Abstract
Background
Obesity is a risk factor for cholelithiasis. Besides, rapid weight loss after bariatric surgery upsurges the rate of cholelithiasis and acute cholecystitis. This study aimed to compare gallstone development frequency after LSG under ursodeoxycholic acid (UDCA) prophylaxis.
Methods
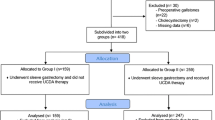
This prospective controlled study included 332 patients scheduled for LSG randomized to receive 500 mg UDCA daily for 12 months (UDCA Group) or no treatment (Control Group). Ultrasonography was done 6 and 12 months after surgery to detect gallstones. Cholecystectomy was done for complicated cases of cholelithiasis.
Results
Seventy-one patients were lost to follow-up, and 3 developed severe adverse effects of UDCA and excluded. Data are presented for 130 patients in the UDCA group and 128 in the Control group. Collectively, 11 patients (8.5%) of the UDCA group and 41 (32.0%) of the Control group developed gall stones during the first postoperative year (p < 0.001). Cholecystectomy was indicated in 3 patients (2.3%) of the UDCA group and 9 (7.0%) of the Control group (p = 0.072). On multivariate analysis, higher BMI, dyslipidemia, and lacking UDCA prophylaxis were the independent factors significantly associated with stone development. Also, stone development was associated with higher weight loss after 6 and 12 months.
Conclusion
UDCA 500 mg once daily for 12 months after LSG is effective in reducing gallstone formation at 1 year. UDCA administration reduced the frequency of cholecystectomies from 7 to 2.3%. High BMI and dyslipidemia are the independent preoperative factors significantly associated with stone development.


Similar content being viewed by others
References
Afshin A et al (2017) Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med 377:13–27
Scherer PE, Hill JA (2016) Obesity, diabetes, and cardiovascular diseases: a compendium. Circ Res 118:1703–1705
Stender S, Nordestgaard BG, Tybjaerg-Hansen A (2013) Elevated body mass index as a causal risk factor for symptomatic gallstone disease: a Mendelian randomization study. Hepatology 58:2133–2141
Iglézias Brandão de Oliveira C, Adami Chaim E, da Silva BB. Impact of rapid weight reduction on risk of cholelithiasis after bariatric surgery. Obes Surg. 2003;13:625–8.
Dittrick GW, Thompson JS, Campos D, Bremers D, Sudan D (2005) Gallbladder pathology in morbid obesity. Obes Surg 15:238–242
Welbourn R, Hollyman M, Kinsman R, Dixon J, Liem R, Ottosson J et al (2019) Bariatric surgery worldwide: baseline demographic description and one-year outcomes from the fourth IFSO Global Registry report 2018. Obes Surg 29:782–795
Erlinger S (2000) Gallstones in obesity and weight loss. Eur J Gastroenterol Hepatol 12:1347–1352
Tapas M, Kona Kumari L, Kiran Kumar P (2016) Prevalence of cholelithiasis and choledocholithiasis in morbidly obese South Indian patients and the further development of biliary calculus disease after sleeve gastrectomy, gastric bypass and mini gastric bypass. Obes Surg 26:2411–2417
Coupaye M, Castel B, Sami O, Tuyeras G, Msika S, Ledoux S (2015) Comparison of the incidence of cholelithiasis after sleeve gastrectomy and Roux-en-Y gastric bypass in obese patients: a prospective study. Surg Obes Relat Dis 11:779–784
Manatsathit W, Leelasinjaroen P, Al-Hamid H, Szpunar S, Hawasli A (2016) The incidence of cholelithiasis after sleeve gastrectomy and its association with weight loss: a two-centre retrospective cohort study. Int J Surg 30:13–18
Plecka Östlund M, Wenger U, Mattsson F, Ebrahim F, Botha A, Lagergren J (2012) Population-based study of the need for cholecystectomy after obesity surgery. Br J Surg 99:864–869
Nguyen NT, Hinojosa MW, Slone J, Lee J, Khiatani V, Wilson SE (2007) Laparoscopic transgastric access to the biliary tree after Roux-en-Y gastric bypass. OBES SURG 17:416–419
Hussain A, El-Hasani S (2016) Potential benefits of prophylactic cholecystectomy in patients undergoing bariatric bypass surgery. Obes Surg 26:865–865
Worni M, Guller U, Shah A, Gandhi M, Shah J, Rajgor D et al (2012) Cholecystectomy concomitant with laparoscopic gastric bypass: a trend analysis of the nationwide inpatient sample from 2001 to 2008. Obes Surg 22:220–229
Magouliotis DE, Tasiopoulou VS, Svokos AA, Svokos KA, Chatedaki C, Sioka E et al (2017) Ursodeoxycholic acid in the prevention of gallstone formation after bariatric surgery: an updated systematic review and meta-analysis. Obes Surg 27:3021–3030
Portincasa P, Moschetta A, Palasciano G (2006) Cholesterol gallstone disease. The Lancet 368:230–239
Tsai C-J (2006) Weight cycling and risk of gallstone disease in men. Arch Intern Med 166:2369
Yi S-Q, Ohta T, Tsuchida A, Terayama H, Naito M, Li J et al (2007) Surgical anatomy of innervation of the gallbladder in humans and Suncus murinus with special reference to morphological understanding of gallstone formation after gastrectomy. World J Gastroenterol 13:2066–2071
