Abstract
Background
There is a lack of published data on variations in practices concerning laparoscopic cholecystectomy. The purpose of this study was to capture variations in practices on a range of preoperative, perioperative, and postoperative aspects of this procedure.
Methods
A 45-item electronic survey was designed to capture global variations in practices concerning laparoscopic cholecystectomy, and disseminated through professional surgical and training organisations and social media.
Results
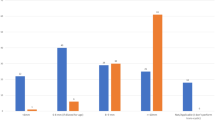
638 surgeons from 70 countries completed the survey. Pre-operatively only 5.6% routinely perform an endoscopy to rule out peptic ulcer disease. In the presence of preoperatively diagnosed common bile duct (CBD) stones, 85.4% (n = 545) of the surgeons would recommend an Endoscopic Retrograde Cholangio-Pancreatography (ERCP) before surgery, while only 10.8% (n = 69) of the surgeons would perform a CBD exploration with cholecystectomy. In patients presenting with gallstone pancreatitis, 61.2% (n = 389) of the surgeons perform cholecystectomy during the same admission once pancreatitis has settled down. Approximately, 57% (n = 363) would always administer prophylactic antibiotics and 70% (n = 444) do not routinely use pharmacological DVT prophylaxis preoperatively.
Open juxta umbilical is the preferred method of pneumoperitoneum for most patients used by 64.6% of surgeons (n = 410) but in patients with advanced obesity (BMI > 35 kg/m2, only 42% (n = 268) would use this technique and only 32% (n = 203) would use this technique if the patient has had a previous laparotomy. Most surgeons (57.7%; n = 369) prefer blunt ports. Liga clips and Hem-o-loks® were used by 66% (n = 419) and 30% (n = 186) surgeons respectively for controlling cystic duct and (n = 477) 75% and (n = 125) 20% respectively for controlling cystic artery. Almost all (97.4%) surgeons felt it was important or very important to remove stones from Hartmann’s pouch if the surgeon is unable to perform a total cholecystectomy.
Conclusions
This study highlights significant variations in practices concerning various aspects of laparoscopic cholecystectomy.

Similar content being viewed by others
Data availability
The data used to support the findings of this study can be released upon request.
References
Reynolds W Jr (2001) The first laparoscopic cholecystectomy. JSLS 5:89–94
Hasbahceci M (2016) Laparoscopic cholecystectomy: what has changed over the last three decades? Clin Surg 1:1166
National Institute for Health and Care Excellence, Health and Social Care Directorate (2015) Quality Standards and Indicators Briefing Paper. https://www.nice.org.uk/guidance/qs104/documents/gallstone-disease-qs-briefing-paper2 Last Accessed 25/07/2021.
Macano C, Griffiths EA, Vohra RS (2017) Current practice of antibiotic prophylaxis during elective laparoscopic cholecystectomy. Ann R Coll Surg Engl. https://doi.org/10.1308/rcsann.2017.0001
Donnellan E, Coulter J, Mathew C, Choynowski M, Flanagan L, Bucholc M, Johnston A, Sugrue M (2020) A meta-analysis of the use of intraoperative cholangiography; time to revisit our approach to cholecystectomy? Surg Open Sci. https://doi.org/10.1016/j.sopen.2020.07.004
