Abstract
Background
Laparoscopic inguinal hernia repair is one of the procedures most commonly performed by paediatric surgeons. Current research on the learning curve for laparoscopic hernia repair in children is scarce. This study aims to evaluate the clinical outcome and learning curve of laparoscopic intra-corporeal inguinal hernia repair in children.
Methods
A retrospective single-centre analysis of all paediatric patients who underwent laparoscopic intra-corporeal inguinal hernia repair between 2010 and 2019 was performed. The clinical outcomes were analysed. The data on the achievement of the learning curve by surgical trainees were evaluated with the CUSUM technique, focusing on operative time.
Results
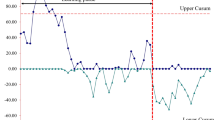
There were 719 patients with laparoscopic intra-corporeal inguinal hernia repair (comprising 1051 sides) performed during the study period. The overall ipsilateral recurrence rate was 1.8% without other complications detected. CUSUM analysis showed that there were 3 phases of training, for which the trainees underwent initial learning phase (Phase 1) for the first 7 cases. After mastering of the skills and extrapolating the skills to male patients with smaller body size (Phase 2), they then achieved performance comparable to that of the senior surgeons after 18 procedures (Phase 3).
Conclusions
18 procedures seem to be the number required to reach the learning curve plateau in terms of operative time by surgical trainees. The clinical outcomes show that laparoscopic intra-corporeal inguinal hernia repair is a safe and transferrable technique, even in the hands of trainees, with adequate supervision and careful case selection. It also provides skill acquisition for minimally invasive surgery.




Similar content being viewed by others
References
Chang SJ et al (2016) The incidence of inguinal hernia and associated risk factors of incarceration in pediatric inguinal hernia: a nation-wide longitudinal population-based study. Hernia 20(4):559–563
Chan IH, Wong KK (2017) Common urological problems in children: inguinoscrotal pathologies. Hong Kong Med J 23(3):272–281
Levitt MA et al (2002) Variability of inguinal hernia surgical technique: a survey of North American pediatric surgeons. J Pediatr Surg 37(5):745–751
Laberge JM (2002) What’s new in pediatric surgery. J Am Coll Surg 195(2):208–218
Esposito C et al (2012) Unilateral inguinal hernia: laparoscopic or inguinal approach. Decision making strategy: a prospective study. Eur J Pediatr 171(6):989–991
Chan KL, Hui WC, Tam PK (2005) Prospective randomized single-center, single-blind comparison of laparoscopic vs open repair of pediatric inguinal hernia. Surg Endosc 19(7):927–932
Toufique Ehsan M et al (2009) Laparoscopic hernioplasties in children: the implication on contralateral groin exploration for unilateral inguinal hernias. Pediatr Surg Int 25(9):759–762
Dreuning K et al (2019) Laparoscopic versus open pediatric inguinal hernia repair: state-of-the-art comparison and future perspectives from a meta-analysis. Surg Endosc 33(10):3177–3191
Yoshizawa J et al (2013) Laparoscopic percutaneous extraperitoneal closure for inguinal hernia: learning curve for attending surgeons and residents. Pediatr Surg Int 29(12):1281–1285
Shalaby R et al (2010) Laparoscopic hernia repair in infancy and childhood: evaluation of 2 different techniques. J Pediatr Surg 45(11):2210–2216
Valsamis EM et al (2018) Learning curves in surgery: variables, analysis and applications. Postgrad Med J 94(1115):525–530
Neugebauer E et al (1995) The E.A.E.S. Consensus development conferences on laparoscopic cholecystectomy, appendectomy, and hernia repair. Consensus statements–September 1994. The educational committee of the european association for endoscopic surgery. Surg Endosc 9(5):550–563
Mari G et al (1995) A postgraduate teaching course in laparoscopic surgery. Surg Endosc 9(10):1119–1122
Hopper AN, Jamison MH, Lewis WG (2007) Learning curves in surgical practice. Postgrad Med J 83(986):777–779
Pogorelić Z et al (2021) Learning curve for laparoscopic repair of pediatric inguinal hernia using percutaneous internal ring suturing. Children (Basel) 8(4):294
Barroso C et al (2017) Learning curves for laparoscopic repair of inguinal hernia and communicating hydrocele in children. Front Pediatr 5:207
Shibuya S et al (2019) The learning curve of laparoscopic percutaneous extraperitoneal closure (LPEC) for inguinal hernia: protocoled training in a single center for six pediatric surgical trainees. BMC Surg 19(1):6
Chan KL, Tam PK (2004) Technical refinements in laparoscopic repair of childhood inguinal hernias. Surg Endosc 18(6):957–960
Kuge H et al (2020) Learning curve for laparoscopic transabdominal preperitoneal repair: a single-surgeon experience of consecutive 105 procedures. Asian J Endosc Surg 13(2):205–210
Lim TO et al (2002) Assessing doctors’ competence: application of CUSUM technique in monitoring doctors’ performance. Int J Qual Health Care 14(3):251–258
Lipskar AM et al (2010) Laparoscopic inguinal hernia inversion and ligation in female children: a review of 173 consecutive cases at a single institution. J Pediatr Surg 45(6):1370–1374
Pant N, Aggarwal SK, Ratan SK (2014) Laparoscopic repair of hernia in children: comparison between ligation and nonligation of sac. J Indian Assoc Pediatr Surg 19(2):76–79
Gause CD et al (2017) Laparoscopic versus open inguinal hernia repair in children ≤3: a randomized controlled trial. Pediatr Surg Int 33(3):367–376
Maat S et al (2021) Comparison of intra- and extra-corporeal laparoscopic hernia repair in children: a systematic review and pooled data-analysis. J Pediatr Surg 56(9):1647–1656
Nasseri Y et al (2021) Learning curve in robotic colorectal surgery. J Robot Surg 15(3):489–495
Nomi T et al (2015) Learning curve for laparoscopic major hepatectomy. Br J Surg 102(7):796–804
Haas EM et al (2013) Critical appraisal of learning curve for single incision laparoscopic right colectomy. Surg Endosc 27(12):4499–4503
Cagir B et al (1994) The learning curve for laparoscopic cholecystectomy. J Laparoendosc Surg 4(6):419–427
Wong KP et al (2016) Determining the learning curve of transcutaneous laryngeal ultrasound in vocal cord assessment by CUSUM analysis of eight surgical residents: when to abandon laryngoscopy. World J Surg 40(3):659–664
McCulloch RA et al (2021) Assessing the performance and learning curve of orthopaedic surgical trainees in primary total hip arthroplasty. Ann R Coll Surg Engl 103(7):514–519
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Adrian Chi Heng Fung, Ivy Hau Yee Chan, and Prof. Kenneth Kak Yuen Wong have no conflicts of interest or financial ties to disclose.
Ethical approval
The project does not include any interaction or intervention with human subjects or include any access to identifiable private information therefore no IRB approval was deemed necessary.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fung, A.C.H., Chan, I.H.Y. & Wong, K.K.Y. Outcome and learning curve for laparoscopic intra-corporeal inguinal hernia repair in children. Surg Endosc 37, 434–442 (2023). https://doi.org/10.1007/s00464-022-09530-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09530-1