Abstract
Background
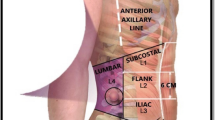
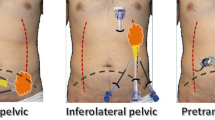
The best approach for lateral incisional hernia is not known. Posterior component separation (reverse TAR) offers the possibility of using the retromuscular space for medial extension of the challenging preperitoneal plane. The aim of our multicenter study was to compare the operative and patient-reported outcomes measures (PROMs) using two open surgical techniques from the lateral approach: a totally preperitoneal vs a reverse TAR.
Methods
A retrospective cohort study was performed since 2012 to 2020. Patients with lateral incisional hernia treated through a lateral approach were identified from a prospectively maintained multicenter database. Reverse TAR was added when the preperitoneal plane could not be safely dissected. The results obtained using these two lateral approaches were compared, including short- and long-term complications, as well as PROMs, using the specific tool EuraHSQoL.
Results
A total of 61 patients were identified. Reverse TAR was performed in 33 patients and lateral retromuscular preperitoneal approach in 28 patients. Both groups were comparable in terms of sociodemographic and comorbidities variables. Surgical site occurrences occurred in 13 cases (21.3%), with 8 patients (13.1%) requiring procedural intervention. During a median follow-up of 34 months, no incisional hernia recurrence was registered. There was a case (1.6%) of symptomatic bulging that required reoperation. Also 12 patients (19.7%) presented an asymptomatic bulging. No statistically significant difference was identified in the complications and PROMs between the two procedures.
Conclusion
The open lateral retromuscular reconstruction using very large meshes that reach the midline has excellent long-term results with acceptable postoperative complications, including PROMs. A reverse TAR may be added, when necessary, without increasing complications and obtaining similar long-term results.
Graphical abstract












Similar content being viewed by others
Abbreviations
- ASA:
-
American Society of Anesthesiologists
- AWR:
-
Abdominal wall reconstruction
- BMI:
-
Body mass index
- CDC:
-
Centers for Disease Control and Prevention
- CeDAR:
-
Carolina’s equation for determining associated risks
- COPD:
-
Chronic obstructive pulmonary disease
- CT:
-
Computed tomography
- DVT:
-
Deep venous thrombosis
- EHS:
-
European Hernia Society
- EuraHSQoL:
-
European Abdominal Wall Hernia Quality of Life Scores
- GEE:
-
Generalized estimating equations
- ICAP:
-
International Classification of Abdominal Wall Planes
- IH:
-
Incisional hernia
- LAW:
-
Lateral abdominal wall
- PCS:
-
Posterior component separation
- PE:
-
Pulmonary thromboembolism
- PROM:
-
Patient-reported outcomes measure
- QoL:
-
Quality of Life
- SPSS:
-
Statistical Package for the Social Sciences
- SSI:
-
Surgical site infection
- SSO:
-
Surgical site occurrence
- SSOPI:
-
Surgical site occurrence that required procedural intervention
- STROB:
-
Strengthening the Reporting of Observational Studies in Epidemiology
- STROCSS:
-
Strengthening the Reporting of Cohort Studies in Surgery
- TAR:
-
Transversus abdominis release
- VHSS:
-
Ventral hernia staging system
- VHWG:
-
Ventral hernia working group
References
Kapur SK, Liu J, Baumann DP, Butler CE (2019) Surgical outcomes in lateral abdominal wall reconstruction: a comparative analysis of surgical techniques. J Am Coll Surg 229:267–276
Chatterjee S, Nam R, Fleshner N, Klotz L (2004) Permanent flank bulge is a consequence of flank incision for radical nephrectomy in one half of patients. Urol Oncol Semin Orig Investig 22:36–39
Takei A, Sazuka T, Nakamura K, Nihei N, Ichikawa T (2016) Port-site transversus abdominis fascia closure reduced the incidence of incisional hernia following retroperitoneal laparoscopic nephrectomy. Hernia 20:735–740
