Abstract
Background
The adoption of minimally invasive pancreatoduodenectomy (MIPD) has increased over the last decade. Most of the data on perioperative and oncological outcomes derives from single-center high-volume hospitals. The impact of MIPD on oncological outcomes in a multicenter setting is poorly understood.
Methods
The National Cancer Database was utilized to perform a propensity score matching analysis between MIPD vs open pancreatoduodenectomy (OPD). The primary outcomes were lymphadenectomy ≥ 15 nodes and surgical margins. Secondary outcomes were 90-day mortality, length of stay, and overall survival.
Results
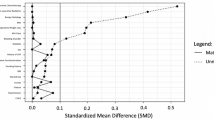
A total of 10,246 patients underwent pancreatoduodenectomy for ductal adenocarcinoma between 2010 and 2016. Among these patients, 1739 underwent MIPD. A propensity score matching analysis with a 1:2 ratio showed that the rate of lymphadenectomy ≥ 15 nodes was significantly higher for MIPD compared to OPD, 68.4% vs 62.5% (P < .0001), respectively. There was no statistically significant difference in the rate of positive margins, 90-day mortality, and overall survival. OPD was associated with an increased rate of length of stay > 10 days, 36.6% vs 33% for MIPD (P < .01). Trend analysis for the patients who underwent MIPD revealed that the rate of adequate lymphadenectomy increased during the study period, 73.1% between 2015 and 2016 vs 63.2% between 2010 and 2012 (P < .001). In addition, the rate of conversion to OPD decreased over time, 29.3% between 2010 and 2012 vs 20.2% between 2015 and 2016 (P < .001).
Conclusion
In this propensity score matching analysis, the MIPD approach was associated with a higher rate of adequate lymphadenectomy and a shorter length of stay compared to OPD. The surgical margins status, 90-day mortality, and overall survival were similar between the groups.

Similar content being viewed by others
References
Cameron JL, Riall TS, Coleman J, Belcher KA (2006) One thousand consecutive pancreaticoduodenectomies. Ann Surg 244(1):10–15
Tol JA, Gouma DJ, Bassi C, Dervenis C, Montorsi M, Adham M et al (2014) Definition of a standard lymphadenectomy in surgery for pancreatic ductal adenocarcinoma: a consensus statement by the International Study Group on Pancreatic Surgery (ISGPS). Surgery 156(3):591–600
Sood A, Meyer CP, Abdollah F, Sammon JD, Sun M, Lipsitz SR et al (2017) Minimally invasive surgery and its impact on 30-day postoperative complications, unplanned readmissions and mortality. Br J Surg 104(10):1372–1381
Xu T, Hutfless SM, Cooper MA, Zhou M, Massie AB, Makary MA (2015) Hospital cost implications of increased use of minimally invasive surgery. JAMA Surg 150(5):489–490
Spampinato MG, Coratti A, Bianco L, Caniglia F, Laurenzi A, Puleo F et al (2014) Perioperative outcomes of laparoscopic and robot-assisted major hepatectomies: an Italian multi-institutional comparative study. Surg Endosc 28(10):2973–2979
Wright GP, Zureikat AH (2016) Development of minimally invasive pancreatic surgery: an evidence-based systematic review of laparoscopic versus robotic approaches. J Gastrointest Surg Off J Soc Surg Aliment Tract 20(9):1658–1665
Zureikat AH, Borrebach J, Pitt HA, McGill D, Hogg ME, Thompson V et al (2017) Minimally invasive hepatopancreatobiliary surgery in North America: an ACS-NSQIP analysis of predictors of conversion for laparoscopic and robotic pancreatectomy and hepatectomy. HPB (Oxford) 19(7):595–602
Venkat R, Edil BH, Schulick RD, Lidor AO, Makary MA, Wolfgang CL (2012) Laparoscopic distal pancreatectomy is associated with significantly less overall morbidity compared to the open technique: a systematic review and meta-analysis. Ann Surg 255(6):1048–1059
Sun R, Yu J, Zhang Y, Liang Z, Han X (2021) Perioperative and oncological outcomes following minimally invasive versus open pancreaticoduodenectomy for pancreatic duct adenocarcinoma. Surg Endosc 35(5):2273–2285
van Hilst J, de Rooij T, Klompmaker S, Rawashdeh M, Aleotti F, Al-Sarireh B et al (2019) Minimally invasive versus open distal pancreatectomy for ductal adenocarcinoma (DIPLOMA): a pan-european propensity score matched study. Ann Surg 269(1):10–17
