Abstract
Background
Endoscopic full-thickness resection is a common endoscopic procedure for treating gastrointestinal submucosal tumors. Nasogastric tube placement is frequently performed after abdominal surgery, but the routine use of this approach remains controversial. The aim of this research was to explore whether nasogastric tube placement after gastric endoscopic full-thickness resection is necessary.
Methods
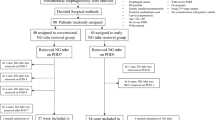
A retrospective study enrolled patients who underwent gastric endoscopic full-thickness resection in our hospital between January 2014 and January 2019, and all the patients had a tumor size ≤ 2 cm. The patients were divided into two groups according to whether a nasogastric tube was placed. Postprocedural adverse events and hospital stay duration were compared between the two groups using 1:1 propensity score matching.
Results
A total of 461 patients were enrolled in this study, including 385 patients in the nasogastric tube group (NGT group) and 76 patients in the non-nasogastric tube group (non-NGT group). After matching, the baseline characteristics of 73 patients in the NGT group and 73 patients in the non-NGT group were balanced (p > 0.05). The postprocedural fever rate in the NGT group was significantly higher than that in the non-NGT group (23.3% vs. 9.6%, p = 0.044). 6.9% (5/73) of patients experienced severe nasogastric tube-related throat discomfort. However, the duration of hospitalization stay was not different between the two groups.
Conclusions
For patients with tumor size ≤ 2 cm, routine nasogastric tube placement after gastric endoscopic full-thickness resection may be unnecessary.




Similar content being viewed by others
References
Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T, Repici A, Vieth M, De Ceglie A, Amato A, Berr F, Bhandari P, Bialek A, Conio M, Haringsma J, Langner C, Meisner S, Messmann H, Morino M, Neuhaus H, Piessevaux H, Rugge M, Saunders BP, Robaszkiewicz M, Seewald S, Kashin S, Dumonceau JM, Hassan C, Deprez PH (2015) Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 47:829–854
Chen H, Li B, Li L, Vachaparambil CT, Lamm V, Chu Y, Xu M, Cai Q (2019) Current status of endoscopic resection of gastric subepithelial tumors. Am J Gastroenterol 114:718–725
Ye LP, Yu Z, Mao XL, Zhu LH, Zhou XB (2014) Endoscopic full-thickness resection with defect closure using clips and an endoloop for gastric subepithelial tumors arising from the muscularis propria. Surg Endosc 28:1978–1983
Schmidt A, Bauder M, Riecken B, von Renteln D, Muehleisen H, Caca K (2015) Endoscopic full-thickness resection of gastric subepithelial tumors: a single-center series. Endoscopy 47:154–158
Guo J, Liu Z, Sun S, Liu X, Wang S, Ge N, Wang G, Qi Y (2015) Endoscopic full-thickness resection with defect closure using an over-the-scope clip for gastric subepithelial tumors originating from the muscularis propria. Surg Endosc 29:3356–3362
Liu S, Zhou X, Yao Y, Shi K, Yu M, Ji F (2020) Resection of the gastric submucosal tumor (G-SMT) originating from the muscularis propria layer: comparison of efficacy, patients’ tolerability, and clinical outcomes between endoscopic full-thickness resection and surgical resection. Surg Endosc 34:4053–4064
Cai MY, Martin Carreras-Presas F, Zhou PH (2018) Endoscopic full-thickness resection for gastrointestinal submucosal tumors. Digest Endosc Off J Jpn Gastroenterol Endosc Soc 30(Suppl 1):17–24
Sagar PM, Kruegener G, MacFie J (1992) Nasogastric intubation and elective abdominal surgery. Br J Surg 79:1127–1131
Carrère N, Seulin P, Julio CH, Bloom E, Gouzi JL, Pradère B (2007) Is nasogastric or nasojejunal decompression necessary after gastrectomy? A prospective randomized trial. World J Surg 31:122–127