Munoz-Rodriguez JM, Lopez-Monclus J, San Miguel Mendez C, Perez-Flecha Gonzalez M, de Robin-Valle Lersundi A, Blázquez Hernando LA, Cuccurullo D, Garcia-Hernandez E, Sanchez-Turrión V, Garcia-Urena MA (2020) Outcomes of abdominal wall reconstruction in patients with the combination of complex midline and lateral incisional hernias. Surgery (United States) 168:532–542
Renard Y, de Mestier L, Cagniet A, Demichel N, Marchand C, Meffert JL, Kianmanesh R, Palot JP (2017) Open retromuscular large mesh reconstruction of lumbar incisional hernias including the atrophic muscular area. Hernia 21:341–349
Veyrie N, Poghosyan T, Corigliano N, Canard G, Servajean S, Bouillot JL (2013) Lateral incisional hernia repair by the retromuscular approach with polyester standard mesh: topographic considerations and long-term follow-up of 61 consecutive patients. World J Surg 37:538–544
Beffa LR, Margiotta AL, Carbonell AM (2018) Flank and lumbar hernia repair. Surg Clin North Am 98:593–605
Moreno-Egea A, Alcaraz AC, Cuervo MC (2013) Surgical options in lumbar hernia: laparoscopic versus open repair. A long-term prospective study. Surg Innov 20:331–344
Novitsky YW, Elliott HL, Orenstein SB, Rosen MJ (2012) Transversus abdominis muscle release: a novel approach to posterior component separation during complex abdominal wall reconstruction. Am J Surg 204:709–716
Gibreel W, Sarr MG, Rosen M, Novitsky Y (2016) Technical considerations in performing posterior component separation with transverse abdominis muscle release. Hernia 20:449–459
Jones CM, Winder JS, Potochny JD, Pauli EM (2016) Posterior component separation with transversus abdominis release: technique, utility, and outcomes in complex abdominal wall reconstruction. Plast Reconstr Surg 137:636–646
Reinpold W (2018) Transversus abdominis muscle release: technique, indication, and results. Int J Abdom Wall Hernia Surg 1:79–86
Robin-Lersundi A, Blazquez Hernando L, López-Monclús J, Cruz Cidoncha A, San Miguel Méndez C, Jimenez Cubedo E, García-Ureña MA (2018) How we do it: down to up posterior components separation. Langenbeck’s Arch Surg 403:539–546
Phillips MS, Krpata DM, Blatnik JA, Rosen MJ (2012) Retromuscular preperitoneal repair of flank hernias. J Gastrointest Surg 16:1548–1553
Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, Chelala E, Dietz UA, Eker HH, El Nakadi I, Hauters P, Hidalgo Pascual M, Hoeferlin A, Klinge U, Montgomery A, Simmermacher RKJ, Simons MP, Śmietański M, Sommeling C, Tollens T, Vierendeels T, Kingsnorth A (2009) Classification of primary and incisional abdominal wall hernias. Hernia 13:407–414
Agha R, Abdall-Razak A, Crossley E, Dowlut N, Iosifidis C, Mathew G (2019) STROCSS 2019 Guideline: strengthening the reporting of cohort studies in surgery. Int J Surg 72:156–165
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP (2014) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg 12:1495–1499
Muysoms FE, Deerenberg EB, Peeters E, Agresta F, Berrevoet F, Campanelli G, Ceelen W, Champault GG, Corcione F, Cuccurullo D, Debeaux AC, Dietz UA, Fitzgibbons RJ, Gillion JF, Hilgers RD, Jeekel J, Kyle-Leinhase I, Köckerling F, Mandala V, Montgomery A, Morales-Conde S, Simmermacher RKJ, Schumpelick V, Śmietański M, Walgenbach M, Miserez M (2013) Recommendations for reporting outcome results in abdominal wall repair: results of a consensus meeting in Palermo, Italy, 28–30 June 2012. Hernia 17:423–433
Parker SG, Halligan S, Liang MK, Muysoms FE, Adrales GL, Boutall A, de Beaux AC, Dietz UA, Divino CM, Hawn MT, Heniford TB, Hong JP, Ibrahim N, Itani KMF, Jorgensen LN, Montgomery A, Morales-Conde S, Renard Y, Sanders DL, Smart NJ, Torkington JJ, Windsor ACJ (2020) International classification of abdominal wall planes (ICAP) to describe mesh insertion for ventral hernia repair. Br J Surg 107:209–217
