Abstract
Background and Aims
Simultaneous endoscopic submucosal dissection (ESD) is occasionally used in synchronous multiple gastric neoplastic lesions (SMGL). Therefore, we aim to evaluate the safety and efficacy of simultaneous ESD for SMGL compared with ESD for single lesions.
Methods
A total of 1058 patients who received ESD from November 2006 to September 2019 were retrospectively evaluated in this study, including 997 single gastric epithelial lesions treated by single ESD (unifocal group) and 125 SMGL from 61 patients treated by simultaneous ESD (multifocal group).
Results
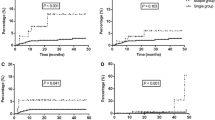
The mean procedure time was 49.2 ± 41.30 min and 89.5 ± 66.33 min in unifocal group and multifocal group, respectively (p < 0.001). There was no significant difference in postoperative stenosis rate (1.0% vs. 0.0%, p = 1.000), intraoperative bleeding (endoscopic resection bleeding-c3 grade) rate (0.5% vs. 1.6%, p = 0.696), postoperative bleeding rate (1.3% vs. 0.0%, p = 0.461), and perforation rate (0.9% vs. 1.6%, p = 0.449) between the two groups. In addition, en block resection rate (p = 0.825), complete resection rate (p = 0.856) and curative resection rate (p = 0.709) were comparable between the two groups. During the follow-up, the local recurrence rate per patient: p = 0.363; per lesion: p = 0.235) was not significantly different between the two groups, however, the cumulative incidence of metachronous lesions after treatment was significantly higher in the multifocal group than the other group (10.0% vs. 3.2%, p = 0.004).
Conclusions
Simultaneous ESD is safe and effective in the treatment of SMGL. However, separate ESD is recommended for SMGL with longer procedure time. Besides, the metachronous gastric neoplastic lesions should be paid attention to during follow-up.




Similar content being viewed by others
References
Meng FS, Zhang ZH, Wang YM, Lu L, Zhu JZ, Ji F (2016) Comparison of endoscopic resection and gastrectomy for the treatment of early gastric cancer: a meta-analysis. Surg Endosc 30:3673–3683
Ryu SJ, Kim BW, Kim BG, Kim JH, Kim JS, Kim JI, Park JM, Oh JH, Kim TH, Kim JJ, Park SM, Park CH, Song KY, Lee JH, Kim SG, Kim DJ, Kim W (2016) Endoscopic submucosal dissection versus surgical resection for early gastric cancer: a retrospective multicenter study on immediate and long-term outcome over 5 years. Surg Endosc 30:5283–5289
Si M, Muto M, Hamamoto Y, Boku N, Ohtsu A, Baba S, Yoshida M, Ohkuwa M, Hosokawa K, Tajiri H, Yoshida S (2002) A new technique for endoscopic mucosal resection with an insulated-tip electrosurgical knife improves the completeness of resection of intramucosal gastric neoplasms. Gastrointest Endosc 55:576–581
Zhao Y, Wang C (2018) Long-term clinical efficacy and perioperative safety of endoscopic submucosal dissection versus endoscopic mucosal resection for early gastric cancer: an updated meta-analysis. Biomed Res Int 2018:3152346
Moertel CG, Bargen J, Soule EH (1957) Multiple gastric cancers; review of the literature and study of 42 cases. Gastroenterology 32:1095–1103
Seo JH, Park JC, Kim YJ, Shin SK, Lee YC, Lee SK (2010) Undifferentiated histology after endoscopic resection may predict synchronous and metachronous occurrence of early gastric cancer. Digestion 81:35–42
Mi YJ, Jin WC, Wang GO, Ko SJ, Yong KC (2013) Clinicopathological characteristics of synchronous and metachronous gastric neoplasms after endoscopic submucosal dissection. Korean J Intern Med 28:687–693
