta S, Kawamura Y, Yoshimura F, Inaba K, Hiramatsu Y, Ishida Y, Taniguchi K, Isogaki J, Uyama I (2011) Video: laparoscopy distinctive technique for suprapancreatic lymph node dissection: medial approach for laparoscopic gastric cancer surgery. Surg Endosc 25:3928–3929
Shibasaki S, Suda K, Nakauchi M, Nakamura T, Kadoya S, Kikuchi K, Inaba K, Uyama I (2018) Outermost layer-oriented medial approach for infrapyloric nodal dissection in laparoscopic distal gastrectomy. Surg Endosc 32:2137–2148
Nakamura K, Suda K, Suzuki A, Nakauchi M, Shibasaki S, Kikuchi K, Nakamura T, Kadoya S, Inaba K, Uyama I (2018) Intracorporeal isosceles right triangle-shaped anastomosis in totally laparoscopic distal gastrectomy. Surg Laparosc, Endosc Percutaneous Tec 28:193–201
Shinohara T, Kanaya S, Taniguchi K, Fujita T, Yanaga K, Uyama I (2009) Laparoscopic total gastrectomy with D2 lymph node dissection for gastric cancer. Arc Surg 144:1138–1142
Inaba K, Satoh S, Ishida Y, Taniguchi K, Isogaki J, Kanaya S, Uyama I (2010) Overlap method: novel intracorporeal esophagojejunostomy after laparoscopic total gastrectomy. J Am Coll Surg 211:e25-29
Shibasaki S, Suda K, Nakauchi M, Nakamura K, Tanaka T, Kikuchi K, Inaba K, Uyama I (2021) Impact of the endoscopic surgical skill qualification system on the safety of laparoscopic gastrectomy for gastric cancer. Surg Endosc 35:6089–6100
Shinohara T, Satoh S, Kanaya S, Ishida Y, Taniguchi K, Isogaki J, Inaba K, Yanaga K, Uyama I (2013) Laparoscopic versus open D2 gastrectomy for advanced gastric cancer: a retrospective cohort study. Surg Endosc 27:286–294
Nakauchi M, Suda K, Kadoya S, Inaba K, Ishida Y, Uyama I (2016) Technical aspects and short- and long-term outcomes of totally laparoscopic total gastrectomy for advanced gastric cancer: a single-institution retrospective study. Surg Endosc 30:4632–4639
Suda K, Man IM, Ishida Y, Kawamura Y, Satoh S, Uyama I (2015) Potential advantages of robotic radical gastrectomy for gastric adenocarcinoma in comparison with conventional laparoscopic approach: a single institutional retrospective comparative cohort study. Surg Endosc 29:673–685
Shibasaki S, Suda K, Nakauchi M, Nakamura K, Kikuchi K, Inaba K, Uyama I (2020) Non-robotic minimally invasive gastrectomy as an independent risk factor for postoperative intra-abdominal infectious complications: A single-center, retrospective and propensity score-matched analysis. World J Gastroenterol 26:1172–1184
Nakauchi M, Suda K, Shibasaki S, Nakamura K, Kadoya S, Kikuchi K, Inaba K, Uyama I (2021) Prognostic factors of minimally invasive surgery for gastric cancer: Does robotic gastrectomy bring oncological benefit? World J Gastroenterol 27:6659–6672
Japanese gastric cancer treatment guidelines (2018) 5th edition. Gastric Cancer 24:1–21
Shibasaki S, Suda K, Nakauchi M, Kikuchi K, Kadoya S, Ishida Y, Inaba K, Uyama I (2017) Robotic valvuloplastic esophagogastrostomy using double flap technique following proximal gastrectomy: technical aspects and short-term outcomes. Surg Endosc 31:4283–4297
Uyama I, Kanaya S, Ishida Y, Inaba K, Suda K, Satoh S (2012) Novel integrated robotic approach for suprapancreatic D2 nodal dissection for treating gastric cancer: technique and initial experience. World J Surg 36:331–337
Suzuki K, Shibasaki S, Nakauchi M, Nakamura K, Akimoto S, Tanaka T, Kikuchi K, Inaba K, Uyama I, Suda K (2021) Impact of routine preoperative sonographic screening with early intervention for deep venous thrombosis in lower extremities on preventing postoperative venous thromboembolism in patients with gastric cancer scheduled for minimally invasive surgery. Langenbeck's archives of surgery / Deutsche Gesellschaft fur Chirurgie
Shibasaki S, Suda K, Kadoya S, Ishida Y, Nakauchi M, Nakamura K, Akimoto S, Tanaka T, Kikuchi K, Inaba K, Uyama I (2022) The safe performance of robotic gastrectomy by second-generation surgeons meeting the operating surgeon’s criteria in the Japan Society for Endoscopic Surgery guidelines. Asian J Endosc Surg 15:70–81
