Abstract
Background
Laparoscopic surgery (LS) is reported to reduce postoperative complications and hospital stay compared with open surgery (OP). Because patient selection may have been biased in previous studies, propensity score matching (PSM) analysis was used in this study to test the benefits of LS compared with OP.
Methods
A total of 759 patients with stage I–III colorectal cancer undergoing curative surgery were retrospectively reviewed. To minimize confounding bias between LS and OP groups, a 1:1 PSM analysis was performed based on adjuvant chemotherapy, age, albumin, body mass index, American Society of Anesthesiologists physical status depth of tumor, gender, lymph node dissection, maximum tumor size, obstructive tumor, previous abdominal surgery, pathological stage, tumor differentiation, and tumor location. Statistical analyses including chi-square test, Mann–Whitney U test, univariate analyses and Kaplan–Meier method and log-rank test were performed using the data after PSM to investigate the benefits of LS compared with OP.
Results
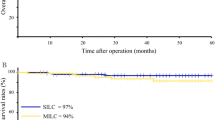
After PSM analysis, 460 patients remained in the study. The LS group had lower intraoperative blood loss (34 ± 70 vs 237 ± 391, mL; P < 0.001), lower frequency of postoperative small bowel obstruction (SBO) (17/213 vs 30/230; P = 0.045), lower rate of nasogastric tube insertion (7/223 vs 17/213; P = 0.036), and shorter postoperative hospital stay (13 ± 10 vs 25 ± 47, day; P < 0.001) than the OP group. Univariate analyses showed that LS significantly reduced the risk of postoperative SBO (odds ratio [OR] 0.532; 95% confidence interval [CI] 0.285–0.995; P = 0.048) and nasogastric tube insertion (OR 0.393; 95% CI 0.160–0.967; P = 0.042) compared with OP. There were no significant differences in OS and RFS between the groups.
Conclusions
LS reduced intraoperative blood loss, frequency of postoperative SBO, rate of nasogastric tube insertion, and postoperative hospital stay compared with OP.


Similar content being viewed by others
Change history
20 December 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00464-023-10648-z
Abbreviations
- ASA-PS:
-
American Society of Anesthesiologists physical status
- BMI:
-
Body mass index
- CRC:
-
Colorectal cancer
- LS:
-
Laparoscopic surgery
- OP:
-
Open surgery
- OS:
-
Overall survival
- PSM:
-
Propensity score matching
- SBO:
-
Small bowel obstruction
- RFS:
-
Recurrence-free survival
- ROC:
-
Receiver operating characteristic
References
Kuipers EJ, Grady WM, Lieberman D, Seufferlein T, Sung JJ, Boelens PG, van de Velde CJ, Watanabe T (2015) Colorectal cancer. Nat Rev Dis Primers 1:15065
Jacobs M, Verdeja JC, Goldstein HS (1991) Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc 1:144–150
Watanabe M, Ohgami M, Teramoto T, Kitajima M (1997) Laparoscopic local excision of the cecum for cecal creeping tumor. Surg Laparosc Endosc 7:144–147
Maggiori L, Panis Y (2013) Surgical management of IBD—from an open to a laparoscopic approach. Nat Rev Gastroenterol Hepatol 10:297–306
Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, Haglind E, Påhlman L, Cuesta MA, Msika S, Morino M, Lacy A, Bonjer HJ (2009) Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 10:44–52
Yamamoto S, Inomata M, Katayama H, Mizusawa J, Etoh T, Konishi F, Sugihara K, Watanabe M, Moriya Y, Kitano S (2014) Short-term surgical outcomes from a randomized controlled trial to evaluate laparoscopic and open D3 dissection for stage II/III colon cancer: Japan Clinical Oncology Group Study JCOG 0404. Ann Surg 260:23–30
Bonjer HJ, Deijen CL, Abis GA, Cuesta MA, van der Pas MH, de Lange-de Klerk ES, Lacy AM, Bemelman WA, Andersson J, Angenete E, Rosenberg J, Fuerst A, Haglind E (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 372:1324–1332