McIntyre C, Johnston A, Foley D, Lawler J, Bucholc M, Flanagan L, Sugrue M (2020) Readmission to hospital following laparoscopic cholecystectomy: a meta-analysis. Anaesthesiol Intensive Ther. https://doi.org/10.5114/ait.2020.92967
Omar I, Hafez A (2021) Readmissions after cholecystectomy in a tertiary UK centre: incidence, causes and burden. J Minim Access Surg. https://doi.org/10.4103/jmas.JMAS_296_20
Adil MT, Aminian A, Bhasker AG, Rajan R, Corcelles R, Zerrweck C, Graham Y, Mahawar K (2020) Perioperative practices concerning sleeve gastrectomy—a survey of 863 surgeons with a cumulative experience of 520,230 procedures. Obes Surg. https://doi.org/10.1007/s11695-019-04195-7
Rosado EG, Olivella G, Natal-Albelo EJ, Echegaray GJ, Rivera LL, Guevara CA, Alejandro LM, Martínez-Rivera A, Ramírez N, Foy CA (2020) Practice variation among Hispanic American orthopedic surgeons in the management of geriatric distal radius fracture. Geriatr Orthop Surg Rehabil. https://doi.org/10.1177/2151459320969378
Garg SK, Bazerbachi F, Sarvepalli S, Majumder S, Vege SS (2019) Why are we performing fewer cholecystectomies for mild acute biliary pancreatitis? Trends and predictors of cholecystectomy from the National Readmissions Database (2010–2014). Gastroenterol Report. https://doi.org/10.1093/gastro/goz037
Davoodabadi A, Beigmohammadi E, Gilasi H, Arj A, Taheri Nassaj H (2020) Optimising cholecystectomy time in moderate acute biliary pancreatitis: a randomised clinical trial study. Heliyon. https://doi.org/10.1016/j.heliyon.2020.e03388
Takahashi N, Umemura A, Suto T, Fujiwara H, Ariyoshi Y, Nitta H, Takahara T, Hasegawa Y, Sasaki A (2021) Aggressive laparoscopic cholecystectomy in accordance with the Tokyo guideline 2018. JSLS. https://doi.org/10.4293/JSLS.2020.00116
Blohm M, Österberg J, Sandblom G, Lundell L, Hedberg M, Enochsson L (2016) The sooner, the better? The importance of optimal timing of cholecystectomy in acute cholecystitis: data from the national Swedish registry for gallstone surgery, GallRiks (2017). J Gastrointest Surg. https://doi.org/10.1007/s11605-016-3223-y
Okamoto K, Suzuki K, Takada T, Strasberg SM, Asbun HJ, Endo I, Iwashita Y, Hibi T, Pitt HA, Umezawa A, Asai K, Han HS, Hwang TL, Mori Y, Yoon YS, Huang WS, Belli G, Dervenis C, Yokoe M, Kiriyama S, Itoi T, Jagannath P, Garden OJ, Miura F, Nakamura M, Horiguchi A, Wakabayashi G, Cherqui D, de Santibañes E, Shikata S, Noguchi Y, Ukai T, Higuchi R, Wada K, Honda G, Supe AN, Yoshida M, Mayumi T, Gouma DJ, Deziel DJ, Liau KH, Chen MF, Shibao K, Liu KH, Su CH, Chan ACW, Yoon DS, Choi IS, Jonas E, Chen XP, Fan ST, Ker CG, Giménez ME, Kitano S, Inomata M, Hirata K, Inui K, Sumiyama Y, Yamamoto M (2018) Tokyo Guidelines 2018: flowchart for the management of acute cholecystitis. J Hepatobiliary Pancreat Sci. https://doi.org/10.1002/jhbp.516
AUGIS (2013). Commissioning guide: Gallstone disease. Available from: https://www.augis.org/wp content/uploads/2014/05/ Gallstone disease commissioning guide for REPUBLICATION 1. pdf. (Last Accessed 2021 3 July).