Shiomi S, Toriumi T, Yagi K, Asaoka R, Okumura Y, Wakamatsu K, Aikou S, Yamashita H, Nomura S, Seto Y (2021) Trunk fat volume can be a predictor of postoperative complications after gastrectomy: a retrospective cohort study. BMC Surg 21:207
Huguet A, Latournerie M, Debry PH, Jezequel C, Legros L, Rayar M, Boudjema K, Guyader D, Jacquet EB, Thibault R (2018) The psoas muscle transversal diameter predicts mortality in patients with cirrhosis on a waiting list for liver transplantation: a retrospective cohort study. Nutrition 51–52:73–79
Saitoh-Maeda Y, Kawahara T, Miyoshi Y, Tsutsumi S, Takamoto D, Shimokihara K, Hayashi Y, Mochizuki T, Ohtaka M, Nakamura M, Hattori Y, Teranishi JI, Yumura Y, Osaka K, Ito H, Makiyama K, Nakaigawa N, Yao M, Uemura H (2017) A low psoas muscle volume correlates with a longer hospitalization after radical cystectomy. BMC Urol 17:87
Zhang Y, Liu J, Li F, Cao F, Li A (2021) Contrast-enhanced computed tomography does not provide more information about sarcopenia than unenhanced computed tomography in patients with pancreatic cancer. Contrast Media Mol Imaging 2021:5546030
Taniguchi Y, Kurokawa Y, Takahashi T, Saito T, Yamashita K, Tanaka K, Makino T, Yamasaki M, Nakajima K, Eguchi H, Doki Y (2021) Impacts of preoperative psoas muscle mass and visceral fat area on postoperative short- and long-term outcomes in patients with gastric cancer. World J Surg 45:815–821
(2002) New criteria for ‘obesity disease’ in Japan. Circ J 66: 987–992
Nishikawa H, Shiraki M, Hiramatsu A, Moriya K, Hino K, Nishiguchi S (2016) Japan Society of Hepatology guidelines for sarcopenia in liver disease (1st edition): Recommendation from the working group for creation of sarcopenia assessment criteria. Hepatol Res 46:951–963
Kumagai K, Hiki N, Nunobe S, Kamiya S, Tsujiura M, Ida S, Ohashi M, Yamaguchi T, Sano T (2018) Impact of anatomical position of the pancreas on postoperative complications and drain amylase concentrations after laparoscopic distal gastrectomy for gastric cancer. Surg Endosc 32:3846–3854
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196
Katayama H, Kurokawa Y, Nakamura K, Ito H, Kanemitsu Y, Masuda N, Tsubosa Y, Satoh T, Yokomizo A, Fukuda H, Sasako M (2016) Extended Clavien-Dindo classification of surgical complications: Japan clinical oncology group postoperative complications criteria. Surg Today 46:668–685
Kanda Y (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48:452–458
Tamura T, Sakurai K, Nambara M, Miki Y, Toyokawa T, Kubo N, Tanaka H, Muguruma K, Yashiro M, Ohira M (2019) Adverse effects of preoperative sarcopenia on postoperative complications of patients with gastric cancer. Anticancer Res 39:987–992
Mueller TC, Reik L, Prokopchuk O, Friess H, Martignoni ME (2020) Measurement of body mass by bioelectrical impedance analysis and computed tomography in cancer patients with malnutrition - a cross-sectional observational study. Medicine (Baltimore) 99:e23642
Matsui R, Inaki N, Tsuji T (2021) Impact of preoperative muscle quality on postoperative severe complications after radical gastrectomy for gastric cancer patients. Ann Gastroenterol Surg 5:510–518
Shi B, Liu S, Chen J, Liu J, Luo Y, Long L, Lan Q, Zhang Y (2019) Sarcopenia is associated with perioperative outcomes in gastric cancer patients undergoing gastrectomy. Ann Nutr Metab 75:213–222
Yang SJ, Li HR, Zhang WH, Liu K, Zhang DY, Sun LF, Chen XL, Zhao LY, Chen XZ, Yang K, Chen ZX, Zhou ZG, Hu JK (2020) Visceral Fat Area (VFA) Superior to BMI for predicting postoperative complications after radical gastrectomy: a prospective cohort study. J Gastrointest Surg 24:1298–1306
Liu Y, Guo D, Niu Z, Wang Y, Fu G, Zhou Y, Xue Q, Jin X, Gong Z (2018) Prediction of the risk of laparoscopy-assisted gastrectomy by comparing visceral fat area and body mass index. Gastroenterol Res Pract 2018:1359626