Slater NJ, Montgomery A, Berrevoet F, Carbonell AM, Chang A, Franklin M, Kercher KW, Lammers BJ, Parra-Davilla E, Roll S, Towfigh S, Van Geffen E, Conze J, Van Goor H (2014) Criteria for definition of a complex abdominal wall hernia. Hernia 18:7–17
Breuing K, Butler CE, Ferzoco S, Franz M, Hultman CS, Kilbridge JF, Rosen M, Silverman RP, Vargo D (2010) Incisional ventral hernias: review of the literature and recommendations regarding the grading and technique of repair. Surgery 148:544–558
Petro CC, O’Rourke CP, Posielski NM, Criss CN, Raigani S, Prabhu AS, Rosen MJ (2016) Designing a ventral hernia staging system. Hernia 20:111–117
Augenstein VA, Colavita PD, Wormer BA, Walters AL, Bradley JF, Lincourt AE, Horton J, Heniford BT (2015) CeDAR: carolinas equation for determining associated risks. J Am Coll Surg 221:S65–S66
Haskins IN, Horne CM, Krpata DM, Prabhu AS, Tastaldi L, Perez AJ, Rosenblatt S, Poulose BK, Rosen MJ (2018) A call for standardization of wound events reporting following ventral hernia repair. Hernia 22:729–736
Garner JS (1986) CDC guideline for prevention of surgical wound infections, 1985. Supersedes guideline for prevention of surgical wound infections published in 1982. (Originally published in november 1985). Rev Infect Control 7:193–200
García-Ureña MÁ, López-Monclús J, Cuccurullo D, Blázquez Hernando LA, García-Pastor P, Reggio S, Jiménez Cubedo E, San Miguel Méndez C, Cruz Cidoncha A, Valle R, de Lersundi A (2019) Abdominal wall reconstruction utilizing the combination of absorbable and permanent mesh in a retromuscular position: a multicenter prospective study. World J Surg 43:149–158
San Miguel-Méndez C, López-Monclús J, Munoz-Rodriguez J, de Lersundi ÁRV, Artes-Caselles M, Blázquez Hernando LA, García-Hernandez JP, Minaya-Bravo AM, Garcia-Urena MÁ (2021) Stepwise transversus abdominis muscle release for the treatment of complex bilateral subcostal incisional hernias. Surgery. https://doi.org/10.1016/j.surg.2021.04.007
Muysoms F, Campanelli G, Champault GG, DeBeaux AC, Dietz UA, Jeekel J, Klinge U, Köckerling F, Mandala V, Montgomery A, Morales Conde S, Puppe F, Simmermacher RKJ, Śmietański M, Miserez M (2012) EuraHS: the development of an international online platform for registration and outcome measurement of ventral abdominal wall hernia repair. Hernia 16:239–250
de Robin Valle de Lersundi A, Munoz-Rodriguez J, Lopez-Monclus J, Blazquez Hernando LA, San Miguel C, Minaya A, Perez-Flecha M, Garcia-Urena MA (2021) Second look after retromuscular repair with the combination of absorbable and permanent meshes. Front Surg 7:2021. https://doi.org/10.3389/fsurg.2020.611308
Hanley JA, Negassa A, deB Edwardes MD, Forrester JE (2003) Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol 157:364–375
Alkhatib H, Tastaldi L, Krpata DM, Petro CC, Fafaj A, Rosenblatt S, Rosen MJ, Prabhu AS (2020) Outcomes of transversus abdominis release (TAR) with permanent synthetic retromuscular reinforcement for bridged repairs in massive ventral hernias: a retrospective review. Hernia 24:341–352
Winder JS, Majumder A, Fayezizadeh M, Novitsky YW, Pauli EM (2018) Outcomes of utilizing absorbable mesh as an adjunct to posterior sheath closure during complex posterior component separation. Hernia 22:303–309
Gardner GP, Josephs LG, Rosca M, Rich J, Woodson J, Menzoian JO (1994) The Retroperitoneal incision: an evaluation of postoperative flank ‘bulge.’ Arch Surg 129:753–756
Crouzet S, Chopra S, Tsai S, Kamoi K, Haber GP, Remer EM, Berger AK, Gill IS, Aron M (2014) Flank muscle volume changes after open and laparoscopic partial nephrectomy. J Endourol 28:1202–1207
Van Der Graaf T, Verhagen PCMS, Kerver ALA, Kleinrensink GJ (2011) Surgical anatomy of the 10th and 11th intercostal, and subcostal nerves: prevention of damage during lumbotomy. J Urol 186:579–583
Reinpold W, Schröder M, Berger C, Nehls J, Schröder A, Hukauf M, Köckerling F, Bittner R (2019) Mini- or less-open sublay operation (MILOS). Ann Surg 269:748–755