Palanivelu C, Senthilnathan P, Sabnis SC, Babu NS, SrivatsanGurumurthy S, AnandVijai N et al (2017) Randomized clinical trial of laparoscopic versus open pancreatoduodenectomy for periampullary tumours. Br J Surg 104(11):1443–1450
Poves I, Burdío F, Morató O, Iglesias M, Radosevic A, Ilzarbe L et al (2018) Comparison of perioperative outcomes between laparoscopic and open approach for pancreatoduodenectomy: the PADULAP randomized controlled trial. Ann Surg 268(5):731–739
van Hilst J, de Rooij T, Bosscha K, Brinkman DJ, van Dieren S, Dijkgraaf MG et al (2019) Laparoscopic versus open pancreatoduodenectomy for pancreatic or periampullary tumours (LEOPARD-2): a multicentre, patient-blinded, randomised controlled phase 2/3 trial. Lancet Gastroenterol Hepatol 4(3):199–207
Asbun HJ, Moekotte AL, Vissers FL, Kunzler F, Cipriani F, Alseidi A et al (2020) The Miami international evidence-based guidelines on minimally invasive pancreas resection. Ann Surg 271(1):1–14
Gooiker GA, Lemmens VE, Besselink MG, Busch OR, Bonsing BA, Molenaar IQ et al (2014) Impact of centralization of pancreatic cancer surgery on resection rates and survival. Br J Surg 101(8):1000–1005
Sheetz KH, Nuliyalu U, Nathan H, Sonnenday CJ (2020) Association of surgeon case numbers of pancreaticoduodenectomies vs related procedures with patient outcomes to inform volume-based credentialing. JAMA Netw Open 3(4):e203850
Stuart EA, King G, Imai K, Ho D (2011) MatchIt: nonparametric preprocessing for parametric causal inference. J Stat Softw. https://doi.org/10.18637/jss.v042.i08
Adam MA, Choudhury K, Dinan MA, Reed SD, Scheri RP, Blazer DG III et al (2015) Minimally invasive versus open pancreaticoduodenectomy for cancer: practice patterns and short-term outcomes among 7061 patients. Ann Surg 262(2):372–377
Dokmak S, Ftériche FS, Aussilhou B, Bensafta Y, Lévy P, Ruszniewski P et al (2015) Laparoscopic pancreaticoduodenectomy should not be routine for resection of periampullary tumors. J Am Coll Surg 220(5):831–838
van Hilst J, de Rooij T, Abu Hilal M, Asbun HJ, Barkun J, Boggi U et al (2017) Worldwide survey on opinions and use of minimally invasive pancreatic resection. HPB (Oxford) 19(3):190–204
Zureikat AH, Beane JD, Zenati MS, Al Abbas AI, Boone BA, Moser AJ et al (2021) 500 Minimally invasive robotic pancreatoduodenectomies: one decade of optimizing performance. Ann Surg 273(5):966–972
Hata T, Motoi F, Ishida M, Naitoh T, Katayose Y, Egawa S et al (2016) Effect of hospital volume on surgical outcomes after pancreaticoduodenectomy: a systematic review and meta-analysis. Ann Surg 263(4):664–672
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Yazan Ashouri, Katherine Ho, Helen Ho, Chiu-Hsieh Hsu, Iman Ghaderi, Ioannis Konstantinidis, and Felipe Maegawa have no conflicts of interest or financial ties to disclose. Dr. Taylor Riall and her husband have a diversified stock portfolio in Fidelity; owning publicly traded stock in the following companies: Apple, Abbvie, Abbott Laboratories, Amgen, Advansix, Caterpillar, Colgate Palmolive, Canadian National, Railway, Cisco Systems, Cintas Group, Facebook, General Mills, Garret Motion, Healthcare Services, Home Depot, Honeywell, IBM, Intel, Johnson and Johnson, Lockheed Martin, McDonalds, Medtronic, McCormick, 3 M, Merck, Microsoft, Nike, Pepsico, Pfizer, Parker Hannifan, Raytheon, Sherwin Williams, AT&T, United Health Group, Union Pacific, Viatris, Verizon, Walmart, Xlinx. They also have over $5000 in holdings in all but Facebook, Garrett Motion, Healthcare Services, Nike, Viatris. None of Dr. Riall’s stocks are related to this study and other research she has done.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ashouri, Y., Ho, K., Ho, H. et al. Minimally invasive vs open pancreatoduodenectomy on oncological adequacy: a propensity score-matched analysis. Surg Endosc 36, 7302–7311 (2022). https://doi.org/10.1007/s00464-022-09111-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09111-2