Looijaard S, Te Lintel Hekkert ML, Wüst RCI, Otten RHJ, Meskers CGM, Maier AB (2021) Pathophysiological mechanisms explaining poor clinical outcome of older cancer patients with low skeletal muscle mass. Acta Physiol (Oxf) 231:e13516
Nelke C, Dziewas R, Minnerup J, Meuth SG, Ruck T (2019) Skeletal muscle as potential central link between sarcopenia and immune senescence. EBioMedicine 49:381–388
Cepeda MS, Boston R, Farrar JT, Strom BL (2003) Comparison of logistic regression versus propensity score when the number of events is low and there are multiple confounders. Am J Epidemiol 158:280–287
Tokunaga M, Tanizawa Y, Bando E, Kawamura T, Terashima M (2013) Poor survival rate in patients with postoperative intra-abdominal infectious complications following curative gastrectomy for gastric cancer. Ann Surg Oncol 20:1575–1583
Hanhivaara J, Määttä JH, Niinimäki J, Nevalainen MT (2020) Lumbosacral transitional vertebrae are associated with lumbar degeneration: retrospective evaluation of 3855 consecutive abdominal CT scans. Eur Radiol 30:3409–3416
Apaydin M, Uluc ME, Sezgin G (2019) Lumbosacral transitional vertebra in the young men population with low back pain: anatomical considerations and degenerations (transitional vertebra types in the young men population with low back pain). Radiol Med 124:375–381
Durand F, Buyse S, Francoz C, Laouénan C, Bruno O, Belghiti J, Moreau R, Vilgrain V, Valla D (2014) Prognostic value of muscle atrophy in cirrhosis using psoas muscle thickness on computed tomography. J Hepatol 60:1151–1157
Acknowledgements
The authors would like to thank MARUZEN YUSHODO (https://kw.maruzen.co.jp/kousei-honyaku/MZ-FujitaHealthUniversity2013/) for the English language editing.
Author information
Authors and Affiliations
Contributions
All authors have fully satisfied the ICMJE authorship criteria as detailed in the following: Study design: GI, SS, IU, and KS; Data collection: GI, SS, MN, AS, KN, and TT; Statistical analysis and interpretation of results: GI, SS, MN, SA, KI, and KS; Drafting of the manuscript: GI, SS, and KS; Critical revision of the manuscript for important intellectual content: SS, IU, and KS. All authors have read and approved the final manuscript and are accountable for all aspects of the work, particularly in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Disclosures
This study has been approved by a suitably constituted Ethics Committee of the institution (Committee of Fujita Health University Hospital, Approval No. HM18-409), and it conforms to the provisions of the Declaration of Helsinki. This work was not supported by any grant or funding. Gaku Inaguma, Susumu Shibasaki, Masaya Nakauchi, Kenichi Nakamura, Shingo Akimoto, Tsuyoshi Tanaka, Kazuki Inaba, Ichiro Uyama, and Koichi Suda have no commercial association with or financial involvement that might pose a conflict of interest in connection with the submitted article. Ichiro Uyama received lecture fees from Intuitive Surgical, Inc. outside of the submitted work. Tsuyoshi Tanaka and Ichiro Uyama received funding from Medicaroid, Inc. in relation to the Collaborative Laboratory for Research and Development in Advanced Surgical Technology, Fujita Health University. Koichi Suda received funding from Medicaroid, Inc. in relation to the Collaborative Laboratory for Research and Development in Advanced Surgical Intelligence, Fujita Health University, as well as advisory fees from Medicaroid, Inc. outside of the submitted work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Inaguma, G., Shibasaki, S., Nakauchi, M. et al. Muscle mass ratio in male gastric cancer patients as an independent predictor of postoperative complications after minimally invasive distal gastrectomy. Surg Endosc 37, 989–998 (2023). https://doi.org/10.1007/s00464-022-09595-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09595-y