Wei ZW, Li JL, Li ZS, Hao YT, He YL, Chen W, Zhang CH (2014) Systematic review of nasogastric or nasojejunal decompression after gastrectomy for gastric cancer. Eur J Surg Oncol J Eur Soc Surg Oncol Brit Assoc Surg Oncol 40:1763–1770
Lee JH, Kedia P, Stavropoulos SN, Carr-Locke D (2021) AGA clinical practice update on endoscopic management of perforations in gastrointestinal tract: expert review. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc 19:2252-2261.e2252
Nagami Y, Shiba M, Ominami M, Sakai T, Minamino H, Fukunaga S, Sugimori S, Tanaka F, Kamata N, Tanigawa T, Yamagami H, Watanabe T, Tominaga K, Fujiwara Y, Arakawa T (2017) Single locoregional triamcinolone injection immediately after esophageal endoscopic submucosal dissection prevents stricture formation. Clin Transl Gastroenterol 8:e75
Cheatham ML, Chapman WC, Key SP, Sawyers JL (1995) A meta-analysis of selective versus routine nasogastric decompression after elective laparotomy. Ann Surg 221:469–476; discussion 476-468
Chusilp S, Yamoto M, Vejchapipat P, Ganji N, Pierro A (2021) Nasogastric decompression after intestinal surgery in children: a systematic review and meta-analysis. Pediatr Surg Int 37:377–388
Weijs TJ, Kumagai K, Berkelmans GH, Nieuwenhuijzen GA, Nilsson M, Luyer MD (2017) Nasogastric decompression following esophagectomy: a systematic literature review and meta-analysis. Dis Esophagus 30:1–8
Ono H, Yao K, Fujishiro M, Oda I, Uedo N, Nimura S, Yahagi N, Iishi H, Oka M, Ajioka Y, Fujimoto K (2021) Guidelines for endoscopic submucosal dissection and endoscopic mucosal resection for early gastric cancer (second edition). Digest Endosc Off J Jpn Gastroenterol Endosc Soc 33:4–20
Japanese Gastric Cancer Association (2021) Japanese gastric cancer treatment guidelines 2018 (5th edition). Gastric Cancer Off J Int Gastric Cancer Assoc Jpn Gastric Cancer Assoc 24:1–21
Rajan E, Wong Kee Song LM (2018) Endoscopic full thickness resection. Gastroenterology 154:1925-1937.e1922
Torres A, El-Ebiary M, Rañó A (1999) Respiratory infectious complications in the intensive care unit. Clin Chest Med 20:287–301, viii
McAlister FA, Bertsch K, Man J, Bradley J, Jacka M (2005) Incidence of and risk factors for pulmonary complications after nonthoracic surgery. Am J Respir Crit Care Med 171:514–517
Liao F, Zhu Z, Lai Y, Pan X, Long S, Zhou X, Li G, Zhu Y, Chen Y, Shu X (2022) Risk factors for fever after esophageal endoscopic submucosal dissection and its derived technique. Front Med 9:713211
Bauer VP (2013) The evidence against prophylactic nasogastric intubation and oral restriction. Clin Colon Rectal Surg 26:182–185
Acknowledgements
We are grateful to the support of Jiangxi Clinical Research Center for Gastroenterology (20201ZDG02007).
Author information
Authors and Affiliations
Contributions
FL collected data, analyzed relevant information, and drafted the manuscript, DS collected data and wrote the manuscript. SY collected data. XP, SL, XZ, GL, YZ, and YC clinically managed the patient. ZZ and XS designed the article, approved the final submission, and clinically managed the patient.
Corresponding authors
Ethics declarations
Disclosures
Foqiang Liao, Danting Shao, Shuman Yao, Xiaolin Pan, Shunhua Long, Xiaojiang Zhou, Guohua Li, Yin Zhu, Youxiang Chen, Zhenhua Zhu and Xu Shu have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liao, F., Shao, D., Yao, S. et al. Routine nasogastric tube placement after gastric endoscopic full-thickness resection of tumor size ≤ 2 cm may be unnecessary: a propensity score-matching analysis. Surg Endosc 37, 932–940 (2023). https://doi.org/10.1007/s00464-022-09560-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09560-9