Abstract
Background
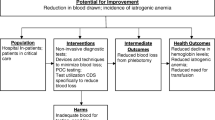
A quality improvement opportunity was identified to de-adopt the low-value care practice of routinely performing bloodwork for all patients undergoing elective bariatric surgery. While these patients are typically discharged on postoperative day 1 (POD1) after bloodwork is performed, it is uncommon for the discharge plan to change due to unexpected laboratory abnormalities alone.
Methods
Patients undergoing bariatric surgery between September 2020 and April 2021 only had POD1 bloodwork if there were perioperative clinical concerns, they had insulin-dependent diabetes, or they were therapeutically anticoagulated. Thirty-day Emergency Department (ED) visits and readmissions were monitored as balancing measures. Outcomes were compared to a control group that underwent bariatric surgery prior to September 2020 when POD1 laboratory testing was routinely performed. Financial and environmental costs were estimated based our institutional standards.
Results
The intervention group consisted of 303 patients: 248 (82%) Roux-en-Y gastric bypasses and 55 (18%) sleeve gastrectomies. Most patients (n = 256, 84.5%) did not have POD1 bloodwork. Twelve (3.9%) had bloodwork performed in violation of our protocol, of which none had a change in management based on the results. Of the 35 (12%) who had appropriately ordered bloodwork, 6 (2%) required a transfusion and 2 (0.7%) required a second surgery on the same admission for hemorrhage. Forty-four (14.5%) had 30-day ED visits of which 17 (5.6%) were within 7 days. Sixteen (5.3%) were readmitted. There were no significant differences between intervention and control groups in the rate of transfusion, second surgery, or 30-day ED visits. The avoidance of POD1 bloodwork saved approximately $6602.24 in lab processing fees alone and 512 test tubes.
Conclusion
POD1 bloodwork can be safely avoided in the absence of clinical concerns. In addition to not significantly increasing postoperative complications, there were benefits from a financial cost, environmental impact, and patient discomfort perspective.
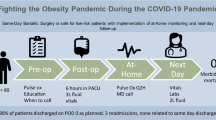
Graphical abstract

Similar content being viewed by others
References
Levinson W, Huynh T (2014) Engaging physicians and patients in conversations about unnecessary tests and procedures: choosing Wisely Canada. CMAJ 186(5):325–326. https://doi.org/10.1503/cmaj.131674
Mafi JN, Parchman M (2018) Low-value care: an intractable global problem with no quick fix. BMJ Qual Saf 27(5):333–336. https://doi.org/10.1136/bmjqs-2017-007477
Choosing Wisely Canada, Anesthesiology (2018) Five things physicians and patients should question. Choosing Wisely Canada, Toronto, ON. https://choosingwiselycanada.org/anesthesiology/
Murphy AM, Tunitsky-Bitton E, Krlin RM, Barber MD, Goldman HB (2013) Utility of postoperative laboratory studies after female pelvic reconstructive surgery. Am J Obstet Gynecol 209(4):363.e1-363.e3635. https://doi.org/10.1016/j.ajog.2013.06.008
Manning BT, Sankaranarayanan S, Hassanzadeh H, Nandyala SV, Marquez-Lara A, Naqvi A, Elboghdady IM, Noureldin M, Singh K (2014) The utility of obtaining routine hematological laboratory values following an anterior cervical diskectomy and fusion. Spine 39(20):E1228–E1232. https://doi.org/10.1097/BRS.0000000000000512
Halawi MJ, Plourde JM, Cote MP (2019) Routine postoperative laboratory tests are not necessary after primary total hip arthroplasty. J Arthroplasty 34(3):538–541. https://doi.org/10.1016/j.arth.2018.11.037
Niven DJ, Mrklas KJ, Holodinsky JK, Straus SE, Hemmelgarn BR, Jeffs LP, Stelfox HT (2015) Towards understanding the de-adoption of low-value clinical practices: a scoping review. BMC Med 13:255. https://doi.org/10.1186/s12916-015-0488-z
Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program. American College of Surgeons. https://www.facs.org/quality-programs/mbsaqip. Accessed 28 Sept 2021
Mostello AJ, Tenpenny W, Lingamfelter M, Wu ES (2020) Daily postoperative complete blood counts after primary total joint arthroplasty may not always be necessary. Orthopedics 43(1):e31–e36. https://doi.org/10.3928/01477447-20191031-08
Howell EP, Kildow BJ, Karas V, Green CL, Cunningham DJ, Ryan SP, Bolognesi MP, Seyler TM (2019) Clinical impact of routine complete blood counts following total knee arthroplasty. J Arthroplasty 34(7S):S168–S172. https://doi.org/10.1016/j.arth.2019.03.016
United Nations Climate Action (2019) https://www.un.org/en/climatechange/climate-action-areas.shtml.
World Health Organisation (WHO) (2019). https://www.who.int/health-topics/climate-change#tab=tab_1.
Mortimer F, Isherwood J, Wilkinson A, Vaux E (2018) Sustainability in quality improvement: redefining value. Future Healthc J 5(2):88–93
Penny T, Collins M, Whiting A, Aumonier S (2015). Care pathways: guidance of appraising sustainability. coalition for sustainabile pharmaceuticals and medical devices.
Presley B, Isenberg JD (2020) Ultrasound guided intravenous access. StatPearls Publishing, In StatPearls
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Rajajee Selvam, Amer Jarrar, Cynthia Meghaizel, Joseph Mamazza, Amy Neville, Caolan Walsh, and Nicole Kolozsvari have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Selvam, R., Jarrar, A., Meghaizel, C. et al. Redefining the role of routine postoperative bloodwork following uncomplicated bariatric surgery. Surg Endosc 37, 364–370 (2023). https://doi.org/10.1007/s00464-022-09518-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09518-x