Abstract
Background
Recovery of preoperative ambulation levels 1 month after surgery represents an important patient-centered outcome. The objective of this study is to identify clinical factors associated with the inability to regain baseline preoperative ambulation levels 28 days postoperatively.
Methods
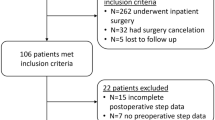
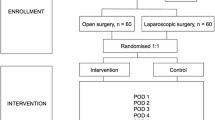
This is a prospective cohort study enrolling patients scheduled for elective inpatient abdominal operations. Daily ambulation (steps/day) was measured with a wristband accelerometer. Preoperative steps were recorded for at least 3 full calendar days before surgery. Postoperatively, daily steps were recorded for at least 28 days. The primary outcome was delayed recovery of ambulation, defined as inability to achieve 50% of preoperative baseline steps at 28 days postoperatively.
Results
A total of 108 patients were included. Delayed recovery (< 50% of baseline preoperative steps/day) occurred in 32 (30%) patients. Clinical factors associated with delayed recovery after multivariable logistic regression included longer operative time (OR 1.37, 95% CI 1.05–1.79), open operative approach (OR 4.87, 95% CI 1.64–14.48) and percent recovery on POD3 (OR 0.73, 95% CI 0.56–0.96). In addition, patients with delayed ambulation recovery had increased rates of postoperative complications (16% vs 1%, p < 0.01) and readmission (28% vs 5%, p < 0.01).
Conclusion
After elective inpatient abdominal operations, nearly one in three patients do not recover 50% of their baseline preoperative steps 28 days postoperatively. Factors that can be used to identify these patients include longer operations, open operations and low ambulation levels on postoperative day #3. These data can be used to target rehabilitation efforts aimed at patients at greatest risk for poor ambulatory recovery.


Similar content being viewed by others
References
Kluivers KB, Riphagen I, Vierhout ME, Brolmann HA, de Vet HC (2008) Systematic review on recovery specific quality-of-life instruments. Surgery 143(2):206–215
Paddison JS, Sammour T, Kahokehr A, Zargar-Shoshtari K, Hill AG (2011) Development and validation of the Surgical Recovery Scale (SRS). J Surg Res 167(2):e85-91
Appelboom G, Yang AH, Christophe BR et al (2014) The promise of wearable activity sensors to define patient recovery. J Clin Neurosci 21(7):1089–1093
Bassett DR Jr, Cureton AL, Ainsworth BE (2000) Measurement of daily walking distance-questionnaire versus pedometer. Med Sci Sports Exerc 32(5):1018–1023
Cook DJ, Thompson JE, Prinsen SK, Dearani JA, Deschamps C (2013) Functional recovery in the elderly after major surgery: assessment of mobility recovery using wireless technology. Ann Thorac Surg 96(3):1057–1061
Toogood PA, Abdel MP, Spear JA, Cook SM, Cook DJ, Taunton MJ (2016) The monitoring of activity at home after total hip arthroplasty. Bone Jt J 98-b(11):1450–1454
Sun V, Dumitra S, Ruel N et al (2017) Wireless monitoring program of patient-centered outcomes and recovery before and after major abdominal cancer surgery. JAMA Surg 152(9):852–859
Höchsmann C, Knaier R, Eymann J, Hintermann J, Infanger D, Schmidt-Trucksäss A (2018) Validity of activity trackers, smartphones, and phone applications to measure steps in various walking conditions. Scand J Med Sci Sports 28(7):1818–1827
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383
Borson S, Scanlan JM, Chen P, Ganguli M (2003) The Mini-Cog as a screen for dementia: validation in a population-based sample. J Am Geriatr Soc 51(10):1451–1454
Robinson TN, Wu DS, Pointer L, Dunn CL, Cleveland JC Jr, Moss M (2013) Simple frailty score predicts postoperative complications across surgical specialties. Am J Surg 206(4):544–550
Khuri SF, Daley J, Henderson W et al (1998) The Department of Veterans Affairs’ NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Ann Surg 228(4):491–507
R Core Team (2014) R:A language and environment for statistical Computing. R Found Stat Comput Vienna, Austria. http://wwwR-project.org/2014.
Callahan EH, Thomas DC, Goldhirsch SL, Leipzig RM (2002) Geriatric hospital medicine. Med Clin North Am 86(4):707–729
Lane AJ (1999) Evaluation of the fall prevention program in an acute care setting. Orthop Nurs 18(6):37–43
Lawrence VA, Hazuda HP, Cornell JE et al (2004) Functional independence after major abdominal surgery in the elderly. J Am Coll Surg 199(5):762–772
Carmichael H, Overbey DM, Hosokawa P et al (2019) Wearable technology—a pilot study to define “normal” postoperative recovery trajectories. J Surg Res 244:368–373. https://doi.org/10.1016/j.jss.2019.1006.1057
Funding
This work was funded by a 2018 grant from the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES).
Author information
Authors and Affiliations
Contributions
HC, DO and TR contributed to the research conception and design. HC, DO, CG, TJ, EJ and TR Contributed to acquisition of data. HC, PH, CG and TR completed all data analysis and complication of the data. AK, HC, PH, EJ, TJ and TR contributed to writing and critical revision of the article.
Corresponding author
Ethics declarations
Disclosures
Dr Heather Carmichael and Thomas Robinson received a 2018 SAGES Research Grant for this study. No study number was assigned. Drs Alexandra Kovar, Teresa Jones, Douglas Overbey and Edward Jones have no conflicts of interest or financial ties to disclose. Patrick Hosokawa and Christina Goode have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kovar, A., Carmichael, H., Jones, T.S. et al. Early identification of patients at risk for delayed recovery of ambulation after elective abdominal surgery. Surg Endosc 36, 4828–4833 (2022). https://doi.org/10.1007/s00464-021-08829-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08829-9