Abstract
Background
Topical pharyngeal anesthesia has improved esophagogastroduodenoscopy (EGD) efficiency with smooth insertion, reducing pain and discomfort. Lidocaine spray is one of the safe and widely used methods. In practice, the patients walk, sit in a wheelchair, or lie on a trolley bed, and the lidocaine sprays are applied to those in sitting or supine positions for pre-endoscopic preparation. Although there is no current guidance technique, this study aims to compare the effects of lidocaine sprays between sitting (Group A; Gp A) and supine positions (Group B; Gp B) for patients undergoing unsedated EGD.
Methods
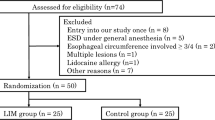
This study was a single-center prospective randomized controlled trial. Unsedated EGD patients were randomly allocated the lidocaine spray in sitting or lidocaine spray in the supine position.
Results
Lidocaine spray treatments were significantly different in the gag reflex (NRS; Gp A: 1.28 ± 0.67, Gp B: 1 ± 0.63, p = 0.0003), ease of esophageal instrumentation (NRS; Gp A: 7.68 ± 0.91, Gp B: 7.95 ± 0.66, p = 0.0042), and pain score (NRS; Gp A: 5.16 ± 2.08, Gp B: 4.53 ± 1.93, p = 0.0059). When considering modified Mallampati classification (MMC), MMC classes III and IV were significantly different in the same direction but MMC classes I and II were not.
Conclusion
The technique of spraying in the supine position was associated with less gagging, less pain, and easier esophageal instrumentation, especially in patients with MMC classes III and IV.


Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.
References
Teh JL, Shabbir A, Yuen S, So JB (2020) Recent advances in diagnostic upper endoscopy. World J Gastroenterol 26(4):433–447
Yamamoto Y, Yahagi N, Yamamoto H, Ono H, Inoue H (2020) Innovative therapeutic endoscopy in the upper gastrointestinal tract: a review of the JGES core sessions. Dig Endosc 32:882–887
Chang KJ (2019) Endoscopic foregut surgery and interventions: the future is now. The state-of-the-art and my personal journey. World J Gastroenterol 25(1):1–41
Carey EJ, Sorbi D (2004) Unsedated endoscopy. Gastrointest Endosc Clin N Am 14(2):369–383
Sorbi D, Chak A (2003) Unsedated EGD. Gastrointest Endosc 58(1):102–110
Hagan KB, Thirumurthi S, Gottumukkala R, Vargo J (2016) Sedation in the endoscopy suite. Curr Treat Options Gastroenterol 14(2):194–209
Sidhu R, Turnbull D, Newton M et al (2019) Deep sedation and anaesthesia in complex gastrointestinal endoscopy: a joint position statement endorsed by the British Society of Gastroenterology (BSG), Joint Advisory Group (JAG) and Royal College of Anaesthetists (RCoA). Frontline Gastroenterol 10(2):141–147
Leslie K, Allen ML, Hessian E, Lee AY (2016) Survey of anaesthetists’ practice of sedation for gastrointestinal endoscopy. Anaesth Intensive Care 44(4):491–497
Cohen LB, Wecsler JS, Gaetano JN et al (2006) Endoscopic sedation in the United States: results from a nationwide survey. Am J Gastroenterol 101(5):967–974
Ristikankare M, Julkunen R, Heikkinen M et al (2006) Sedation, topical pharyngeal anesthesia and cardiorespiratory safety during gastroscopy. J Clin Gastroenterol 40(10):899–905
Heuss LT, Hanhart A, Dell-Kuster S et al (2011) Propofol sedation alone or in combination with pharyngeal lidocaine anesthesia for routine upper GI endoscopy: a randomized, double-blind, placebo-controlled, non-inferiority trial. Gastrointest Endosc 74(6):1207–1214
Ullman DA, Saleem SA, Shahnawaz A, Kotakanda S, Scribani MB, Victory JM (2019) Relation of viscous lidocaine combined with propofol deep sedation during elective upper gastrointestinal endoscopy to discharge. Proc (Bayl Univ Med Cent) 32(4):505–509
Watanabe J, Ikegami Y, Tsuda A et al (2021) Lidocaine spray versus viscous lidocaine solution for pharyngeal local anesthesia in upper gastrointestinal endoscopy: Systematic review and meta-analysis. Dig Endosc 33(4):538–548
Hayashi T, Asahina Y, Waseda Y et al (2017) Lidocaine spray alone is similar to spray plus viscous solution for pharyngeal observation during transoral endoscopy: a clinical randomized trial. Endosc Int Open 5(1):E47–E53
