Abstract
Background
Robot-assisted surgery is expanding worldwide. Most research in this field concentrates on surgeons’ technical skills and patient outcome, but research from open and laparoscopic surgery shows that teamwork is crucial for patient safety. Team composition is changed in robot-assisted surgery with the surgeon placed away from the bedside, potentially altering teamwork and workflow in the operating theatre. This scoping review aimed to explore how factors affecting workflow as well as team members’ social and cognitive skills during robot-assisted surgery are reported in the literature.
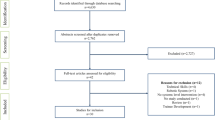
Methods
A systematic search was performed in the databases Medline, EMBASE, PsycINFO, and Web of Science. Reports were screened according to the Preferred Reporting Item for Systematic reviews and Meta-Analysis for Scoping Review guidelines. Inclusion criteria were robot-assisted surgery, multi-professional teams, and workflow, flow disruptions, or non-technical skills.
Results
A total of 12,527 references were screened, and 24 articles were included in the review. Articles were heterogeneous in terms of aim, methods and focus. The studies concentrated on two main fields: flow disruptions and the categorization of their causes and incidences; and non-technical skills describing the challenges of communication and effects on situation awareness.
Conclusion
Many studies focused on flow disruptions and found that communication, coordination, training, and equipment/technology were the most frequent causes. Another focus of studies was non-technical skills—primarily communication and situation awareness. Future studies could focus on how to prevent the most harmful flow disruptions and develop interventions for improving workflow.

Similar content being viewed by others
References
De Vries EN, Ramrattan MA, Smorenburg SM, Gouma DJ, Boermeester MA (2008) The incidence and nature of in-hospital adverse events: a systematic review. Qual Saf Heal Care 17:216–223. https://doi.org/10.1136/qshc.2007.023622
Rogers SO, Gawande AA, Kwaan M, Puopolo AL, Yoon C, Brennan TA, Studdert DM (2006) Analysis of surgical errors in closed malpractice claims at 4 liability insurers. Surgery 140:25–33. https://doi.org/10.1016/j.surg.2006.01.008
Flin R, O’connor P, Crichton M (2008) Safety at the sharp End: a guide to non-technical skills. Ashgate, Burlington, VT
Gjeraa K, Spanager L, Konge L, Petersen RH, Østergaard D (2016) Non-technical skills in minimally invasive surgery teams: a systematic review. Surg Endosc 30:5185–5199. https://doi.org/10.1007/s00464-016-4890-1
Wiegmann DA, ElBardissi AW, Dearani JA, Daly RC, Sundt TM (2007) Disruptions in surgical flow and their relationship to surgical errors: an exploratory investigation. Surgery 142:658–665. https://doi.org/10.1016/j.surg.2007.07.034
Arksey H, O’Malley L (2005) Scoping studies: towards a methodological framework. Int J Soc Res Methodol Theory Pract 8:19–32. https://doi.org/10.1080/1364557032000119616
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE (2018) PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 169:467. https://doi.org/10.7326/M18-0850
Catchpole K, Perkins C, Bresee C, Solnik MJ, Sherman B, Fritch J, Gross B, Jagannathan S, Hakami-Majd N, Avenido R, Anger JT (2016) Safety, efficiency and learning curves in robotic surgery: a human factors analysis. Surg Endosc 30:3749–3761. https://doi.org/10.1007/s00464-015-4671-2
Catchpole KR, Hallett E, Curtis S, Mirchi T, Souders CP, Anger JT (2018) Diagnosing barriers to safety and efficiency in robotic surgery. Ergonomics 61:26–39. https://doi.org/10.1080/00140139.2017.1298845