Lim JH, Sang GK, Choi J, Im JP, Jung HC (2014) Risk factors for synchronous or metachronous tumor development after endoscopic resection of gastric neoplasms. Gastric Cancer 18:817–823
Joh DH, Park CH, Jung S, Choi SH, Kim HK, Lee H, Park JC, Shin SK, Lee YC, Lee SK (2015) Safety and feasibility of simultaneous endoscopic submucosal dissection for multiple gastric neoplasias. Surg Endosc 29:3690–3697
Choi J, Sang GK, Im JP, Kang SJ, Lee HJ, Yang HK, Kim JS, Kim WH, Jung HC, Song IS (2011) Lymph node metastasis in multiple synchronous early gastric cancer. Gastrointest Endosc 74:276–284
Kim HM, Kim HK, Sang KL, Cho JH, Youn YH (2011) Multifocality in early gastric cancer does not increase the risk of lymph node metastasis in a single-center study. Ann Surg Oncol 19:1251–1256
Isobe T, Hashimoto K, Kizaki J, Murakami N, Aoyagi K, Koufuji K, Akagi Y, Shirouzu K (2013) Characteristics and prognosis of synchronous multiple early gastric cancer. World J Gastroenterol 19(41):7154–7159
Kasuga A, Yamamoto Y, Fujisaki J, Okada K, Igarashi M (2012) Simultaneous endoscopic submucosal dissection for synchronous double early gastric cancer. Gastric Cancer 16:555–562
Chen ZS, Jin XF, Wu HL, Guo JQ (2017) Simultaneous endoscopic submucosal dissection for multiple early gastric cancers in a low volume center. Medicine (Baltimore) 96:e7745
Japanese Gastric Cancer Association (2011) Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer 14:101–112
The Paris endoscopic classification of superficial neoplastic lesions: esophagus, stomach, and colon: November 30 to December 1, 2002. Gastrointest Endosc 58(6 Suppl):S3–S43
Linghu EQ (2019) New classifications of intraoperative bleeding and muscularis propria injury in endoscopic resection. Chin Med J (Engl) 132(15):1856–1858
Yoo JH, Shin SJ, Lee KM, Choi JM, Wi JO, Kim DH, Lim SG, Hwang JC, Cheong JY, Yoo BM (2013) How can we predict the presence of missed synchronous lesions after endoscopic submucosal dissection for early gastric cancers or gastric adenomas? J Clin Gastroenterol 47:e17–e22
Nasu J, Doi T, Endo H, Nishina T, Hirasaki S, Hyodo I (2005) Characteristics of metachronous multiple early gastric cancers after endoscopic mucosal resection. Endoscopy 37(10):990–993
Ohta T, Ishihara R, Uedo N, Takeuchi Y, Nagai K, Matsui F, Kawada N, Yamashina T, Kanzaki H, Hanafusa M, Yamamoto S, Hanaoka N, Higashino K, Iishi H (2012) Factors predicting perforation during endoscopic submucosal dissection for gastric cancer. Gastrointest endosc 75:1159–1165
Toyokawa T, Inaba T, Omote S, Okamoto A, Miyasaka R, Watanabe K, Izumikawa K, Horii J, Fujita I, Ishikawa S, Morikawa T, Murakami T, Tomoda J (2012) Risk factors for perforation and delayed bleeding associated with endoscopic submucosal dissection for early gastric neoplasms: analysis of 1123 lesions. J Gastroenterol Hepatol 27:907–912
Chan HP, Kim H, Kang YA, Cho IR et al (2013) Risk factors and prognosis of pulmonary complications after endoscopic submucosal dissection for gastric neoplasia. Dig Dis Sci 58:540–546
Kim M, Jeon SW, Cho KB, Park KS, Kim ES, Park CK, Seo HE, Chung YJ, Kwon JG, Jung JT, Kim EY, Jang BI, Lee SH, Kim KO, Yang CH (2013) Predictive risk factors of perforation in gastric endoscopic submucosal dissection for early gastric cancer: a large, multicenter study. Surg Endosc 27:1372–1378