Yokoe M, Hata J, Takada T, Strasberg SM, Asbun HJ, Wakabayashi G, Kozaka K, Endo I, Deziel DJ, Miura F, Okamoto K, Hwang TL, Huang WS, Ker CG, Chen MF, Han HS, Yoon YS, Choi IS, Yoon DS, Noguchi Y, Shikata S, Ukai T, Higuchi R, Gabata T, Mori Y, Iwashita Y, Hibi T, Jagannath P, Jonas E, Liau KH, Dervenis C, Gouma DJ, Cherqui D, Belli G, Garden OJ, Giménez ME, de Santibañes E, Suzuki K, Umezawa A, Supe AN, Pitt HA, Singh H, Chan ACW, Lau WY, Teoh AYB, Honda G, Sugioka A, Asai K, Gomi H, Itoi T, Kiriyama S, Yoshida M, Mayumi T, Matsumura N, Tokumura H, Kitano S, Hirata K, Inui K, Sumiyama Y, Yamamoto M. Tokyo Guidelines (2018) Diagnostic criteria and severity grading of acute cholecystitis (with videos) (2018). J Hepatobiliary Pancreat Sci. https://doi.org/10.1002/jhbp.515
Kunnuru SKR, Kanmaniyan B, Thiyagarajan M, Singh BK, Navrathan N (2021) A study on Efficacy of UGI Scopy in Cholelithiasis patients before laparoscopic cholecystectomy. Minim Invasive Surg. https://doi.org/10.1155/2021/8849032
Kang KA, Kwon HJ, Ham SY, Park HJ, Shin JH, Lee SR, Kim MS (2020) Impacts on outcomes and management of preoperative magnetic resonance cholangiopancreatography in patients scheduled for laparoscopic cholecystectomy: for whom it should be considered? Ann Surg Treat Res. https://doi.org/10.4174/astr.2020.99.4.221
Gao MJ, Jiang ZL (2021) Effects of the timing of laparoscopic cholecystectomy after endoscopic retrograde cholangiopancreatography on liver, bile, and inflammatory indices and cholecysto-choledocholithiasis patient prognoses. Clinics (Sao Paulo). https://doi.org/10.6061/clinics/2021/e2189
Wang CC, Tsai MC, Wang YT, Yang TW, Chen HY, Sung WW, Huang SM, Tseng MH, Lin CC (2019) Role of cholecystectomy in choledocholithiasis patients underwent endoscopic retrograde cholangiopancreatography. Sci Rep. https://doi.org/10.1038/s41598-018-38428-z
Abdalkoddus M, Franklyn J, Ibrahim R, Yao L, Zainudin N, Aroori S (2021) Delayed cholecystectomy following endoscopic retrograde cholangio-pancreatography is not associated with worse surgical outcomes. Surg Endosc. https://doi.org/10.1007/s00464-021-08593-w
Xu J, Yang C (2020) Cholecystectomy outcomes after endoscopic sphincterotomy in patients with choledocholithiasis: a meta-analysis. BMC Gastroenterol. https://doi.org/10.1186/s12876-020-01376-y
Zhong FP, Wang K, Tan XQ, Nie J, Huang WF, Wang XF (2019) The optimal timing of laparoscopic cholecystectomy in patients with mild gallstone pancreatitis: a meta-analysis. Medicine (Baltimore). https://doi.org/10.1097/MD.0000000000017429
Milosevic M, Plecko V, Kalenic S, Fiolic Z, Vanek M (2013) Surveillance of surgical site infection after cholecystectomy using the hospital in Europe link for infection control through surveillance protocol. Surg Infect (Larchmt). https://doi.org/10.1089/sur.2012.096
Warren DK, Nickel KB, Wallace AE, Mines D, Tian F, Symons WJ, Fraser VJ, Olsen MA (2017) Risk factors for surgical site infection after cholecystectomy. Open Forum Infect Dis. https://doi.org/10.1093/ofid/ofx036
Yang JD, Yu HC (2021) Prospective control study of clinical effectiveness of prophylactic antibiotics in laparoscopic cholecystectomy on infection rate. Yonsei Med J. https://doi.org/10.3349/ymj.2021.62.2.172
Vohra RS, Hodson J, Pasquali S, Griffiths EA, CholeS study group, West Midlands research collaborative (2017) Effectiveness of antibiotic prophylaxis in non-emergency cholecystectomy using data from a population-based cohort study. World J Surg. https://doi.org/10.1007/s00268-017-4018-3
Pasquali S, Boal M, Griffiths EA, Alderson D, Vohra RS, CholeS Study Group, West Midlands Research Collaborative (2015) Meta-analysis of perioperative antibiotics in patients undergoing laparoscopic cholecystectomy. Br J Surg. https://doi.org/10.1002/bjs.9904