Cofran L, Cohen T, Alfred M, Kanji F, Choi E, Savage S, Anger J, Catchpole K (2021) Barriers to safety and efficiency in robotic surgery docking. Surg Endosc. https://doi.org/10.1007/s00464-020-08258-0
Dru CJ, Anger JT, Souders CP, Bresee C, Weigl M, Hallett E, Catchpole K (2017) Surgical flow disruptions during robotic-assisted radical prostatectomy. Can J Urol 24:8814–8821
El-Hamamsy D, Walton TJ, Griffiths TRL, Anderson ES, Tincello DG (2020) Surgeon-team separation in robotic theaters: a qualitative observational and interview study. Female Pelvic Med Reconstr Surg 26:86–91. https://doi.org/10.1097/SPV.0000000000000829
Jain M, Fry BT, Hess LW, Anger JT, Gewertz BL, Catchpole K (2016) Barriers to efficiency in robotic surgery: the resident effect. J Surg Res 205:296–304. https://doi.org/10.1016/j.jss.2016.06.092
Souders CP, Catchpole K, Hannemann A, Lyon R, Eilber KS, Bresee C, Cohen T, Weigl M, Anger JT (2019) Flow disruptions in robotic-assisted abdominal sacrocolpopexy: does robotic surgery introduce unforeseen challenges for gynecologic surgeons? Int Urogynecol J. https://doi.org/10.1007/s00192-019-03929-6
Weber J, Catchpole K, Becker AJ, Schlenker B, Weigl M (2018) Effects of flow disruptions on mental workload and surgical performance in robotic-assisted surgery. World J Surg 42:3599–3607. https://doi.org/10.1007/s00268-018-4689-4
Weigl M, Weber J, Hallett E, Pfandler M, Schlenker B, Becker A, Catchpole K (2018) Associations of intraoperative flow disruptions and operating room teamwork during robotic-assisted radical prostatectomy. Urology 114:105–113. https://doi.org/10.1016/j.urology.2017.11.060
Ahmad N, Hussein AA, Cavuoto L, Sharif M, Allers JC, Hinata N, Ahmad B, Kozlowski JD, Hashmi Z, Bisantz A, Guru KA (2016) Ambulatory movements, team dynamics and interactions during robot-assisted surgery. BJU Int 118:132–139. https://doi.org/10.1111/bju.13426
Allers JC, Hussein AA, Ahmad N, Cavuoto L, Wing JF, Hayes RM, Hinata N, Bisantz AM, Guru KA (2016) Evaluation and impact of workflow interruptions during robot-assisted surgery. Urology 92:33–37. https://doi.org/10.1016/j.urology.2016.02.040
Manuguerra A, Mazeaud C, Hubert N, Eschwège P, Roumiguié M, Salleron J, Hubert J (2021) Non-technical skills in robotic surgery and impact on near-miss events: a multi-center study. Surg Endosc 35:5062–5071. https://doi.org/10.1007/s00464-020-07988-5
Raheem S, Ahmed YE, Hussein AA, Johnson A, Cavuoto L, May P, Cole A, Wang D, Ahmad B, Hasasneh A, Guru KA (2018) Variability and interpretation of communication taxonomy during robot-assisted surgery: do we all speak the same language? BJU Int 122:99–105. https://doi.org/10.1111/bju.14150
Sexton K, Johnson A, Gotsch A, Hussein AA, Cavuoto L, Guru KA (2018) Anticipation, teamwork and cognitive load: chasing efficiency during robot-assisted surgery. BMJ Qual Saf 27:148–154. https://doi.org/10.1136/bmjqs-2017-006701
Tiferes J, Hussein AA, Bisantz A, Higginbotham DJ, Sharif M, Kozlowski J, Ahmad B, O’Hara R, Wawrzyniak N, Guru K (2019) Are gestures worth a thousand words? Verbal and nonverbal communication during robot-assisted surgery. Appl Ergon 78:251–262. https://doi.org/10.1016/j.apergo.2018.02.015
Tiferes J, Hussein AA, Bisantz A, Kozlowski JD, Sharif MA, Winder NM, Ahmad N, Allers J, Cavuoto L, Guru KA (2016) The loud surgeon behind the console: understanding team activities during robot-assisted surgery. J Surg Educ 73:504–512. https://doi.org/10.1016/j.jsurg.2015.12.009
Cunningham S, Chellali A, Jaffre I, Classe J-M (2012) Effects of experience and workplace culture in human-robot team interaction in robotic surgery: a case study. Int J Soc Robot. https://doi.org/10.1007/s12369-012
Randell R, Greenhalgh J, Hindmarsh J, Honey S, Pearman A, Alvarado N, Dowding D (2019) How do team experience and relationships shape new divisions of labour in robot-assisted surgery? A realist investigation. Health. https://doi.org/10.1177/1363459319874115