Amornyotin S, Srikureja W, Chalayonnavin W, Kongphlay S, Chatchawankitkul S (2009) Topical viscous lidocaine solution versus lidocaine spray for pharyngeal anesthesia in unsedated esophagogastroduodenoscopy. Endoscopy 41(7):581–586
Chan CK, Fok KL, Poon CM (2010) Flavored anesthetic lozenge versus Xylocaine spray used as topical pharyngeal anesthesia for unsedated esophagogastroduodenoscopy: a randomized placebo-controlled trial. Surg Endosc 24(4):897–901
Mogensen S, Treldal C, Feldager E et al (2012) New lidocaine lozenge as topical anesthesia compared to lidocaine viscous oral solution before upper gastrointestinal endoscopy. Local Reg Anesth 5:17–22
Ayoub C, Skoury A, Abdul-Baki H, Nasr V, Soweid A (2007) Lidocaine lollipop as single-agent anesthesia in upper GI endoscopy. Gastrointest Endosc 66(4):786–793
Mahawongkajit P, Talalak N, Soonthornkes N (2021) Comparison of lidocaine spray and lidocaine ice popsicle in patients undergoing unsedated esophagogastroduodenoscopy: a single center prospective randomized controlled trial. Clin Exp Gastroenterol 14:209–216
Noitasaeng P, Vichitvejpaisal P, Kaosombatwattana U, Tassanee J, Suwannee S (2016) Comparison of spraying and nebulized lidocaine in patients undergoing esophago-gastro-duodenoscopy: a randomized trial. J Med Assoc Thai 99(5):462–468
Kollmann CM, Schmiegel W, Brechmann T (2018) Gastrointestinal endoscopy under sedation is associated with pneumonia in older inpatients-results of a retrospective case-control study. United Eur Gastroenterol J 6(3):382–390
Jirapinyo P, Thompson CC (2016) Sedation challenges: obesity and sleep apnea. Gastrointest Endosc Clin N Am 26(3):527–537
Sharma VK, Nguyen CC, Crowell MD, Lieberman DA, de Garmo P, Fleischer DE (2007) A national study of cardiopulmonary unplanned events after GI endoscopy. Gastrointest Endosc 66(1):27–34
Repici A, Hassan C (2017) The endoscopist, the anesthesiologists, and safety in GI endoscopy. Gastrointest Endosc 85(1):109–111
Amornyotin S (2013) Sedation-related complications in gastrointestinal endoscopy. World J Gastrointest Endosc 5(11):527–533
Abraham NS, Fallone CA, Mayrand S, Huang J, Wieczorek P, Barkun AN (2004) Sedation versus no sedation in the performance of diagnostic upper gastrointestinal endoscopy: a Canadian randomized controlled cost-outcome study. Am J Gastroenterol 99(9):1692–1699
Amornyotin S, Lertakayamanee N, Wongyingsinn M, Pimukmanuskit P, Chalayonnavin V (2007) The effectiveness of intravenous sedation in diagnostic upper gastrointestinal endoscopy. J Med Assoc Thai 90(2):301–306
Chung DC, Mainland PA, Kong AS (1999) Anesthesia of the airway by aspiration of lidocaine. Can J Anaesth 46(3):215–219
van de Ven S, Bugter O, Hardillo JA, Bruno MJ, Baatenburg de Jong RJ, Koch AD. Screening for head and neck second primary tumors in patients with esophageal squamous cell cancer: A systematic review and meta-analysis. United European Gastroenterol J. 2019;7(10):1304–1311.
Morimoto H, Yano T, Yoda Y et al (2017) Clinical impact of surveillance for head and neck cancer in patients with esophageal squamous cell carcinoma. World J Gastroenterol 23(6):1051–1058
Kim DH, Gong EJ, Jung HY et al (2014) Clinical significance of intensive endoscopic screening for synchronous esophageal neoplasm in patients with head and neck squamous cell carcinoma. Scand J Gastroenterol 49(12):1486–1492
Acknowledgements
This work was supported by Research Group in Surgery, Faculty of Medicine, Thammasat University. Special thanks to Norman Mangnall for assistance in editing the English version of this paper and Dr. Saritphat Orrapin for scrutinizing methodology.
Funding
This research was supported in part by Thammasat University.
Author information
Authors and Affiliations
Contributions
All authors contributed to data analysis, drafting, and revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Disclosures
Dr. Prasit Mahawongkajit and Dr. Neranchala Soonthornkes have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mahawongkajit, P., Soonthornkes, N. Comparative effectiveness of lidocaine sprays between sitting and supine position for patients undergoing upper gastrointestinal endoscopy: a prospective randomized controlled trial. Surg Endosc 36, 5067–5075 (2022). https://doi.org/10.1007/s00464-021-08868-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08868-2