Jaafar G, Sandblom G, Lundell L, Hammarqvist F (2020) Antibiotic prophylaxis in acute cholecystectomy revisited: results of a double-blind randomised controlled trial. Langenbecks Arch Surg. https://doi.org/10.1007/s00423-020-01977-x
Chen CH, Lin CL, Kao CH (2020) The risk of venous thromboembolism in patients with gallstones. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph17082930
National Institute for Health and Care Excellence (2018). Venous thromboembolism in over 16s: reducing the risk of hospital-acquired deep vein thrombosis or pulmonary embolism. Available from: https://www.nice.org.uk/guidance/ng89/resources/venous-thromboembolism-in-over-16s-reducing-the-risk-of-hospitalacquired-deep-vein-thrombosis-or-pulmonary-embolism-pdf-1837703092165 Last Accessed 03/08/2021. Last Accessed 03/08/2021
Katar MK, Ersoy PE (2021) Is previous upper abdominal surgery a contraindication for laparoscopic cholecystectomy? Cureus. https://doi.org/10.7759/cureus.14272
Abounozha S, Alshahri T, Alammari S, Ibrahim R (2021) Clipless laparoscopic cholecystectomy is a better technique in reducing intraoperative bleeding. Ann Med Surg (Lond). https://doi.org/10.1016/j.amsu.2021.01.039
Abounozha S, Ibrahim R, Alshahri T (2021) Is the rate of bile leak higher in clipless laparoscopic cholecystectomy compared to conventional cholecystectomy? Ann Med Surg (Lond). https://doi.org/10.1016/j.amsu.2021.01.038
de’Angelis N, Catena F, Memeo R, Coccolini F, Martínez-Pérez A, Romeo OM, De Simone B, Di Saverio S, Brustia R, Rhaiem R, Piardi T, Conticchio M, Marchegiani F, Beghdadi N, Abu-Zidan FM, Alikhanov R, Allard MA, Allievi N, Amaddeo G, Ansaloni L, Andersson R, Andolfi E, Azfar M, Bala M, Benkabbou A, Ben-Ishay O, Bianchi G, Biffl WL, Brunetti F, Carra MC, Casanova D, Celentano V, Ceresoli M, Chiara O, Cimbanassi S, Bini R, Coimbra R, Luigi de’Angelis G, Decembrino F, De Palma A, de Reuver PR, Domingo C, Cotsoglou C, Ferrero A, Fraga GP, Gaiani F, Gheza F, Gurrado A, Harrison E, Henriquez A, Hofmeyr S, Iadarola R, Kashuk JL, Kianmanesh R, Kirkpatrick AW, Kluger Y, Landi F, Langella S, Lapointe R, Le Roy B, Luciani A, Machado F, Maggi U, Maier RV, Mefire AC, Hiramatsu K, Ordoñez C, Patrizi F, Planells M, Peitzman AB, Pekolj J, Perdigao F, Pereira BM, Pessaux P, Pisano M, Puyana JC, Rizoli S, Portigliotti L, Romito R, Sakakushev B, Sanei B, Scatton O, Serradilla-Martin M, Schneck AS, Sissoko ML, Sobhani I, Ten Broek RP, Testini M, Valinas R, Veloudis G, Vitali GC, Weber D, Zorcolo L, Giuliante F, Gavriilidis P, Fuks D, Sommacale D (2021) 2020 WSES guidelines for the detection and management of bile duct injury during cholecystectomy. World J Emerg Surg. https://doi.org/10.1186/s13017-021-00369-w
Brunt LM, Deziel DJ, Telem DA, Strasberg SM, Aggarwal R, Asbun H, Bonjer J, McDonald M, Alseidi A, Ujiki M, Riall TS, Hammill C, Moulton CA, Pucher PH, Parks RW, Ansari MT, Connor S, Dirks RC, Anderson B, Altieri MS, Tsamalaidze L, Stefanidis D, and the Prevention of Bile Duct Injury Consensus Work Group (2020) Safe cholecystectomy multi-society practice guideline and state of the art consensus conference on prevention of bile duct injury during cholecystectomy. Ann Surg. https://doi.org/10.1097/SLA.0000000000003791
Michael Brunt L, Deziel DJ, Telem DA, Strasberg SM, Aggarwal R, Asbun H, Bonjer J, McDonald M, Alseidi A, Ujiki M, Riall TS, Hammill C, Moulton CA, Pucher PH, Parks RW, Ansari MT, Connor S, Dirks RC, Anderson B, Altieri MS, Tsamalaidze L, Stefanidis D, Prevention of Bile Duct Injury Consensus Work Group (2020) Safe cholecystectomy multi-society practice guideline and state-of-the-art consensus conference on prevention of bile duct injury during cholecystectomy. Surg Endosc. https://doi.org/10.1007/s00464-020-07568-7