Almeras C, Almeras C (2019) Operating room communication in robotic surgery: Place, modalities and evolution of a safe system of interaction. J Visc Surg. https://doi.org/10.1016/j.jviscsurg.2019.02.004
Schiff L, Tsafrir Z, Aoun J, Taylor A, Theoharis E, Eisenstein D (2016) Quality of communication in robotic surgery and surgical outcomes. JSLS J Soc Laparoendosc Surg. https://doi.org/10.4293/JSLS.2016.00026
Tsafrir Z, Janosek-Albright K, Aoun J, Diaz-Insua M, Abd-El-Barr A-E-R, Schiff L, Talukdar S, Menon M, Munkarah A, Theoharis E, Eisenstein D (2020) The impact of a wireless audio system on communication in robotic-assisted laparoscopic surgery: a prospective controlled trial. Plos One. https://doi.org/10.1371/journal.pone.0220214
Alvarado N, Honey S, Greenhalgh J, Pearman A, Dowding D, Cope A, Long A, Jayne D, Gill A, Kotze A, Randell R (2017) Eliciting context-mechanism-outcome configurations: experiences from a realist evaluation investigating the impact of robotic surgery on teamwork in the operating theatre. Eval Int J Theory, Res Pract 23:444–462. https://doi.org/10.1177/1356389017732172
Randell R, Alvarado N, Honey S, Greenhalgh J, Gardner P, Gill A, Jayne D, BCh M, Kotze A, ChB M, Pearman A, Dowding D (2005) Impact of robotic surgery on decision making: perspectives of surgical teams. AMIA Annu Symp Proc 2015:1057–1066
Schreyer J, Koch A, Herlemann A, Becker A, Schlenker B, Catchpole K, Weigl M (2021) RAS-NOTECHS: validity and reliability of a tool for measuring non-technical skills in robotic-assisted surgery settings. Surg Endosc. https://doi.org/10.1007/s00464-021-08474-2
Moulton CA, Regehr G, Lingard L, Merritt C, MacRae H (2010) Slowing down to stay out of trouble in the operating room: remaining attentive in automaticity. Acad Med 85:1. https://doi.org/10.1097/ACM.0b013e3181f073dd
Bruun B, Poulsen JL, Møhl P, Spanager L (2021) Is non-stop always better? Examining assumptions behind the concept of flow disruptions in studies of robot-assisted surgery. J Robot Surg. https://doi.org/10.1007/s11701-021-01275-8
Hollnagel E (2014) Safety-I and safety-II: the past and future of safety management, 1st edn. Ashgate Publishing Ltd., Farnham
Dieckmann P, Patterson M, Lahlou S, Mesman J, Nyström P, Krage R (2017) Variation and adaptation: learning from success in patient safety-oriented simulation training. Adv Simul 2:1–14. https://doi.org/10.1186/s41077-017-0054-1
Randell R, Honey S, Alvarado N, Pearman A, Greenhalgh J, Long A, Gardner P, Gill A, Jayne D, Dowding D (2016) Embedding robotic surgery into routine practice and impacts on communication and decision making: a review of the experience of surgical teams. Cogn Technol Work 18:423–437. https://doi.org/10.1007/s10111-016-0368-0
van der Vliet WJ, Haenen SM, Solis-Velasco M, Dejong CHC, Neumann UP, Moser AJ, van Dam RM (2019) Systematic review of team performance in minimally invasive abdominal surgery. BJS Open 3:252–259. https://doi.org/10.1002/bjs5.50133
Acknowledgements
The authors received no financial support for the research and authorship of this article. The literature strategy was conducted in collaboration with an information specialist.
Funding
No funding was received to conduct this review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Jannie Lysgaard Poulsen, Birgitte Bruun, Doris Østergaard and Lene Spanager have no conflicts of interest and no financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Poulsen, J.L., Bruun, B., Oestergaard, D. et al. Factors affecting workflow in robot-assisted surgery: a scoping review. Surg Endosc 36, 8713–8725 (2022). https://doi.org/10.1007/s00464-022-09373-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09373-w