Tustumi F, Bernardo WM, Santo MA, Cecconello I (2018) Cholecystectomy in patients submitted to bariatric procedure: a systematic review and meta-analysis. Obes Surg 28:3312–3320
Mechanick JI, Youdim A, Jones DB, Garvey WT, Hurley DL, McMahon M et al (2013) Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Obesity (Silver Spring) 21:S1-27
Obésité : prise en charge chirurgicale chez l’adulte [Internet]. Haute Autorité de Santé. https://www.has-sante.fr/jcms/c_765529/fr/obesite-prise-en-charge-chirurgicale-chez-l-adulte. Accessed 7 Jun 2021
Machado FHF, de Castro HF, de Babadopulos RF, Rocha HAL, da Costa M, de Rocha JL et al (2019) Ursodeoxycholic acid in the prevention of gallstones in patients subjected to Roux-en-Y gastric bypass1. Acta Cir Bras 34(1):e20190010000009
Paumgartner G, Beuers U (2004) Mechanisms of action and therapeutic efficacy of ursodeoxycholic acid in cholestatic liver disease. Clin Liver Dis 8(67–81):vi
Lee JM, Hyun JJ, Choi IY, Yeom SK, Kim SY, Jung SW et al (2015) Comparison on response and dissolution rates between ursodeoxycholic acid alone or in combination with chenodeoxycholic acid for gallstone dissolution according to stone density on CT scan: strobe compliant observation study. Medicine (Baltimore) 94(50):e2037
May GR, Sutherland LR, Shaffer EA (1993) Efficacy of bile acid therapy for gallstone dissolution: a meta-analysis of randomized trials. Aliment Pharmacol Ther 7:139–148
Lazaridis KN, Gores GJ, Lindor KD (2001) Ursodeoxycholic acid “mechanisms of action and clinical use in hepatobiliary disorders.” J Hepatol 35:134–146
Adams LB, Chang C, Pope J, Kim Y, Liu P, Yates A (2016) Randomized, prospective comparison of ursodeoxycholic acid for the prevention of gallstones after sleeve gastrectomy. Obes Surg 26:990–994
Abdallah E, Emile SH, Elfeki H, Fikry M, Abdelshafy M, Elshobaky A et al (2017) Role of ursodeoxycholic acid in the prevention of gallstone formation after laparoscopic sleeve gastrectomy. Surg Today 47:844–850
Coupaye M, Calabrese D, Sami O, Siauve N, Ledoux S (2019) Effectiveness of ursodeoxycholic acid in the prevention of cholelithiasis after sleeve gastrectomy. Obes Surg 29:2464–2469
Şen O, Türkçapar AG, Yerdel MA (2020) Cholelithiasis after sleeve gastrectomy and effectiveness of ursodeoxycholic acid treatment. J Laparoendosc Adv Surg Tech A 30:1150–1152
Nabil TM, Khalil AH, Gamal K (2019) Effect of oral ursodeoxycholic acid on cholelithiasis following laparoscopic sleeve gastrectomy for morbid obesity. Surg Obes Relat Dis 15:827–831
Sioka E, Zacharoulis D, Zachari E, Papamargaritis D, Pinaka O, Katsogridaki G et al (2014) Complicated gallstones after laparoscopic sleeve gastrectomy. J Obes 2014:468203
Moon RC, Teixeira AF, DuCoin C, Varnadore S, Jawad MA (2014) Comparison of cholecystectomy cases after Roux-en-Y gastric bypass, sleeve gastrectomy, and gastric banding. Surg Obes Relat Dis 10:64–68
Tsirline VB, Keilani ZM, El Djouzi S, Phillips RC, Kuwada TS, Gersin K et al (2014) How frequently and when do patients undergo cholecystectomy after bariatric surgery? Surg Obes Relat Dis 10:313–321
Dakour Aridi H, Sultanem S, Abtar H, Safadi BY, Fawal H, Alami RS (2016) Management of gallbladder disease after sleeve gastrectomy in a selected Lebanese population. Surg Obes Relat Dis 12:1300–1304
Guzmán HM, Sepúlveda M, Rosso N, San Martin A, Guzmán F, Guzmán HC (2019) Incidence and risk factors for cholelithiasis after bariatric surgery. Obes Surg 29:2110–2114
Miller K, Hell E, Lang B, Lengauer E (2003) Gallstone formation prophylaxis after gastric restrictive procedures for weight loss. Ann Surg 238:697–702
Li VKM, Pulido N, Martinez-Suartez P, Fajnwaks P, Jin HY, Szomstein S et al (2009) Symptomatic gallstones after sleeve gastrectomy. Surg Endosc 23:2488–2492
Melmer A, Sturm W, Kuhnert B, Engl-Prosch J, Ress C, Tschoner A et al (2015) Incidence of gallstone formation and cholecystectomy 10 years after bariatric surgery. Obes Surg 25:1171–1176
Deitel M, Petrov I (1987) Incidence of symptomatic gallstones after bariatric operations. Surg Gynecol Obstet 164:549–552
Amaral JF, Thompson WR (1985) Gallbladder disease in the morbidly obese. Am J Surg 149:551–557
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Mohamed AbdAlla Salman, Ahmed Salman, Usama Shaker Mohamedm Ahmed Mahmoud Hussein, Mahmoud A. Ameen, Hitham S.E. Omar, Ahmed Elewa, Ahmed hamdy, Abd Al-Kareem Elias, Mohamed Tourky, Alaa Helal, Ahmed Abdelrahman Mahmoud, Feras Aljarad, Ahmed Moustafa, Hossam El-Din Shaaban, Ahmed Nashat, Amr Mahmoud Hussein, Tamer Omar, and Hany Balamoun have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Salman, M.A., Salman, A., Mohamed, U.S. et al. Ursodeoxycholic acid for the prevention of gall stones after laparoscopic sleeve gastrectomy: a prospective controlled study. Surg Endosc 36, 6396–6402 (2022). https://doi.org/10.1007/s00464-021-08980-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08980-3