La Regina D, Mongelli F, Cafarotti S, Saporito A, Ceppi M, Di Giuseppe M, di Tor F, Vajana A (2018) Use of retrieval bag in the prevention of wound infection in elective laparoscopic cholecystectomy: is it evidence-based? A meta-analysis. BMC Surg. https://doi.org/10.1186/s12893-018-0442-z,19Nov
Hajibandeh S, Hajibandeh S, Clark MC, Barratt OA, Taktak S, Subar D, Henley N (2019) Retrieval of gallbladder via umbilical versus epigastric port site during laparoscopic cholecystectomy: a systematic review and meta-analysis. Surg Laparosc Endosc Percutan Tech. https://doi.org/10.1097/SLE.0000000000000662.PMID:31033631
Gelman D, Gelmanas A, Urbanaitė D, Tamošiūnas R, Sadauskas S, Bilskienė D, Naudžiūnas A, Širvinskas E, Benetis R, Macas A (2018) Role of multimodal analgesia in the evolving enhanced recovery after surgery pathways. Medicina. https://doi.org/10.3390/medicina54020020
Omar I, Abualsel A (2019) Efficacy of Intraperitoneal instillation of bupivacaine after bariatric surgery: randomized controlled trial. Obes Surg. https://doi.org/10.1007/s11695-019-03775-x
Liang M, Chen Y, Zhu W, Zhou D (2020) Efficacy and safety of different doses of ropivacaine for laparoscopy-assisted infiltration analgesia in patients undergoing laparoscopic cholecystectomy: a prospective randomised control trial. Medicine. https://doi.org/10.1097/MD.0000000000022540
Vijayaraghavalu S, Bharthi Sekar E (2021) A Comparative study on the postoperative analgesic effects of the intraperitoneal instillation of bupivacaine versus normal saline following laparoscopic cholecystectomy. Cureus. https://doi.org/10.7759/cureus.14151
Yang J, Liu Y, Yan P, Tian H, Jing W, Si M, Yang K, Guo T (2020) Comparison of laparoscopic cholecystectomy with and without abdominal drainage in patients with non-complicated benign gallbladder disease: a protocol for systematic review and meta-analysis. Medicine (Baltimore). https://doi.org/10.1097/MD.0000000000020070
Chandio A, Khatoon Z, Chandio K, Naqvi SM, Naqvi SA (2017) Immediate outcome of day case laparoscopic cholecystectomy. Trends Transplant 2:2017. https://doi.org/10.15761/TiT.1000226
Acknowledgements
None
Funding
No funding was received for this project.
Author information
Authors and Affiliations
Contributions
MK and KB: Methodology, Investigation, Data Curation, Formal analysis, original draft preparation. IO: Formal analysis, Discussion of The Results and Literature Review, Writing—Review & Editing, Supervision. KM: Conceptualisation, Writing—Review & Editing, Supervision. MT: Conceptualisation, Writing—Review & Editing, Supervision. All authors have seen the final manuscript and approved it.
Corresponding author
Ethics declarations
Disclosures
Mr. Matta Kuzman, Mr. Khalid Munir Bhatti, Mr. Islam Omar, Mr. Hany Khalil, Dr. Wah Yang, Mr. Prem Thambi, Mr. Nader Helmy, Mr Amir Botros, Dr. Thomas Kidd, Ms. Siobhan McKay, Mr. Altaf Awan, Prof Mark Taylor, and Prof. Kamal Mahawar have declared no conflict of interest.
Informed consent
Informed Consent does not apply.
Institutional research committee approval number
No prior Institutional or ethical approval was deemed necessary for this type of survey.
Research involving human and/or animal rights
Not Applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kuzman, M., Bhatti, K.M., Omar, I. et al. Solve study: a study to capture global variations in practices concerning laparoscopic cholecystectomy. Surg Endosc 36, 9032–9045 (2022). https://doi.org/10.1007/s00464-022-09367-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09367-8