Li B, Qin C, Yu J, Gong D, Nie X, Li G, Bittner R (2021) Totally endoscopic sublay (TES) repair for lateral abdominal wall hernias: technique and first results. Hernia 25:523–533
Garcia-Urena MÁ, Lopez-Monclus J, de Robin Valle de Lersundi A, Blazquez Hernando LA, Medina Pedrique M, Rial Justo X, Cruz Cidoncha A, Nogueira Sixto M, Munoz-Rodriguez J (2022) Pathways of the preperitoneal plane: from the “fatty triangle” in rives to the “fatty trident” in extended retromuscular abdominal wall reconstruction. A tribute to Prof Schumpelick. Hernia. https://doi.org/10.1007/S10029-022-02602-0
Stoppa RE (1989) The treatment of complicated groin and incisional hernias. World J Surg 13:545–554
Petersen S, Schuster F, Steinbach F, Henke G, Hellmich G, Ludwig K (2002) Sublay prosthetic repair for incisional hernia of the flank. J Urol 168:2461–2463
Carbonell AM, Kercher KW, Sigmon L, Matthews BD, Sing RF, Kneisl JS, Heniford BT (2005) A novel technique of lumbar hernia repair using bone anchor fixation. Hernia 9:22–25
Zieren J, Menenakos C, Taymoorian K, Müller JM (2007) Flank hernia and bulging after open nephrectomy: mesh repair by flank or median approach? Report of a novel technique. Int Urol Nephrol 39:989–993
Luc G, David A, Couzi L, Midy D, Collet D, Dubuisson V (2014) Lateral incisional hernia after renal transplantation: a comparative study. World J Surg 38:2791–2796
Purnell CA, Park E, Turin SY, Dumanian GA (2016) Postoperative flank defects, hernias, and bulges: a reliable method for repair. Plast Reconstr Surg 137:994–1001
Kearney AM, Dumanian GA (2020) Simplified repair of traumatic iliac crest flank hernias with mesh strips. Plast Reconstr Surg - Glob Open 8:e2970
Acknowledgements
We thank Dixie Huntley MD for her linguistic assistance during the preparation of this article.
Funding
No funding was received for this article.
Author information
Authors and Affiliations
Contributions
JMMR, JLM, MPF, ARVDL, LABH, AR, JPGH, AEA, MMP, and MAGU have participated in the preparation of the article by meeting the following criteria: Authors make substantial contributions to conception and design, and/or acquisition of data, and/or analysis and interpretation of data; Authors participate in drafting the article or revising it critically for important intellectual content; Authors give final approval of the version to be submitted and any revised version to be published.
Corresponding author
Ethics declarations
Disclosures
Joaquin M. Munoz-Rodriguez receives speaker fee from Braun and WL Gore & Associates. Javier Lopez-Monclus having receives speaker fees from Medtronic, Dipromed and WL Gore & Associates. Alvaro Robin Valle De Lersundi receives speaker fee from WL Gore & Associates. Luis A. Blazquez-Hernando receives speaker fees from Dipromed and WL Gore & Associates.Miguel A. Garcia-Urena received speaker fees from Medtronic, Bard, Dipromed, Dynamesh, Braun, Johnson and Johnson, Telabio and WL Gore & Associates and Medtronic. Marina Perez-Flecha, Ana Royuela, Juan P. Garcia-Hernandez, Aritz Equisoain Azcona, Manuel Medina Pedrique have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 140870 kb) Video 1: Lateral retromuscular preperitoneal technique. Video clip showing the stepwise preperitoneal retromuscular lateral surgical technique
Supplementary file2 (MP4 148937 kb) Video 2: Reverse TAR technique. Video clip showing the stepwise reverse TAR surgical technique
Rights and permissions
About this article
Cite this article
Munoz-Rodriguez, J.M., Lopez-Monclus, J., Perez-Flecha, M. et al. Reverse TAR may be added when necessary in open preperitoneal repair of lateral incisional hernias: a retrospective multicentric cohort study. Surg Endosc 36, 9072–9091 (2022). https://doi.org/10.1007/s00464-022-09375-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09375-8