Ono H, Yao K, Fujishiro M, Oda I, Nimura S, Yahagi N, Iishi H, Oka M, Ajioka Y, Ichinose M, Matsui T (2016) Guidelines for endoscopic submucosal dissection and endoscopic mucosal resection for early gastric cancer. Dig Endosc 28:3–15
Yoo JH, Shin SJ, Lee KM, Choi JM, Wi JO, Kim DH, Lim SG, Hwang JC, Cheong JY, Yoo BM, Lee KJ, Kim JH, Cho SW (2012) Risk factors for perforations associated with endoscopic submucosal dissection in gastric lesions: emphasis on perforation type. Surg Endosc 26:2456–2464
Ding X, Luo H, Duan H (2019) Risk factors for perforation of gastric endoscopic submucosal dissection: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol 31:1481–1488
Watari J, Tomita T, Toyoshima F, Sakurai J, Kondo T, Asano H, Yamasaki T, Okugawa T, Ikehara H, Oshima T, Fukui H, Miwa H (2013) Clinical outcomes and risk factors for perforation in gastric endoscopic submucosal dissection: a prospective pilot study. World J Gastrointest Endosc 5:281–287
Akintoye E, Obaitan I, Muthusamy A, Akanbi O, Olusunmade M, Levine D (2016) Endoscopic submucosal dissection of gastric tumors: a systematic review and meta-analysis. World J Gastrointest Endosc 8:517–532
Park SE, Kim DH, Jung HY, Lim H, Ahn JY, Choi KS, Lee JH, Choi KD, Song HJ, Lee GH, Kim JH, Han S (2016) Risk factors and correlations of immediate, early delayed, and late delayed bleeding associated with endoscopic resection for gastric neoplasms. Surg Endosc 30:625–632
Jeon SW, Jung MK, Cho CM, Tak WY, Kweon YO, Kim SK, Choi YH (2009) Predictors of immediate bleeding during endoscopic submucosal dissection in gastric lesions. Surg Endosc 23:1974–1979
Nakajima T, Oda I, Gotoda T, Hamanaka H, Eguchi T, Yokoi C, Saito D (2006) Metachronous gastric cancers after endoscopic resection: how effective is annual endoscopic surveillance? Gastric Cancer 9:93–98
Han JS, Jang JS, Choi SR, Kwon HC, Kim MC, Jeong JS, Kim SJ, Sohn YJ, Lee EJ (2011) A study of metachronous cancer after endoscopic resection of early gastric cancer. Scand J Gastroenterol 46:1099–1104
Moon HS, Yun GY, Kim JS, Eun HS, Kang SH, Sung JK, Jeong HY, Song KS (2017) Risk factors for metachronous gastric carcinoma development after endoscopic resection of gastric dysplasia: Retrospective, single-center study. World J Gastroenterol 23:4407–4415
Arima N, Adachi K, Katsube T, Amano K, Kinoshita Y (1999) Predictive factors for metachronous recurrence of early gastric cancer after endoscopic treatment. J Clin Gastroenterol 29:44–47
Okada K, Suzuki S, Naito S, Yamada Y, Haruki S, Kubota M, Nakajima Y, Shimizu T, Ando K, Uchida Y, Hirasawa T, Fujisaki J, Tsuchida T (2019) Incidence of metachronous gastric cancer in patients whose primary gastric neoplasms were discovered after Helicobacter pylori eradication. Gastrointest Endosc 89:1152-1159.e1
Funding
The present study was supported by grants from National Key R&D Program of China (No. 2016YFC1303601).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Shanshan Xu, Ningli Chai, Xiaowei Tang, Enqiang Linghu, Zhongsheng Lu, Shasha Wang, and Bao Li have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xu, S., Chai, N., Tang, X. et al. Outcomes of simultaneous endoscopic submucosal dissection for synchronous multiple gastric neoplastic lesions: a retrospective comparative study. Surg Endosc 36, 4014–4024 (2022). https://doi.org/10.1007/s00464-021-08722-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08722-5