van der Pas MH, Haglind E, Cuesta MA, Fürst A, Lacy AM, Hop WC, Bonjer HJ (2013) Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol 14:210–218
Baiu I, Hawn MT (2018) Small bowel obstruction. JAMA 319:2146
Kazama K, Numata M, Aoyama T, Atsumi Y, Tamagawa H, Godai T, Saeki H, Saigusa Y, Shiozawa M, Yukawa N, Masuda M, Rino Y (2021) Does the Endoscopic Surgical Skill Qualification System improve patients’ outcome following laparoscopic surgery for colon cancer? A multicentre, retrospective analysis with propensity score matching. World J Surg Oncol 19:53
Egenvall M, Mörner M, Påhlman L, Gunnarsson U (2014) Degree of blood loss during surgery for rectal cancer: a population-based epidemiologic study of surgical complications and survival. Colorectal Dis 16:696–702
Story SK, Chamberlain RS (2009) A comprehensive review of evidence-based strategies to prevent and treat postoperative ileus. Dig Surg 26:265–275
Wichmann MW, Hüttl TP, Winter H, Spelsberg F, Angele MK, Heiss MM, Jauch KW (2005) Immunological effects of laparoscopic vs open colorectal surgery: a prospective clinical study. Arch Surg 140:692–697
Sammour T, Kahokehr A, Chan S, Booth RJ, Hill AG (2010) The humoral response after laparoscopic versus open colorectal surgery: a meta-analysis. J Surg Res 164:28–37
Saito S, Akagi T, Katayama H, Wakabayashi M, Inomata M, Yamamoto S, Ito M, Kinugasa Y, Egi H, Munakata Y, Kokuba Y, Bando H, Yasui M, Ikeda M, Nakajima K, Shida D, Kanemitsu Y, Kitano S (2021) Identification of patient subgroups with unfavorable long-term outcomes associated with laparoscopic surgery in a randomized controlled trial comparing open and laparoscopic surgery for colon cancer (Japan Clinical Oncology Group Study JCOG0404). Ann Gastroenterol Surg 5:804–812
Hayashi H, Ozaki N, Ogawa K, Ikuta Y, Tanaka H, Ogata K, Doi K, Takamori H (2018) Assessing the economic advantage of laparoscopic vs. open approaches for colorectal cancer by a propensity score matching analysis. Surg Today 48:439–448
Gehrman J, Angenete E, Björholt I, Lesén E, Haglind E (2020) Cost-effectiveness analysis of laparoscopic and open surgery in routine Swedish care for colorectal cancer. Surg Endosc 34:4403–4412
Maassen van den Brink M, Tweed TTT, de Hoogt PA, Hoofwijk AGM, Hulsewé KWE, Sosef MN, Stoot JHMB (2021) The introduction of laparoscopic colorectal surgery: can it improve hospital economics? Dig Surg 38:58–65
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not for profit sectors.
Author information
Authors and Affiliations
Contributions
KS wrote the manuscript. TS was corresponding author, revised the manuscript, performed statistical analyses and planed the study design. The authors wish to thank MI, TA and KK for their advice on the study design. In addition, the authors would like to thank the timely help given by SM, MN, NS, HH, TM, TS, YS, SM, YI and KT in collecting the large amount of patients’ data.
Corresponding author
Ethics declarations
Disclosures
Kotaro Suda, Takayuki Shimizu, Mitsuru Ishizuka, Shotaro Miyashita, Maiko Niki, Norisuke Shibuya, Hiroyuki Hachiya, Takatsugu Matsumoto, Takayuki Shiraki, Yuhki Sakuraoka, Shozo Mori, Yukihiro Iso, Kazutoshi Takagi, Taku Aoki, Keiichi Kubota have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Suda, K., Shimizu, T., Ishizuka, M. et al. Laparoscopic surgery reduced frequency of postoperative small bowel obstruction, and hospital stay compared with open surgery in a cohort of patients with colorectal cancer: a propensity score matching analysis. Surg Endosc 36, 8790–8796 (2022). https://doi.org/10.1007/s00464-022-09302-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09302-x